There appears to be some truth to the age-old belief that body aches are a sign that bad weather is approaching. It’s more than just an anecdote! In fact, research suggests a relationship between pain levels and changes in weather, particularly in those suffering from chronic pain (like arthritis). So, what is the truth about rainy days and our health? Read on to find out whether body pain can be caused or worsen due to cold weather.
Did You Know? Your ancestry test DNA data includes 700,000 markers, which can be used to learn everything from disease risk and drug sensitivities to nutritional requirements and fitness parameters, even your pain tolerance. Learn more.
Historically, individuals suffering from chronic pain conditions like arthritis have often claimed that their symptoms intensify in cold weather.
Researchers have undertaken multiple studies to understand this link.
Some evidence suggests that a drop in temperature can lead to an increase in muscle stiffness and joint pain.
Although the reasons behind this aren't entirely clear-cut, the connection between body pain due to cold weather is hard to ignore.
Several theories explain the link between increased body pain and colder temperatures:
How Genes Influence Your Pain Tolerance?
Absolutely. People with chronic pain conditions or those who've had prior injuries might notice more pain during cold weather.
Older adults, with naturally reduced blood circulation and joint wear, may also experience an increase in pain symptoms.
Additionally, those who are more sensitive to changes in atmospheric pressure or have certain genetic predispositions might be more susceptible to body pain due to cold weather.
Several health conditions may see exacerbated symptoms in cold weather:
If you're susceptible to body pain due to cold weather, consider the following tips:
In conclusion, despite many reports of worsening body pain due to cold weather, the mechanism behind it is poorly understood.
Theories surrounding this point towards atmospheric pressure changes and blood vessel constriction during cold weather.
It is important to note that everyone experiences and manages pain differently. Therefore, it is important to sit down with your doctor to find a method of pain management that suits your body well.
Nonalcoholic fatty liver disease (NAFLD) is becoming a global threat in the healthcare industry, with more than a quarter of the world’s population affected.
Researchers now believe that certain gene variants could be encouraging the development of this condition.
Novel therapeutic treatment options targeting specific gene expressions could be the most effective way to handle NAFLD.
Read more about personalized treatment options for NAFLD and the different therapeutic treatments to look forward to in the future to handle fatty liver.
Genetic ancestry tests are becoming increasingly popular. While your DNA can be used to learn about your roots, did you know that it can also reveal important things about your health risks and wellness aspects? This allows you to take proactive measures for health conditions, even before the symptoms appear, thereby preventing it. You can upload your DNA data to learn 1,500+ things about your health. Learn more.
Nonalcoholic Fatty Liver Disease (NAFLD) affects a quarter of the global population.
NAFLD is the most commonly occurring liver disease worldwide.
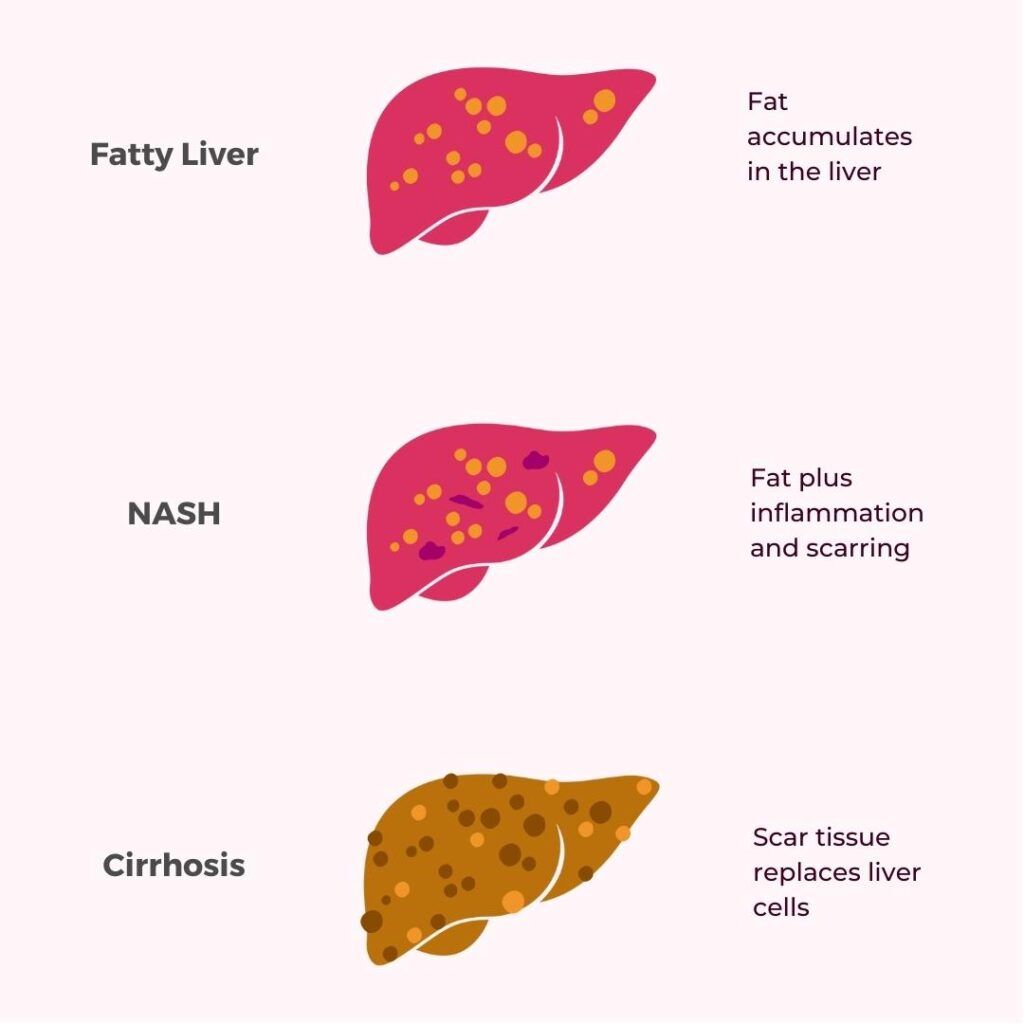
This condition can lead to liver damage and cirrhosis if left untreated.
While some of the common causes of NAFLD are lifestyle-related, researchers now believe that genetic factors also play an essential role in determining the rate of fat deposition and metabolism.
One important gene associated with NFALD is patatin-like phospholipase domain containing 3 (PNPLA3).
The patatin-like phospholipase domain containing 3 (PNPLA3) gene helps produce a protein named adiponutrin.
Adiponutrin is an essential component of hepatocytes (liver cells) and adipocytes (fat cells).
The complete role of adiponutrin is not well understood as of now.
However, researchers believe adiponutrin may play a role in fat production and breakdown.
It may also help develop adipocyte cells.
It has been noticed that during periods of fasting, the functioning of the PNPLA3 gene decreased.
PNPLA3 gene’s function increased after a meal.
This suggests that the PNPLA3 gene and the adiponutrin protein also play a role in fat metabolism and storage in the body.
NAFLD is a condition caused by excessive fat deposition in the liver.
NAFLD is characterized by high levels of serum LDL cholesterol and triglycerides and overweight.
The PNPLA3 gene breaks down triglycerides and other types of fats.
Studies report that mutations in this gene lead to a build-up of triglycerides in the liver.
This, over time, can lead to conditions like liver inflammation, NAFLD, liver cirrhosis, and even liver cancer.
The PNPLA3 gene is a lipid regulator in the liver cells.
In the liver cells, this gene helps break down triglycerides and convert polyunsaturated fatty acids into their intermediate form, called phosphocholines.
These processes are required to break down fat and eliminate it from the body.
Mutant forms of this gene can therefore affect fat breakdown in the liver and lead to fat accumulation instead.
A particular variant of the PNPLA3 gene was commonly found in those diagnosed with NAFLD.
People with this variant had problems in the regular production of the adiponutrin protein and could not break down fats in their bodies.
Researchers are now trying to target this gene and create therapeutic solutions for different liver diseases.
A 2021 study published by Cherubini and his team explores the idea of using the PNPLA3 as a therapeutic target for slowing down the progression of NAFLD.
According to this study, the PNPLA3 rs738409 C>G variant is the most commonly noted mutation in individuals with NAFLD.
This variant is associated with liver cirrhosis and inflammation and increases the risk of developing hepatocellular carcinoma (liver cancer) by up to 10 times.
The current generation of therapeutic treatments aims at targeting and disrupting specific protein expressions in the body to achieve favorable results.
Researchers are using liver-targeted Antisense Oligonucleotides (ASOs) as potential treatments for NAFLD.
ASO-based therapies use drugs that bind to the target RNA and modify protein expression through different mechanisms.
There are already preclinical trials conducted using liver-targeted ASOs.
These results report that the PNPLA3 ASO therapy effectively reduced the severity of Nonalcoholic Steatohepatitis (NASH) at all stages.
NASH is a more severe form of NAFLD.
The therapy was able to suppress the actions of the PNPLA3 148M protein successfully.
It helped reduce the intensity of liver inflammation, fibrosis, and fat accumulation.
The next step is the clinical trial, where the researchers would try and treat NASH patients with the PNPLA3 ASO therapy.
The research team hopes to deliver precision medicine to people with NASH using ASO therapy in less than ten years from now.
The team also emphasizes the need to understand the different variants of the PNPLA3 gene and other genes of interest to know how they would react to targeted therapy.
PXL770 is a novel therapeutic drug under investigation to treat NAFLD.
AMP Kinase (AMPK) is an energy sensor associated with lipid metabolism.
The PXL770 drug is a direct AMPK activator and could help people with NAFLD and type-2 diabetes handle their conditions better.
Between 2019 and 2020, a randomized, placebo-controlled, phase 2a study was conducted in 120 patients.
According to the researchers, AMPK activation definitely has the potential to become a pharmacology target in those with NAFLD.
PF-06835919 is a Ketohexokinase (KHK) inhibitor under investigation to treat NAFLD and NASH.
KHK is an enzyme that converts fructose into its next stage, fructose-1-phosphate.
High fructose consumption is one of the reasons for developing NAFLD.
Researchers conducted a randomized phase 2 trial in 2021 with 48 participants.
The research reports that KHK inhibition may be a potential pharmacological target in treating NFALD.
In 2021, an open-label phase II study was conducted to test the effectiveness of PX-104 against liver diseases.
PX-104 is a non-steroidal FXR agonist.
Four-week treatment with PX-104 lowered serum alanine aminotransferase (ALT) and γ-glutamyltransferase (GGT) levels.
These are markers pointing to liver diseases.
Researchers recommend further studies on this medicine to treat NAFLD and NASH.
https://www.mdpi.com/2077-0383/12/5/1852
https://pubmed.ncbi.nlm.nih.gov/34904923/
https://www.tandfonline.com/doi/full/10.1080/14728222.2021.2018418
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7262620/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6777808/
https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/pnpla3
https://www.frontiersin.org/articles/10.3389/fmed.2019.00304/full
https://medlineplus.gov/genetics/gene/pnpla3/
https://pubmed.ncbi.nlm.nih.gov/29935383/
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0132640
https://pubmed.ncbi.nlm.nih.gov/18820647/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7355792/
https://pubmed.ncbi.nlm.nih.gov/34560015/
https://pubmed.ncbi.nlm.nih.gov/35590219/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8116226/
Home DNA tests have become very popular because they are readily available and affordable.
Did you know that 1 in 5 Americans have already taken at least one DNA home test?
Taking a DNA test can be life-changing for many. That’s why it is critical to pick an accurate and trustworthy kit.
DNA tests are also called genetic tests. These analyze a person’s genes to identify mutations or changes in them.
These mutations can increase the person’s risk for various physical and mental health conditions and be the reason for specific actions and traits.
A person’s genes can also help identify their ancestry details, giving clarity on what their ethnicity could be.
At-home DNA tests don’t require the user to visit the lab or testing center to provide their DNA samples or get results. The samples are provided via mail, and the results are received by email.
The following are steps to take an at-home DNA test.
Medical DNA tests are also called clinical DNA tests. Here, healthcare professionals collect samples and run tests in a lab setting.
Most patients who undergo clinical DNA testing would have the opportunity to undergo genetic counseling. Some tests can tell if you may develop a certain health condition.
At-home DNA tests are done in a similar clinical setup. However, the samples for these are collected and sent by the individuals. If the samples are compromised, then the results can vary.
Home DNA tests also cannot definitively predict health conditions. They can only say if the person has certain gene changes that may increase the risk of certain diseases.
Finally, it is easy for individuals to misread reports and test results. So it would be best to talk to your healthcare provider before making any changes in lifestyle, medications, or diet based on your at-home DNA test reports.
Currently, at-home DNA tests cannot identify your risk for all diseases or traits and are limited to certain conditions. Even with the diseases they test for, they can only say whether or not you are at risk for developing them.
You may be the carrier of a mutated gene for diabetes but not develop it. Inversely, some disease-causing variants may not be identifiable with these tests, and you may still develop the condition.
You may need to get a clinical genetic test done for confirmation.
At-home DNA tests are also called Direct-To-Consumer tests. You must understand these tests to make full use of them.
At-home DNA tests have allowed people to explore their ancestry details, health and wellness traits, and carrier statuses.
These are affordable and, more importantly, can be done from the comforts of their home without needing an expert to prescribe them.
These tests can open up awareness about genetic diseases and offer recommendations regarding diet and lifestyle changes. The test reports can help you stay proactive and get yourself tested regularly if you are genetically inclined to develop certain health conditions.
If you are interested in knowing your ethnicity, these direct-to-consumer tests can give detailed ancestry details too. Many people find bloodlines on genomic websites using their family tree applications.
You have to know that such at-home DNA tests are still being researched. They may not offer you a complete picture of your health and wellness and may need to be followed up with clinical tests if you want more clarity.
At-home DNA tests offer you an overall health risk profile, which is great for someone whose family has had its share of genetic diseases in the past. It may be beneficial to know if you are at risk for developing inherited health conditions to take proactive steps.
These reports may also give a detailed list of possible allergens, from common ones like pollen to lesser-known ones like misophonia.
Mental health is a huge topic of interest now. Xcode Life’s mental health traits report may help you understand how your genes affect your feelings and thoughts.
Clinical DNA tests can be costly unless your healthcare provider approves and your insurance covers them.
For just $149, Xcode Life’s Premium Pack helps you explore 3000+ health and wellness traits in the following categories.
All you need is your raw DNA data. The company accepts raw data from most top genomic and ancestry companies. Once you upload the data, you can get results in less than a day.
This is a great package and offers value for money for individuals interested in knowing how their genes play a role in their physical and mental health and personalities.
At-home DNA tests are not as accurate as clinical genetic tests. However, if you are just trying to get started with DNA testing and there is no specific need for clinical tests, these at-home DNA tests are a great affordable start to exploring your genes and their effects on your life.
Know the limitations of home DNA tests and have practical expectations of the results.
Did you know one in eight Americans with prostate will be diagnosed with prostate cancer in their lifetimes? A majority of prostate cancer are silent and do not show any signs or symptoms in the initial stages. Screening tests have been widely recommended and performed to help in the early diagnosis of prostate cancers. However, what if an individual is at risk of prostate cancer due to their family history? Let’s learn whether prostate cancer is hereditary.
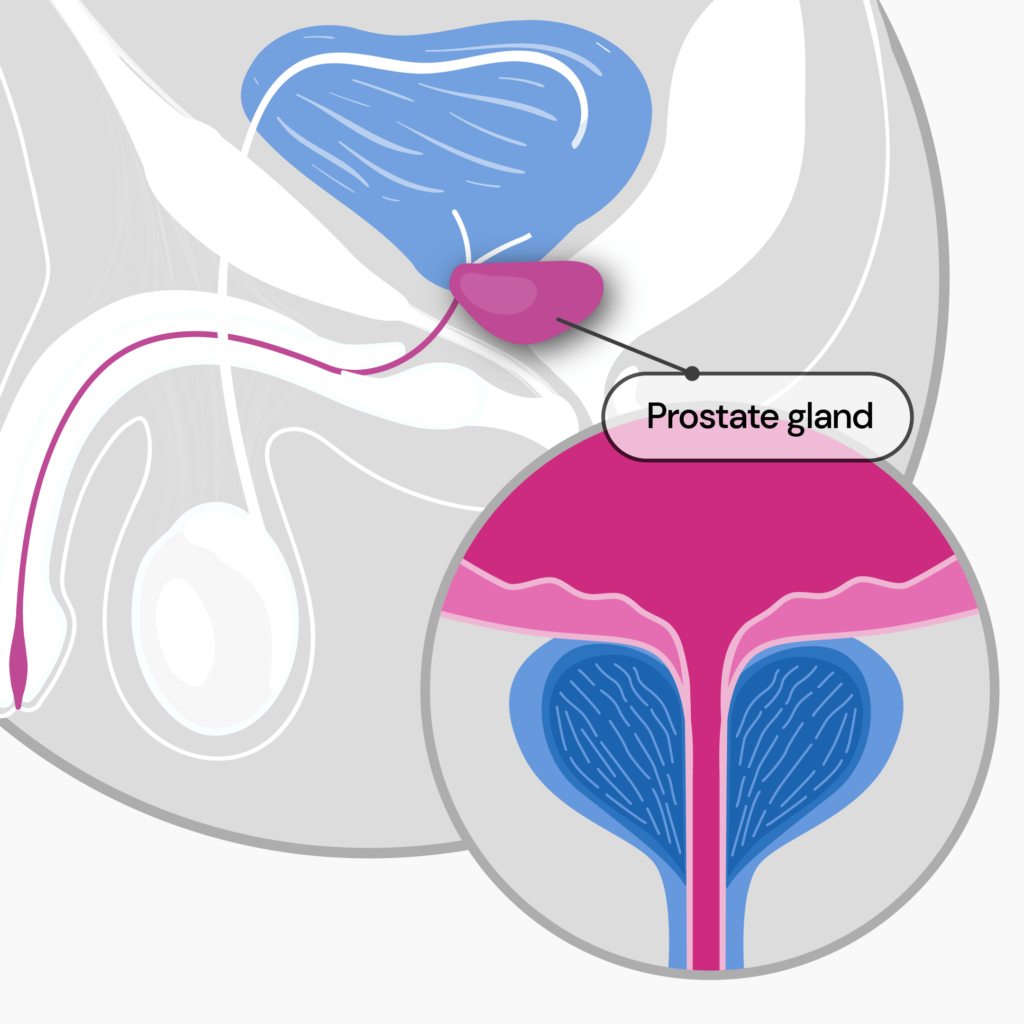
The prostate is a walnut-shaped gland located below the bladder and in front of the rectum.
It forms a part of the male reproductive system and forms the fluid portion of semen.
When the cells in the prostate start to multiply or grow uncontrollably, they form a tumor.
As the tumor grows, the signs and symptoms of the condition start appearing.
While most prostate cancers are slow-growing, some can be aggressive and life-threatening.
Prostate cancer is a common cancer among middle-aged and older men.
A small percentage of prostate cancers are hereditary and run in families.
Everyone with a prostate is at risk for prostate cancer.
A few factors that may increase your risk for prostate cancer are:
Prostate cancer has a good prognosis when diagnosed and treated early.
However, like most diseases, prostate cancer does not cause signs or symptoms in the early stages.
Here are five warning signs of prostate cancer that may help in its early detection and prompt treatment:
Other signs that may be a sign of prostate cancer are weak urine flow and unexplained pain around the prostate when sitting.
In cases where cancer has spread beyond the prostate, there may be swelling in the back, hip, and lower body.
Unexplained weight loss with changed bowel and urinary habits may also be seen.
Despite family history being one of the risk factors for prostate cancer, many cases of the condition are not related to inherited genes.
These cancers occur due to mutations (abnormal changes) in the prostate gland cells (somatic variations).
When prostate cancer is related to inherited gene mutations, the inheritance pattern depends upon the gene involved.
The most common genes that cause prostate cancer are inherited in an autosomal dominant pattern.
This means having just one copy of the altered gene is sufficient to increase an individual’s chance of developing prostate cancer.
Prostate cancer may not always be hereditary.
However, did you know prostate cancer is the most inheritable of all the major cancers?
58% of prostate cancer is driven by genetics.
Men with a close relative with prostate cancer are twice as likely to develop the condition.
5% to 10% of prostate cancers are found to be hereditary.
Most inherited prostate cancer cases occur due to these three genes– BRCA1, BRCA2, and HOXB13.
Men with BRCA2 and HOXB13 gene variants are at a higher risk of developing life-threatening forms of prostate cancer.
BRCA1 and BRCA2
BRCA1 and BRCA2 genes produce proteins that fix DNA and maintain the stability of the cell’s genetic information.
These genes are called tumor suppressors because they prevent cells from growing and multiplying fast or uncontrollably.
When these cells undergo mutations, they lose their ability to repair DNA and give rise to breast, prostate, and other cancers.
HOXB13
The HOXB13 gene provides instructions for producing a protein that binds to specific regions of the cell DNA and regulates the activities of other genes.
The protein produced by the HOXB13 gene is called a transcription factor.
Like the BRCA1 and BRCA2, the HOXB13 is also called a tumor suppressor.
So, any mutation in the HOXB13 gene may result in prostate cancer.
Other genes that are associated with prostate cancer include:
Prostate Specific Antigen (PSA) and Direct Rectal Examination (DRE) have been routinely recommended for screening prostate cancer.
Two groups of men are recommended to undergo genetic testing for prostate cancer:
For example, PARP inhibitors like olaparib and rucaparib are FDA-approved medications for individuals with a specific type of metastatic prostate cancer.
Undergoing a genetic test to look for any mutation that may lead to prostate cancer can benefit the entire family.
In usual screening for prostate cancer, a high PSA level is used to determine the further course of disease management.
However, genetic testing allows the doctor to determine if an individual needs a biopsy, even with a low PSA level.
At the end of a hectic day, we all look forward to heading back home to our bed and getting a good night’s sleep. Well, why not! A good night’s sleep is like a reboot button that ensures our mind, body, and soul are adequately rested and we wake up fresh and rejuvenated the following day. But not everyone is blessed to have a good night’s sleep. Besides insomnia, another condition linked to poor sleep and an increased risk of health complications is sleep apnea. Did you know snoring, a simple yet annoying habit many people have, maybe a sign of sleep apnea? This article attempts to answer the question, “Can sleep apnea lead to brain damage?”
Did You Know? Your ancestry test DNA data includes 700,000 markers, which can be used to learn everything from disease risk and drug sensitivities to nutritional requirements and fitness parameters. Learn more.
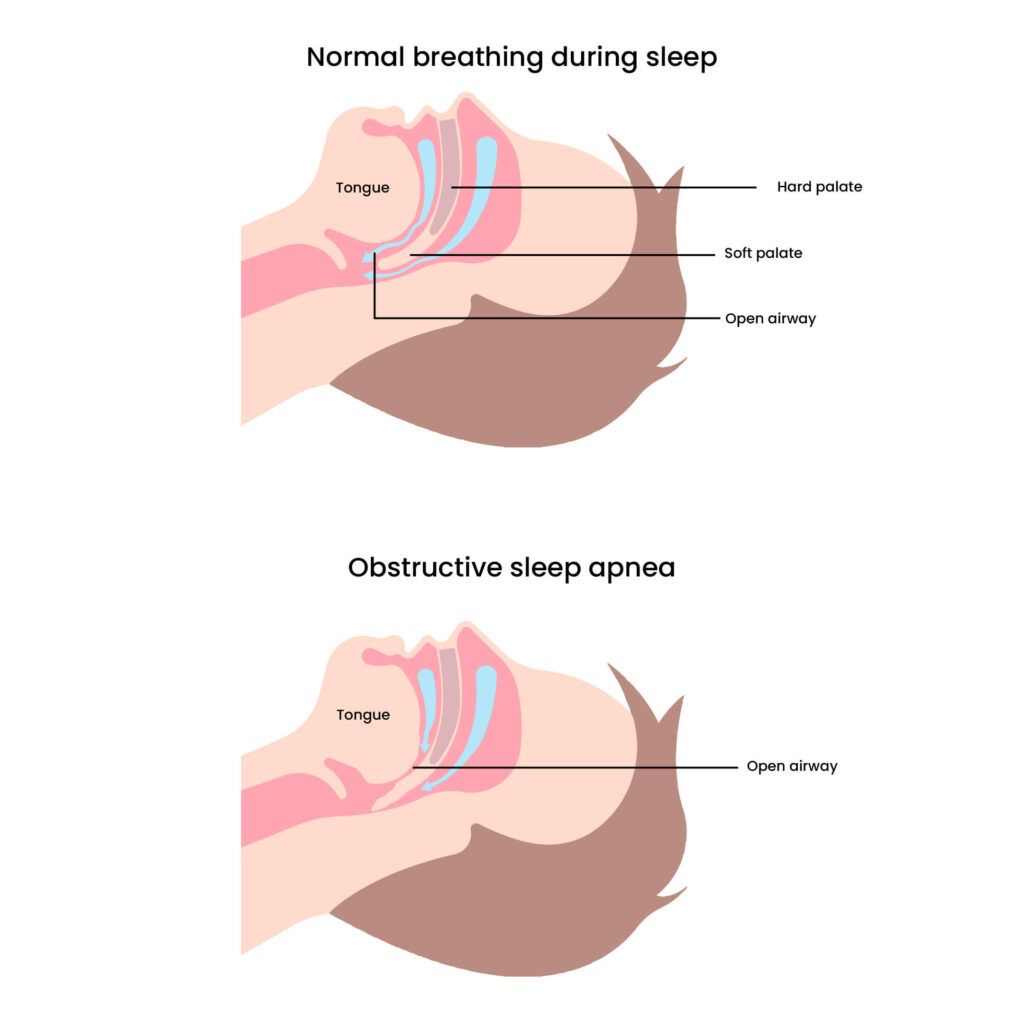
Sleep apnea is a medical condition that causes interrupted breathing during sleep.
Obstructive sleep apnea (OSA) is the most common type of sleep apnea, which occurs when something blocks the airway temporarily or permanently during sleep.
Sleep apnea is characterized by paused or shallow breathing during sleep.
This results in low levels of oxygen in the blood during sleep time.
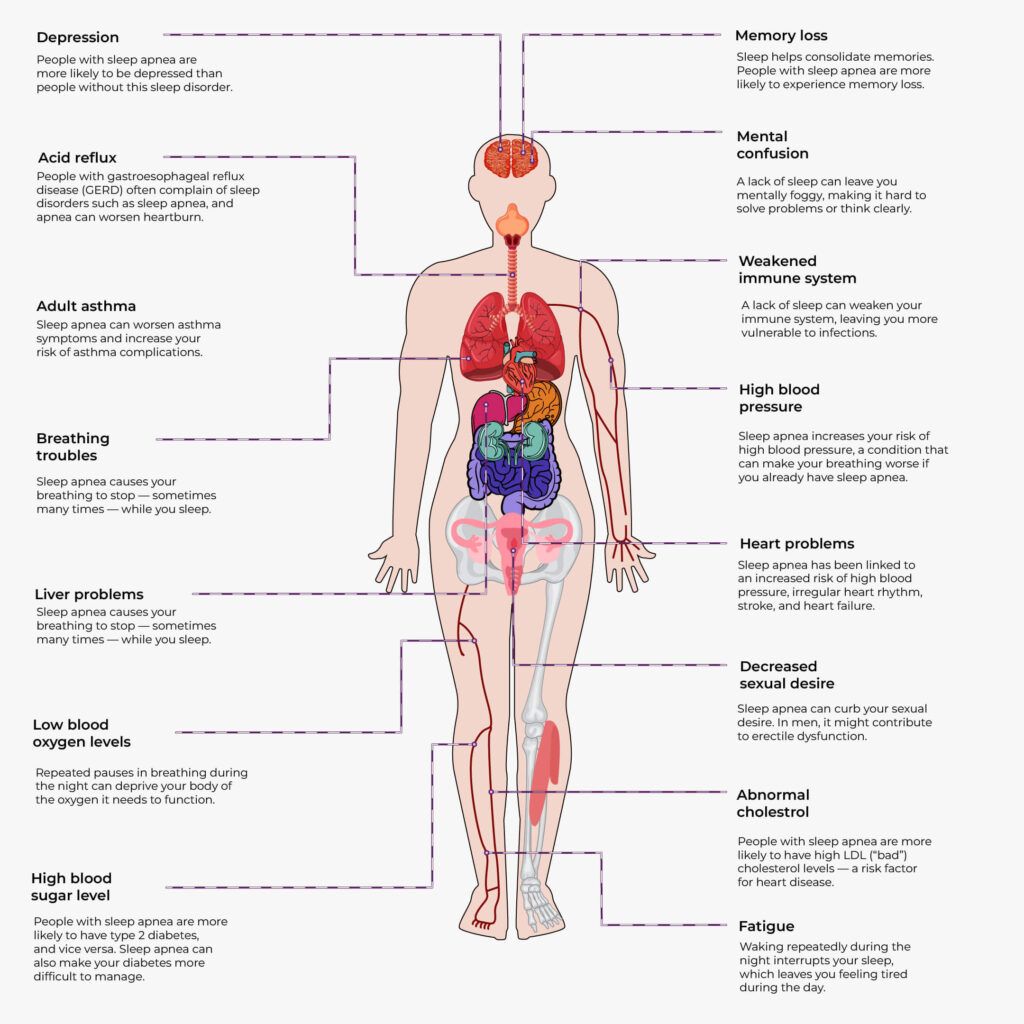
Untreated sleep apnea has been linked to stroke, acute coronary syndrome, neurodegenerative disease, obesity, and type 2 diabetes.
Most people with sleep apnea are unaware of their condition.
It is often a partner, spouse, or family member who observes the following signs in an individual with sleep apnea:
The individual with sleep apnea may experience the following symptoms:
Obstruction in the airways that is seen in sleep apnea may occur due to the following:
Causes of obstruction mentioned above may occur due to any of the following conditions:
Some people are more prone to sleep apnea than others.
A few risk factors of sleep apnea include:
While sleep apnea causes symptoms related to breathing and increases the risk of developing various cardiovascular conditions, it also impacts the brain.
Sleep apnea is associated with an increased risk of brain damage.
If uncorrected or untreated in time, sleep apnea may cause emotional dysfunction and cognitive impairments.
People with sleep apnea often have problems with mood and memory.
This happens because sleep apnea affects structures in the brain that regulate memory, mood, and attention.
Some studies state that sleep apnea may reduce the amount of gray matter (the tissue responsible for the brain’s ability to process information).
Here are some ways sleep apnea contributes to brain damage:
Sleep apnea causes periodic breathing interruptions throughout the night.
These pauses in breathing disrupt REM sleep cycles that are important for memory and learning.
Over a period of time, the lack of REM sleep can result in cognitive impairment and memory loss.
The interruptions in breathing in people with sleep apnea may cause hypoxemia (low oxygen levels in the blood).
When the brain does not receive an adequate and constant supply of oxygen, it may lead to brain damage and death.
Studies have shown that untreated obstructive sleep apnea can break down the blood-brain barrier(BBB) (BBB protects the brain tissue from harmful substances).
As a result, the individual is more prone to conditions like stroke, epilepsy, multiple sclerosis, and meningitis.
The link between sleep apnea and neurological problems is bidirectional.
Research states that individuals with neurological conditions like Parkinson’s, myotonic dystrophy, and myasthenia gravis have a higher chance of sleep apnea.
At the same time, sleep apnea also increases the risk of developing neurological problems.
Recent studies have shown a relationship between OSA and neurological disorders, including neurodegenerative diseases, epilepsy, and stroke.
OSA may also accelerate mild cognitive impairment in Alzheimer’s disease.
According to a study published in May 2023 in the journal Neurology, sleep apnea and snoring may harm your brain health.
Researchers found that people with severe sleep apnea have a higher risk of developing brain biomarkers associated with cognitive decline, increased risk of strokes, and Alzheimer’s.
These biomarkers are sensitive signs that indicate early cerebrovascular disease.
The study observed 140 people, with an average age of 72, all of whom had sleep apnea.
Of these participants:
All the participants were cognitively unimpaired and did not have dementia.
They were subjected to two types of MRI scans.
While observing the brain, researchers found that people with severe sleep apnea had more damage to their white matter than those with deep sleep (also called slow-wave sleep).
The study also highlighted that for every 10% decreased time spent in deep sleep, white matter changes were similar to being 2.3 years older.
The study's co-author, Dr. Carvalho, stated that the association of sleep apnea with brain damage was found to be more in people with a severe form of the condition.
Mild to moderate sleep apnea may not affect white matter in the brain.
Further studies are required in this area to assess the causation of these changes.
Brain damage due to sleep apnea has been well-established.
But is it reversible?
The good news is- Yes, it is!
Continuous positive airway pressure (CPAP) therapy can help reverse the damage to the white and gray matter in individuals with sleep apnea.
The first choice of treatment for most sleep apnea cases is CPAP therapy.
CPAP Therapy involves the placement of a mask over the nose or nose and mouth while sleeping.
This is done using a continuous positive airway pressure (CPAP) device, which blows pressurized air into the lungs and keeps the airways open during sleep.
Besides relieving sleep apnea symptoms, CPAP therapy has been found to reverse brain damage partially or entirely.
Researchers also found that white matter takes longer to respond to CPAP therapy than gray matter.
If you or someone you know is living with sleep apnea, you must get it treated at the earliest.
Here are a few tips that make coping with sleep apnea possible:
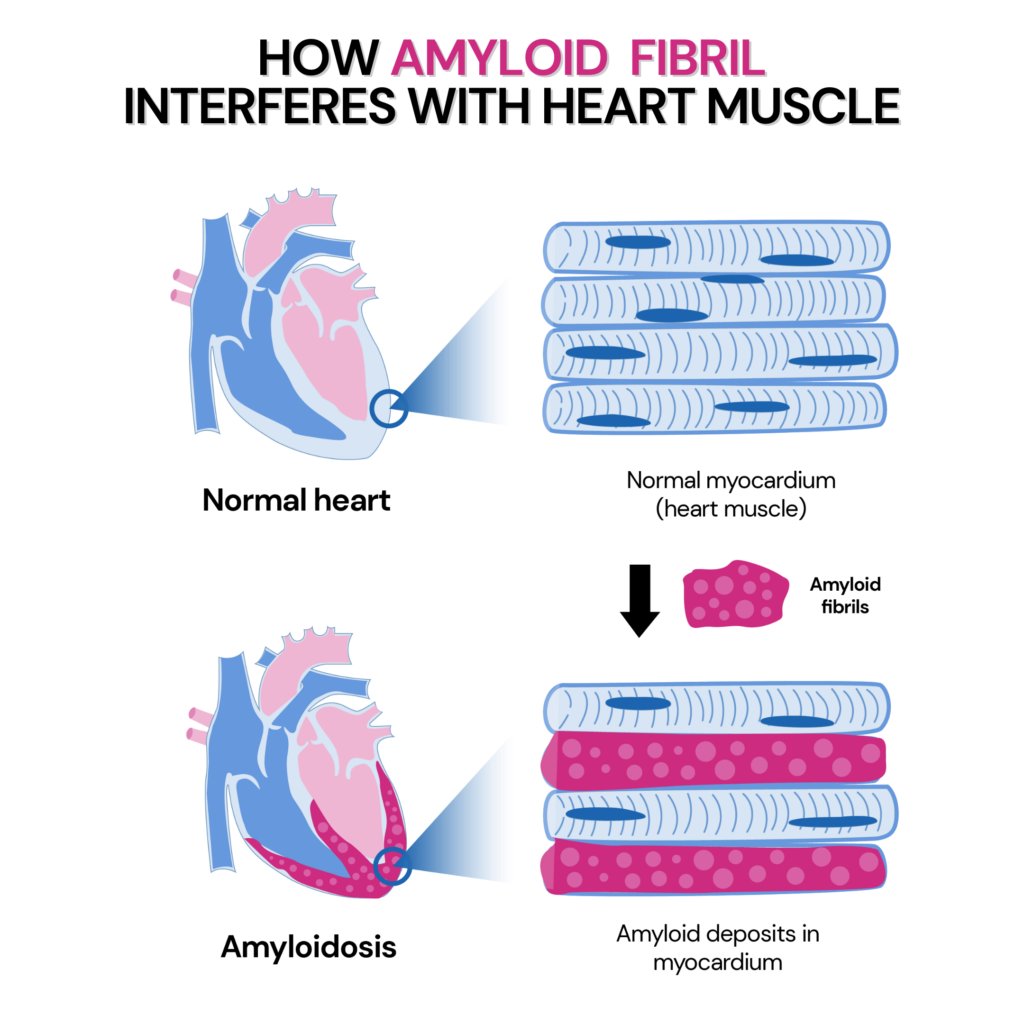
Proteins are the building blocks of the body. But can they be harmful to us? Well, they surely can! While most proteins are helpful to the body, some can give rise to diseases. One such protein is amyloid.
Amyloid is abnormal fibrous, extracellular, and proteinaceous deposits in organs and tissue. It is insoluble in nature and has no functional role in the body. In fact, deposits of amyloid in organs and tissues result in a range of diseases called amyloidoses.
Did you know: Diseases like type 2 diabetes and Alzheimer’s can develop as a result of amyloid deposits in the body?
Let’s learn more about hereditary amyloidosis, a rare condition caused by abnormal changes or mutations in some genes!
Did You Know? Your 23andMe or other ancestry test DNA data includes 700,000 markers, which can be used to learn everything from disease risk and drug sensitivities to nutritional requirements and fitness parameters. Learn more. Here's how others like you have benefited by uploading their data to Xcode Life:
Amyloidosis is a name given to a group of rare and serious systemic diseases that are caused by amyloid deposits.
When amyloid gets deposited in various tissues and organs, it is difficult for them to work properly.
Without timely treatment, it can result in organ failure.
Amyloidosis can be systemic or localized.
Primary or AL (light chain immunoglobulin) amyloidosis is the most common type of systemic amyloidosis, whereas ATTR or hereditary amyloidosis runs in families.
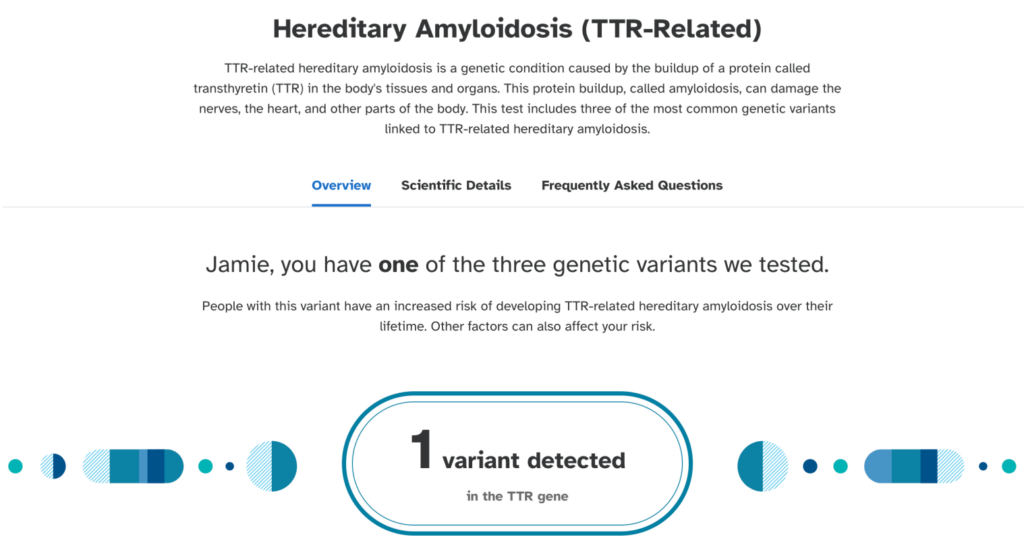
Hereditary amyloidosis is a rare form of disease that is caused by an abnormal genetic change.
While several genes can cause hereditary amyloidosis, the most common one is ATTR which is caused by mutations in the transthyretin or TTR gene.
ATTR amyloidosis runs in families, and people with this condition produce abnormal TTR proteins throughout their lives, which results in amyloid deposits.
Hereditary amyloidosis is passed down from parents to their children.
For this reason, genes are believed to play an essential role in developing this condition.
Hereditary amyloidosis may produce symptoms at any age beginning around 30 years.
The symptoms of this condition depend upon the following:
Here are some common symptoms of this disease:
When amyloid gets deposited in the heart, it causes stiffening of the heart muscles.
You may experience symptoms like:
Amyloid deposits can cause peripheral and autonomic neuropathy.
It is caused when the nerves supplying the extremities like arms, hands, legs, and feet are inflamed or damaged.
Symptoms of peripheral neuropathy include:
It damages the nerves that supply internal organs like the heart, stomach, and intestines.
Symptoms of autonomic neuropathy include:
Amyloid deposits in the digestive system can affect the nerves that supply the area.
A few symptoms that you may experience include:
When amyloid gets deposited in the kidneys, it affects how they filter toxins and proteins from the blood.
This may give rise to a nephrotic syndrome characterized by
If not attended to in time, nephrotic syndrome can progress to cause renal failure.
There are two types of Familial transthyretin-associated amyloidosis (ATTR amyloidosis), namely:
Hereditary can be of different types, the three most common ones being:
Hereditary amyloidosis may affect organs, including the heart, liver, kidneys, nervous and digestive systems.
Sometimes, the spleen may be affected too.
Since TTR protein is primarily made in the liver, amyloidosis most commonly affects it.
TTR protein transports the hormone thyroxine and retinol (Vitamin A) around the body, thereby getting its name transthyretin.
Hereditary ATTR amyloidosis is caused by a mutation in the transthyretin (TTR) gene that is inherited.
This mutation produces an abnormal TTR protein that is unstable and misfolds, forming aggregates of amyloid in different tissues and organs.
Hereditary amyloidosis is inherited as an autosomal dominant pattern.
Autosomal dominant condition is when a person develops the genetic condition with just one copy of the defective gene.
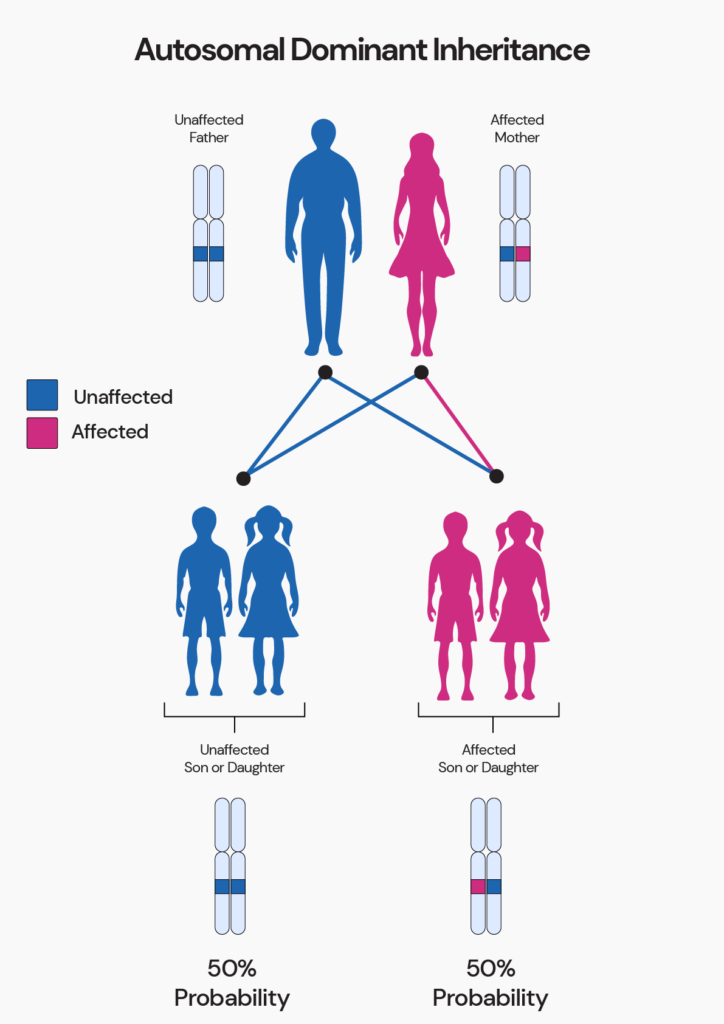
However, not everyone with an affected gene develops the condition despite an autosomal inheritance pattern.
This is due to a genetic principle called incomplete penetrance.
According to this principle:
Hereditary amyloidosis is diagnosed by:
Hereditary ATTR amyloidosis is confirmed if the genetic test confirms the presence of the mutated ATTR gene.
The challenge of diagnosing amyloidosis based on signs and symptoms is that they are similar to many routine health conditions.
A few of these conditions that can be mistaken for amyloidosis are:
A genetic test, a type of blood test, is the best way to diagnose hereditary amyloidosis.
This may be followed by a few scans to identify the type of amyloidosis and differentiate ATTR from AL amyloidosis in organs like the heart.
Immunohistochemistry and mass spectrometry may also be used to differentiate between ATTR and AL amyloidosis.
23andMe Health + Ancestry service covers a report on this condition.
Based on your genetic makeup, the results can tell you if you may have an increased risk of developing TTR-related hereditary amyloidosis.
23andMe analyzes 3 variants to adjudge the risk of this condition.
Until recently, the only treatment for hereditary amyloidosis was a liver transplant.
However, with medical advances, several drugs can help treat hereditary ATTR.
Treatment for hereditary amyloidosis today involves:
Drugs called TTR stabilizers are used to stop the production of TTR proteins and amyloid deposits.
This approach is done through gene silencing.
Gene silencers are drugs that prevent TTR protein production by blocking the TTR gene.
These treatments have been approved for hereditary ATTR peripheral neuropathy.
Though this is a suggested method for treating hereditary amyloidosis, no approved drugs exist.
A few drugs are being tested in clinical trials.
Sometimes, the underlying cause cannot be addressed.
In these cases, supportive treatments are prescribed to help relieve symptoms and improve the individual’s quality of life.
Factors like age, overall health, and extent of organ damage are considered when recommending supportive treatment.
If you have amyloidosis, your diet can play a role in preventing and worsening of symptoms.
Here are some foods that are high in amyloid-like fiber:
Here are foods that are safe and recommended for people with amyloidosis:
Xcode Life's comprehensive DNA analysis includes 10 health and wellness reports.
If you have done an ancestry genetic test with companies like 23andMe, AncestryDNA, MyHeritage, etc., you can learn everything about your health in just 3 steps.
Not yet tested?
If you're new to the world of genetic testing, we've got you covered!
You can now get your ancestry DNA kits at an additional discount!
By following the link provided in this article, you can purchase a DNA kit at 10% OFF (the discount will be reflected when you add the product).
This will ensure that you have everything you need to embark on your genetic journey.
Once you receive your kits, you can follow the instructions given by the respective service providers to collect your sample and ship it.
After you receive your DNA test results from the kit, you can upload your DNA data to our secure platform.