Key Takeaways
- Peripheral arterial disease (PAD) is common among older adults, particularly those over 65.
- It occurs when blood vessels narrow or when cholesterol or fatty material accumulates inside your arteries.
- Optimal sleeping positions for people with PAD include sleeping on the back with legs slightly elevated or sleeping on the left side with a pillow between your legs.
- Follow your doctor’s advice on medications and lifestyle changes to help manage PAD symptoms.
What Is Peripheral Artery Disease?
Peripheral artery disease (PAD) is a condition caused by the narrowing of the peripheral arteries (blood vessels that carry blood away from the heart to other parts of the body).
It is a progressive disease and a manifestation of atherosclerosis.
This results in reduced blood flow to the limbs, particularly the legs and feet.
PAD is primarily of two types:
- Lower-extremity PAD: This is the most common type, in which blood flow is reduced to the legs and feet.
- Upper-extremity PAD: This form of PAD impacts the arms, hands, and fingers and is less common (affects less than 10% of the population).
The signs and symptoms of PAD are often mistaken for other conditions, like arthritis in the hip, ankle, or foot.
This increases the individual’s risk for coronary artery disease, heart attacks, and stroke.
If left untreated, PAD can result in gangrene and amputation of the affected limbs.
Why Does Sleeping Position Matter for Peripheral Artery Disease?
PAD does not directly cause sleep problems.
However, people with PAD may experience:
- Leg pain at night
- Rest pain in advanced disease
- Cramping
- Coexisting sleep apnea
In advanced PAD, pain may worsen when the legs are elevated and improve when the legs hang down. This is due to gravity-assisted blood flow.
Further, nocturnal rest pain may occur due to reduced arterial perfusion at rest.
Because of this, body position may influence comfort, but high-quality trials comparing sleep positions in PAD are limited.
Most recommendations are based on clinical experience rather than randomized controlled trials.
| Expert picks: What To Read Next |
|---|
| What Is The Best Sleeping Position For Lower Back Pain? |
| What Are Some Simple Tests You Can Do To See If You’re Aging Well? |
What Is The Best Sleeping Position For Peripheral Artery Disease (PAD)?
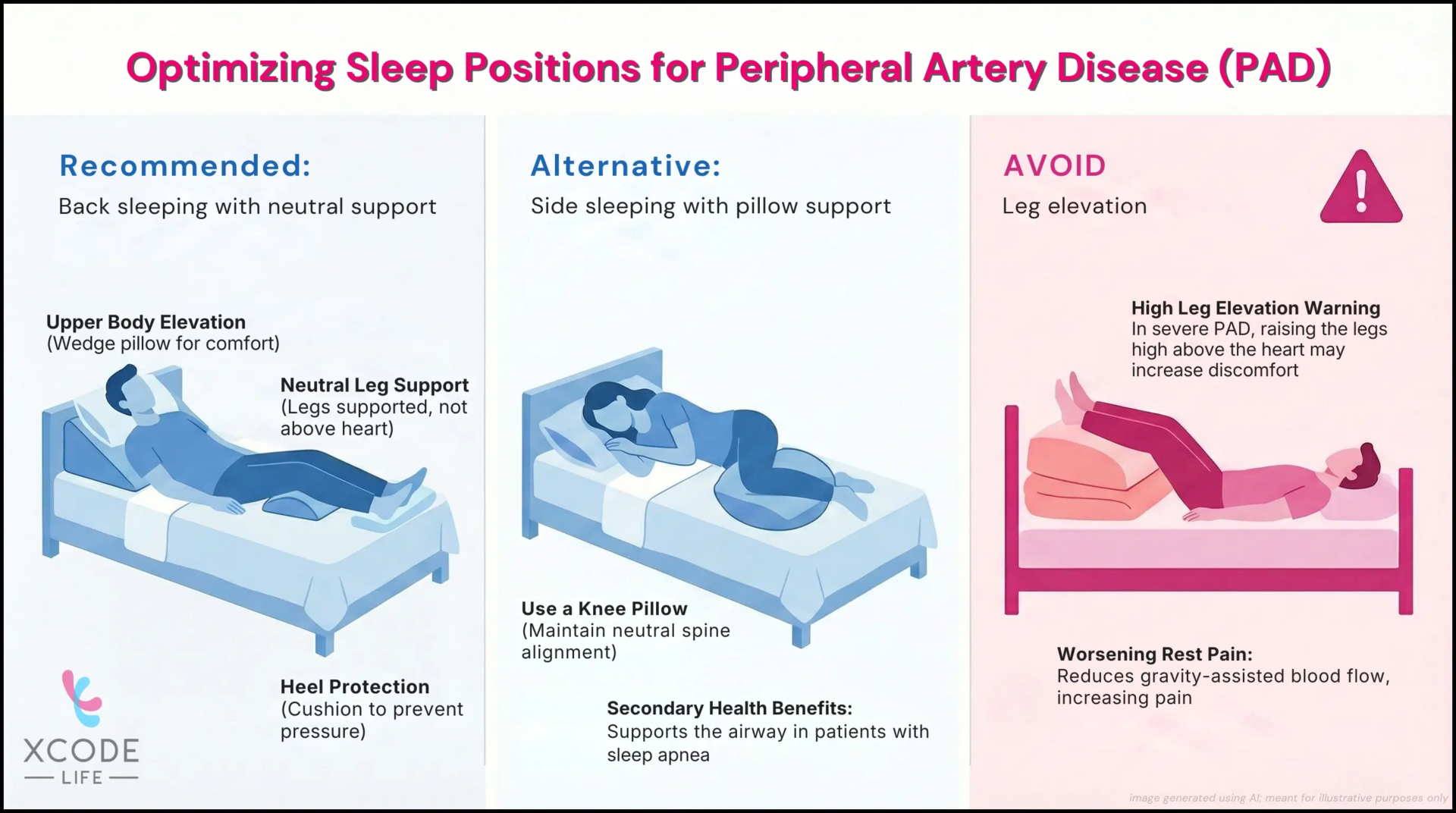
The most commonly recommended sleeping positions for peripheral artery disease (PAD) are:
- Lying on your back with the upper body slightly elevated and the legs supported at a neutral level
- Sleeping on your side with a pillow between the knees
These positions are generally suggested to reduce pressure points and improve comfort during the night.
However, in advanced PAD with rest pain, elevating the legs above heart level may worsen discomfort. Positioning should be adjusted based on symptom severity.
Side Sleeping With Pillow Between Knees
Sleeping on either side with a pillow between the knees may:
- Reduce hip and lower-back strain
- Improve overall comfort
- Support spinal alignment
There is no strong evidence that the left side specifically improves arterial circulation in PAD.
Side sleeping is often recommended for people who also have obstructive sleep apnea, as it may reduce airway collapse.
Sleeping On Back With Head Elevated
Some individuals report symptom relief when the head and upper body are slightly elevated.
This can be achieved using an adjustable bed or wedge pillow.
Importantly:
In people with advanced PAD and rest pain, keeping the legs flat or slightly dependent (not elevated above heart level) may reduce ischemic discomfort.
Elevating the legs above the heart, which is often recommended for venous disease, may worsen symptoms in arterial disease.
Sleep On Back With Heel Support
Sleeping on the back may be comfortable if:
- The heels are cushioned
- Pressure points are minimized
- The legs are not elevated excessively
At the same time, according to Dr. Trisha Roy, MD, Vascular Surgery at Houston Methodist, people with PAD benefit from sleeping positions that lift the pressure off their heels.
So, placing a cushion under the legs can help raise the heels off the bed and relieve pressure.
Best Sleep Position For Peripheral Artery Disease With Sleep Apnea
For people with PAD and sleep apnea, the optimal sleep position is one that provides airway support to minimize apnea episodes.
The recommended position for these individuals is sleeping on the left side as
- It reduces strain on lowr back
- Keeps the airways more open to lessen sleep apnea disruptions
Sleeping Positions To Avoid For Peripheral Artery Disease
- Sleeping on the stomach may increase neck or back strain. While it is not specifically linked to worsening PAD, discomfort from this position may disrupt sleep quality.
- Sleeping on the back with legs elevated can increase discomfort.
- Very tight curling of the legs (fetal position) may cause joint stiffness in some individuals, making it uncomfortable.
Other Evidence-based Ways to Manage PAD
Sleep position may influence comfort, but it does not treat the underlying disease.
Here are a few things you can do to manage PAD and improve your sleep:
Supervised Exercise Therapy (SET)
Supervised walking programs are one of the most evidence-supported interventions for intermittent claudication.
Guidelines recommend structured/supervised exercise as first-line therapy for many patients with symptomatic PAD.
In the CLEVER study (aortoiliac PAD), supervised exercise improved functional outcomes and quality of life compared with optimal medical care, with benefits comparable to stenting in some measures over follow-up.
How it’s typically done (high-level): walking intervals to moderate symptoms, rest, and repeat; usually several sessions per week for multiple weeks, under supervision.
Smoking Cessation (strongest modifiable risk factor)
Smoking is strongly associated with PAD development and progression, and quitting is consistently recommended in major cardiovascular guidelines as part of PAD risk reduction
Statin Therapy (Cardiovascular + Limb Outcome Benefit)
Because PAD is a form of atherosclerotic cardiovascular disease, lipid-lowering therapy is foundational.
Guidelines recommend statins for PAD to reduce cardiovascular events.
Meta-analyses in PAD populations also associate statin therapy (and often higher-intensity therapy) with better cardiovascular outcomes and improved limb-related outcomes.
Antiplatelet Therapy (Reduce Heart Attack and Stroke Risk)
Antiplatelet therapy is commonly used in symptomatic PAD to reduce major cardiovascular events.
The CAPRIE trial compared clopidogrel vs aspirin in patients with recent MI, ischemic stroke, or symptomatic PAD, and the PAD subgroup showed a greater relative benefit with clopidogrel than aspirin for major ischemic events.
Revascularization When Symptoms Persist, Despite Therapy
When symptoms remain limiting despite medical therapy and exercise, endovascular or surgical options may be considered in appropriate patients.
Guidelines discuss revascularization as an option based on anatomy, symptom severity, and response to conservative therapy.
Control Of Comorbid Risk Factors
PAD outcomes are strongly influenced by cardiovascular risk factors. Guideline-based management commonly includes:
- Blood pressure control
- Diabetes management
- Physical activity beyond structured programs
- Nutrition patterns that support lipid and blood pressure goals
These interventions support overall vascular risk reduction rather than producing immediate symptom relief.
Disclaimer
The management strategies discussed above are based on published clinical guidelines and research studies. They are intended for general educational purposes only.
Peripheral artery disease varies in severity between individuals. Treatment decisions depend on medical history, symptom pattern, diagnostic findings, and overall cardiovascular risk.
Exercise programs, medications, and revascularization procedures should be considered only under the guidance of a qualified healthcare professional.
This article does not replace medical evaluation, diagnosis, or individualized treatment planning.
If you experience worsening leg pain, rest pain, non-healing wounds, or sudden changes in symptoms, medical assessment is important.
Frequently Asked Questions
PAD in legs cannot typically be reversed.
Treatment for PAD focuses on reducing symptoms and preventing further progression of the condition.
Supervised walking programs are strongly recommended in PAD. Clinical trials show they improve walking distance and functional capacity.
You can choose socks made specifically for people with PAD.
These socks must be seamless or have smooth seams, with moisture-wicking properties, in merino wool or technical fibres.
Tight socks with rough seams may affect circulation and, therefore, are not suitable for people with PAD.
Leg elevation above heart level is generally recommended for venous disease, not arterial disease. In advanced PAD, elevation may worsen ischemic pain. Positioning should be individualized.
There is no clinically proven optimal sleep position for improving arterial blood flow. Comfort-focused positioning that does not worsen rest pain is typically advised.
Smoking is the most important modifiable risk factor for PAD and should be avoided.
It aggravates PAD symptoms and accelerates the progression of the disease. It also increases the risk for complications like heart attack and stroke.
Final Takeaway
- The most commonly recommended sleeping positions for peripheral artery disease (PAD) are lying on your back with the upper body slightly elevated and the legs supported at a neutral level, or sleeping on your side with a pillow between the knees.
- These positions are suggested to improve comfort and reduce pressure points during sleep.
- However, in advanced PAD with rest pain, elevating the legs above heart level may worsen discomfort. Positioning should be guided by symptom response rather than fixed rules.
- Sleep position does not treat arterial narrowing. Long-term management of PAD focuses on supervised exercise therapy, cardiovascular risk reduction, and appropriate medical care.
References
- https://www.ncbi.nlm.nih.gov/books/NBK279271/
- https://www.medicalnewstoday.com/articles/best-sleeping-position-for-peripheral-artery-disease
- https://www.goodrx.com/well-being/sleep/best-sleep-position-for-peripheral-artery-disease
- https://www.healthline.com/health/best-sleeping-position-for-peripheral-artery-disease
- https://my.clevelandclinic.org/health/diseases/17357-peripheral-artery-disease-pad
- https://www.heart.org/en/health-topics/peripheral-artery-disease/about-peripheral-artery-disease-pad
- https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0181733
- https://academic.oup.com/ehjopen/article-abstract/3/2/oead008/7068263
- https://www.nhlbi.nih.gov/health/sleep-apnea/treatment
- https://www.nhlbi.nih.gov/health/peripheral-artery-disease/treatment
- https://www.nhs.uk/conditions/peripheral-arterial-disease-pad/treatment/#:~:text=One%20of%20the%20best%20exercises,again%20until%20the%20pain%20returns.
- https://www.heart.org/en/health-topics/peripheral-artery-disease/why-pad-matters
- https://www.nhlbi.nih.gov/health/heart/smoking