If you're one of the many people who struggle with getting a good night's sleep, you may have heard of various remedies to help you doze off, including taking vitamin supplements. One such supplement is vitamin B6, which is believed to have multiple health benefits, including promoting healthy sleep. But just how effective is vitamin B6 in improving sleep quality? In this article, we'll explore the scientific evidence behind this claim and provide you with a clear answer.
Vitamin B6, or pyroxidine, is an essential nutrient for the body.
It is a significant part of many bodily processes and is needed to keep the nervous system healthy.
It is also required for normal immune function.
Some people who suffer from kidney disease can have a vitamin B6 deficiency in the body.
Certain autoimmune disorders, a weakened immune system, and anemia can also cause vitamin B6 deficiency.
If you are persistently nauseous, especially in your first trimester, your doctor might prescribe vitamin B6 supplements.
It is said to improve the quality of sleep.
Dopamine, also known as the happy hormone, improves mood.
However, more evidence is needed to back this claim.
For adults aged 50 or below, the RDA of vitamin B6 is 1.3 milligrams.
After age 50, women are recommended to take 1.5 milligrams, while men must take 1.7 milligrams of vitamin B6.
It is always advisable to consult your doctor before starting any supplement.
Vitamin B6 is essential for the synthesis of the amino acid tryptophan.
Tryptophan is a precursor to serotonin, a hormone known for regulating sleep.
Vitamin B6 converts tryptophan to serotonin and niacin, or vitamin B3.
Since vitamin B6 cannot be stored in the body, getting adequate vitamin B6 from your diet is essential.
Tryptophan is also necessary for melatonin production.
Melatonin is a hormone that regulates the sleep-wake cycle, also called the diurnal rhythm.
Vitamin B6 plays a vital role in the synthesis of GABA.
GABA is an amino acid that depresses the central nervous system and produces a calming effect that reduces sleeplessness.
Pyridoxal 5’ phosphate is the active coenzyme form of vitamin B6.
Studies have shown that P5P deficiency can cause altered mental states, confusion, and depression.
The Mayo Clinic recommends 1.3 to 1.7 mg of P5P daily for adults.
The dosage increases to 1.9 to 2.0 milligrams daily during pregnancy and lactation.*
*The dosages mentioned here are for informational purposes only. Please consult a qualified medical practitioner for advice.
Clinical trials have shown that too much vitamin B6 can cause adverse side effects in the body.
This overdose is rarely due to food sources but from vitamin B6 supplementation.
More than 1000 milligrams of pyridoxine can cause sensory neuropathy, according to studies.
Perceptual and Motor Skills journal conducted a trial with 100 people in 2018.
In this trial, participants who took over 240 mg of vitamin B6 supplementation reported lowered sleep quality.
They further said that they felt more tired upon waking up.
Besides vitamin B6 or pyridoxine, vitamin B12 plays a role in regulating sleep.
It supports the production of neurotransmitters in the brain that help in sleep.
Vitamin D, also called the sunshine vitamin, helps improve sleep quality.
A study showed that vitamin D, combined with omega-3 fatty acids in fatty fish like salmon, improved sleep in subjects.
Apart from having calcium, milk is also rich in vitamin B6.
One cup of goat or cow’s milk provides 5 percent of the daily requirement of vitamin B6.
It has one of the highest concentrations of vitamin B6 among foods.
The wild varieties of salmon usually have a higher concentration of nutrients than the farmed ones.
They provide almost 10 percent of the daily recommended dose of vitamin B6.
They supply as much vitamin B6 as a glass of milk.
In addition, they are versatile vegetables that can be eaten raw or cooked.
Vitamin B6 is a nutrient that plays a vital role in metabolism.
It helps in the digestion of protein and keeps your adrenal glands healthy.
In addition, it helps protect your nervous system.
Vitamin B6 deficiency can manifest in the body as insomnia, depression, and mental confusion.
Studies found that adequate amounts of vitamin B6 are necessary for good sleep, as too much or too little can disrupt it.
Chicken, fish, milk, and vegetables like carrots and spinach are all rich in vitamin B6.
Did you know that sudden weight loss can affect vitamin absorption in your blood?
Vitamin K is a fat-soluble vitamin that is essential for many bodily functions.
It requires body fat to be adequately absorbed in the blood.
So before you jump into another fad diet, read on to find out just how essential Vitamin K is for the body.
Vitamin K is a fat-soluble vitamin that naturally occurs in two forms.
Phyloquinone, or Vitamin K1, is the primary type found in green leafy vegetables like kale and spinach.
Menaquinone (MK), also called Vitamin K2, is located in fermented foods.
Vitamin K2 can have various subtypes.
MK-5 and MK-15 are in fermented foods, while MK-4 is in chicken, butter, and egg yolks.
Vitamin K is necessary for healthy bone-building in the body.
In addition, Prothrombin, an essential protein for blood clotting, is dependent on Vitamin K.
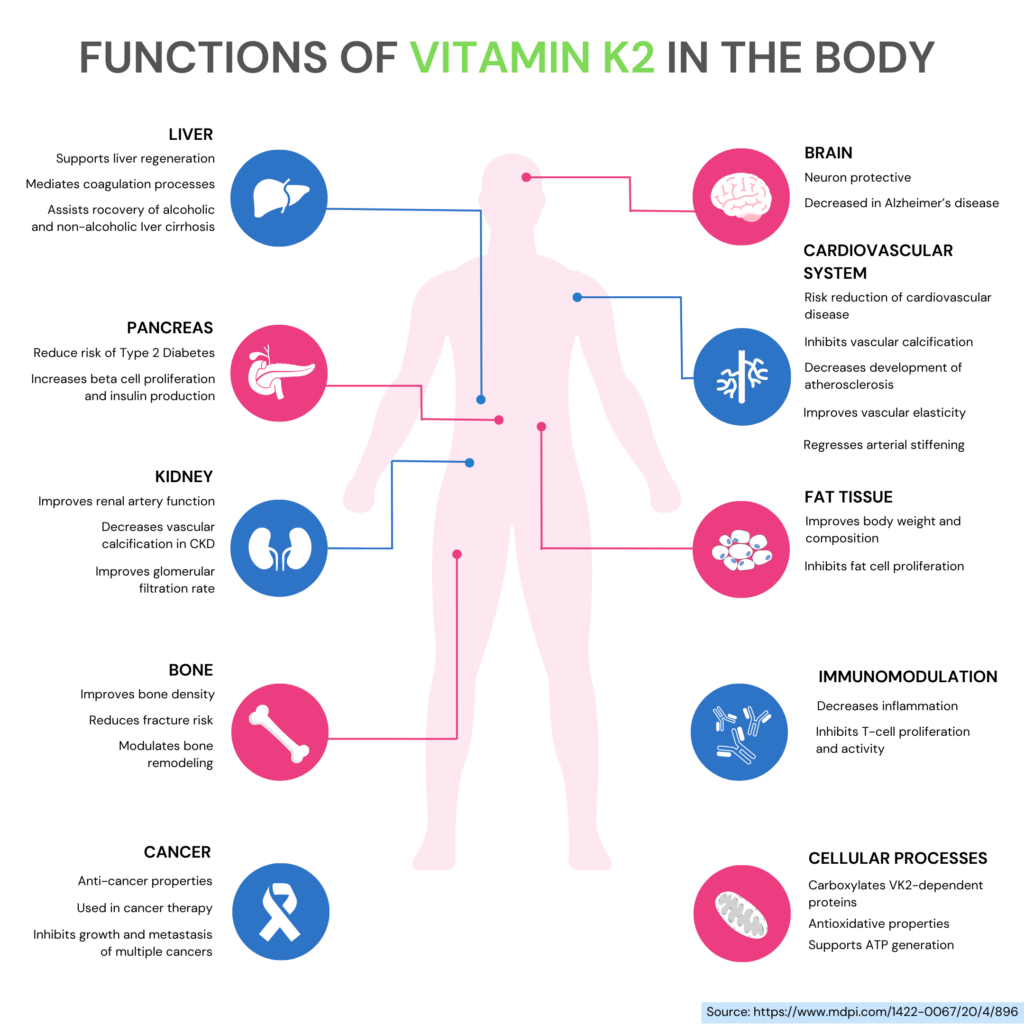
Blood clotting is a naturally occurring process that helps prevent excessive blood loss in an injury.
It involves a cascade of coordinated reactions that plugs the injury site with a clot.
Prothrombin, a protein essential for blood clotting, needs Vitamin K for proper functioning.
Thus Vitamin K is necessary to heal wounds.
An enzyme called gamma-glutamyl carboxylase is necessary for adequately functioning osteocalcin, a protein in bone.
This enzyme depends on Vitamin K.
Thus, you lose bone mass and density when your body is low on Vitamin K.
It can cause bone thinning, called osteoporosis, and frequent fractures.
Some studies show that adequate Vitamin K can prevent hypertension.
Vitamin K interacts with and regulates your blood calcium levels.
As a result, it keeps your blood pressure in check.
Calcium can get mineralized and deposited on the walls of our blood vessels as we age.
Adequate amounts of Vitamin K can help remineralize the calcium and prevent heart ailments.
Sphingolipids are found in brain cell membranes.
These lipids are involved in cellular metabolism.
Changes in their functioning can cause neurodegenerative disorders like Alzheimer’s disease.
Higher levels of phylloquinone can improve memory and prevent age-related cognitive decline.
The average amount of Vitamin K is 120 micrograms for adult men and 90 micrograms for adult women.
Vitamin K deficiency is rare in adults but not impossible.
Some medications can cause a decreased absorption of Vitamin K in the blood.
Infants are prone to Vitamin K deficiency as mother’s milk has a low concentration, and this vitamin cannot cross the placenta.
As a result, you might suffer from excessive bleeding, even from a minor injury.
You might break or fracture bones even from minor falls if deficient in Vitamin K.
Infants who do not receive a Vitamin K injection at birth are at increased risk of developing a deficiency.
Certain diseases affect Vitamin K absorption in the blood.
People with celiac disease, ulcerative colitis, and cystic fibrosis are more prone to a deficiency.
People who have undergone bariatric or weight loss surgery might also develop a deficiency of Vitamin K in the body.
Vitamin K deficiency in the body can make you suffer from many other diseases:
Vitamin K is essential for healthy bone development.
If you suffer from a deficiency of it, you may develop osteoporosis.
This disease brittle your bones, and you can easily break a bone even from a minor injury.
Some studies have shown that Vitamin K can prevent heart disease.
A deficiency of this vitamin can cause the narrowing of blood vessels in the heart and can cause coronary heart disease.
Vitamin K can have severe and harmful interactions with some other drugs.
It can interact with warfarin (Coumadin), a blood thinner or anticoagulant.
If you are on warfarin, limit the intake of Vitamin K from food and dietary supplements.
Consuming less Vitamin K might cause bleeding, while consuming more may cause blood clots.
Some food sources of Vitamin K are:
They are rich in phylloquinone.
Soybeans and Natto, a traditional fermented Japanese dish, are rich in Vitamin K.
Vitamin K is a fat-soluble vitamin found in leafy green vegetables.
It is essential for bone health and blood clotting.
Vitamin K can also prevent cardiovascular diseases and Alzheimer’s disease.
A deficiency of Vitamin K can make one prone to osteoporosis and elevated blood pressure.
Vitamin K can also react adversely with certain medications.
It can have an antagonistic effect on common anticoagulants like warfarin.
So, it is always advisable to consult your doctor before starting any supplements.
Vitamin K is naturally found in green leafy vegetables like spinach and kale.
Are you at risk of developing glaucoma?
While many factors can contribute to this debilitating eye condition, genetics play a crucial role.
Understanding the genetic components of glaucoma can help you take the necessary steps to protect your vision and prevent vision loss.
This article will share five key facts about glaucoma that you might find interesting and useful.
We may be “secret carriers” of certain conditions. This means that we may not have the condition but possess the ability to pass it to the next generation.
Glaucoma is a disorder where the optic nerves are damaged.
The optic nerves connect your eye with the brain.
Optic nerve damage happens when there is a build-up of pressure within the eye, called intraocular pressure.
This optic nerve damage can eventually lead to peripheral vision loss and eventual blindness.
Other common symptoms of glaucoma are bulging eyes and sensitivity to light, also called photophobia.
Glaucoma usually affects older adults.
Some health conditions that increase the risk for glaucoma include diabetes mellitus and hypertension.
A family history of glaucoma is another risk factor.
Early onset glaucoma affects individuals below 40 years of age.
It is a congenital type of glaucoma that runs in the family.
If glaucoma appears before age 3, it is called primary congenital glaucoma.
Our eyes have two primary fluid types: aqueous humor and vitreous humor.
These fluids provide nutrition to the eye and help maintain pressure inside the eye.
These circulating fluids also require proper drainage.
Intraocular pressure builds up when there are problems with a fluid drainage system.
As a result, the optic nerves are damaged.
Eventually, this might lead to blindness.
The most common form of glaucoma is primary open-angle glaucoma.
Primary open-angle glaucoma is hereditary.
If any of your immediate family members have this condition, you are at risk for developing glaucoma.
Make sure that you consult your eye doctor regularly.
When fluid cannot drain from your eyes, it causes open-angle glaucoma.
It, in due time, builds up pressure in the eyes, which damages the optic nerve.
It is the most common type of glaucoma.
There may be no apparent symptoms.
However, you might experience blind spots or tunnel vision.
Genes like CDKN2B-AS, SIX1/SIX6, TMCO1, and CAV1/CAV2 pose the risk of developing open-angle glaucoma.
Mutations in the WDR36 gene on chromosome 5q22 are responsible for 17% of primary open-angle glaucoma.
This condition develops when your iris is not wide open, which leads to improper fluid drainage.
This condition can have symptoms like eye pain, redness, blurred vision, and vomiting.
It may cause blindness.
Mutations in the COL18A1 can cause this condition.
The inheritance pattern of the COL18A1 gene is autosomal dominant - one copy of the faulty gene is enough to cause the condition. 50% risk for glaucoma if either parent has it.
Studies have shown that mutations in this gene can cause angle-closure glaucoma in the fourth decade of life or later.
This type of glaucoma is different from the other types because your eye pressure does not change in this condition.
Your eye doctor can still detect this condition and recommend treatment options.
Variants in a gene containing two proteins, myocilin, and optineurin, can cause this condition.
The TBK1 gene on chromosome 12q14 accounts for 1% of normal-tension glaucoma.
Glaucoma can have different inheritance patterns.
Primary congenital glaucoma is inherited in an autosomal recessive pattern.
It means that both gene copies in each cell should have the variant.
Some studies have suggested that more than 50% of glaucoma is hereditary.
In addition, the risk is ten times higher when a sibling has glaucoma.
Glaucoma is an autosomal recessive condition (except for some types).
Both parents can be carriers of the disease but not have the condition themselves.
When a child inherits these mutations from both parents, they risk developing this condition.
Glaucoma is a disorder that can affect any individual.
However, scientists have found that some groups and races are more likely to develop glaucoma.
African Americans have the highest risk of developing glaucoma.
Cataracts it is the leading cause of blindness among this group.
Aged people of Hispanic descent also show an increased risk of developing glaucoma.
Among Asians, Japanese people have the highest risk of developing normal tension glaucoma.
Approximately 1 in every 50 Americans is a carrier for a rare genetic disorder that can cause spinal muscular atrophy (SMA).
If you are thinking of starting a family or are already pregnant, understanding your carrier status is crucial for the health of your child.
That's why carrier screening for SMA has become increasingly important in recent years.
We may be “secret carriers” of certain conditions. That is, not have the condition but possess the ability to pass it to the next generation. Learn more:
SMA is a group of hereditary diseases that damage and kill nerve cells in the brain and spinal cord.
The condition affects specialized motor neurons (nerve cells).
Motor neurons control the voluntary movement of arms, legs, face, throat, and tongue.
They also help bring about skeletal muscle activity required for actions like speaking, walking, swallowing, and breathing.
The most common form of SMA develops due to an abnormal change (mutation) or a missing part in the survival motor neuron gene 1 (SMN1).
This gene is responsible for producing a protein essential for the functioning of motor neurons.
Due to its effect on the motor neurons, SMA causes muscles supplied by these neurons to become smaller and weak (atrophy).
There are four types of SMA:
This type of SMA, also called Werdnig-Hoffman disease or infantile-onset SMA, is usually evident before six months of age.
Children with type I SMA show reduced movements and shortening of muscles or tendons.
They may also show symptoms like
Treatment is critical for children with type 1 SMA, without which they may die before age two.
This SMA type is usually noticed between six and 18 months of age.
Children with type II SMA can sit without support but cannot stand or walk without assistance.
Some children may also show respiratory difficulties.
Though the life expectancy of these children is reduced, most of them live till they reach adolescence and young adulthood.
Type III SMA is also called Kugelberg-Welander disease and is evident after 18 months of age.
Children with this type of SMA can walk independently but find it difficult to run, rise from a chair or climb stairs like their peers.
A few children with type III SMA may also develop complications like
When treated appropriately, children with type III SMA have average lifespans.
This type of SMA develops after 21 years of age, and individuals usually develop mild to moderate weakness in the leg muscles, along with other symptoms.
The SMN protein produced by the SMN1 gene is found throughout the body, with the highest concentration in the spinal cord.
It maintains specialized nerve cells called motor neurons in the brain and the spinal cord.
Motor neurons receive brain and spinal cord instructions, passing them on to skeletal muscles to cause body movements.
Mutations in the SMN1 gene can result in the loss of motor neurons, which leads to weakness and wastage (muscle death/atrophy) in the muscles responsible for movement.
95% of the individuals with SMA have a missing piece in both copies of the SMN1 gene.
In the other 5%, 1 copy of the gene has a missing piece, and the other copy has a mutation that interferes with the production and functioning of the protein.
SMA is an autosomal recessive neuromuscular disease - when both parents are carriers of the condition, and the child needs to receive two defective copies to be affected.
For a child to develop SMA, both parents must be carriers of the SMN1 gene.
Carriers have at least one copy of the affected gene but are unaffected by the condition.
It is rare that an individual inherits one recessive gene from a parent and acquires a new mutation in the other copy of the gene.
If both parents are carriers of SMA, there is a 25% chance of having a child with SMA in every pregnancy.
At the same time, there is a 50% chance of having a child unaffected by the condition and a 25% chance of having a child who is just a carrier.
Two prenatal tests can be used to detect if the growing fetus has an SMN1 gene mutation:
If both partners are SMA gene carriers, they must meet a genetic counselor before planning a pregnancy.
Carrier screening for SMA is recommended for couples at risk of having a child with the condition.
SMA carrier testing is recommended under the following conditions:
If you suspect you may be a carrier of SMA based on your family history, you must undergo a genetic test to determine your carrier status.
A genetic test can help determine if you are a carrier of SMA.
If you are a carrier for SMA, you have one healthy copy and one faulty or mutated copy of the SMN1 gene.
Around one in 40 to one in 60 people are carriers of this gene.
If you are a carrier for the SMA gene, it is recommended that your partner undergo a genetic test for their carrier status.
Prenatal testing is available for SMA.
It is recommended when both partners are carriers of the SMA gene.
Prenatal testing can be done using chorionic villus sampling (CVS) or amniocentesis.
Carrier testing for SMA costs less than $500, depending upon insurance coverage, the number of conditions tested, and the laboratory used.
Many people may be unaware of its impact on the eyes regarding Ehlers-Danlos Syndrome (EDS), a rare genetic disorder affecting the body's connective tissues.
However, eye problems can be severe and sometimes life-changing for EDS patients. From vision loss to dislocated lenses, let's take a closer look at the link between EDS and the eyes.
EDS is a group of heritable disorders that affect connective tissues like the skin, ligaments, bones, blood vessels, and other tissues and organs.
There are 13 types of EDS, characterized by the following:
In some people, ocular manifestations of EDS have been identified.
1 in 5000 people is affected by EDS, and the hypermobile and classical forms of the condition are more common.
Abnormal changes (called mutations) in at least 20 genes have been identified to cause EDS.
Mutations in the COL5A1, COL5A2, and rarely COL1A1 cause the classical type of EDS.
The genes associated with EDS, such as COL1A1, COL1A2, COL3A1, COL5A1, and COL5A2, provide instructions for making different types of collagen.
Mutations in these genes, therefore, disrupt the production, processing, and assembly of normal collagen.
As a result, the individual has weakened connective tissues, which is characteristic of EDS.
The inheritance pattern of EDS varies based on the type.
The classical, vascular, arthrochalasia, and periodontal EDS have an autosomal dominant inheritance pattern.
This means having just one gene copy in each cell is sufficient to cause the condition.
Other forms likely show an autosomal recessive inheritance pattern, meaning both copies of the defective gene are needed to cause the condition.
An ophthalmologist must evaluate people with EDS to detect any eye abnormalities.
The ophthalmologist will usually perform a dilated eye exam to increase pupil size.
This enables them to examine the structures at the back of the eye, including the retina, blood vessels, and the optic nerve, for abnormalities.
If retinal abnormalities are detected, the individual should undergo eye checkups every three to six months.
Frequent eye examinations may be required if the individual sees floating structures or spots that interfere with their vision.
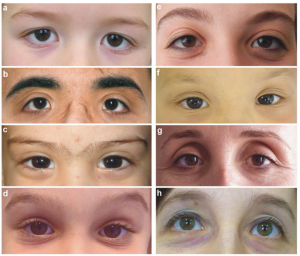
Individuals with kyphoscoliotic EDS tend to have eye and vision problems that can be rectified using corrective glasses.
Some studies indicate that vision problems may also be found across other types of EDS.
In EDS, collagen production is disrupted, resulting in abnormal collagen fibrils and improper assembly.
Mutations primarily cause this in the COL5A1 and COL5A2 genes.
Two other genes, ZNF469 and PRMD5, have been implicated in brittle cornea syndrome, a condition characterized by progressive cornea thinning.
Common vision problem in EDS: A Study
A study compared healthy volunteers with 50 individuals with classical EDS.
The analysis revealed structural changes in the corneas of EDS patients, resulting in symptoms like:
In rare cases, the sclera of EDS patients may turn blue.
The sclera, or the white of the eye, and the cornea (which covers the eye) comprise collagen.
Some functions of collagen in the eyes are
While collagen has an inherent capacity to stretch and regain shape, in people with EDS, collagen loses this elasticity.
Abnormal collagen production can result in many eye conditions and vision problems.
While some symptoms, like dry eyes, are manageable, others may require additional treatment.
A few severe eye conditions resulting from compromised collagen include
When retinal blood vessels leak or break, it is called wet macular degeneration.
It is called dry macular degeneration, when the retina deteriorates or wears out.
Both wet and dry macular degeneration leads to vision loss.
This gives rise to a sensation of a foreign substance in the eye and pain.
A few common ocular signs of EDS include:
Due to corneal changes in EDS, most patients with this condition complain of dry eyes.
Treatment for eye problems in people with EDS is similar to those with similar vision problems without EDS.
The ophthalmologist will treat structural issues with lens replacement, corneal replacement, or other surgical techniques wherever required.
However, surgery may not always be the first treatment choice for people with EDS.
Artificial tears or steroid eye drops may be prescribed to relieve dry eye symptoms.
Treatment and recovery times may be longer for people with EDS.
G6PD deficiency affects the body's ability to produce an enzyme essential for red blood cell function.
Vaccines are designed to stimulate the immune system and protect against infectious diseases.
For G6PD-deficient individuals, a common question is whether they should avoid any particular vaccination.
In this article, we aim to answer this question in detail.
G6PD deficiency disorder is a hereditary blood disorder.
It occurs when the body does not produce enough glucose-6-phosphate dehydrogenase enzyme.
As a result, red blood cells are destroyed earlier than their expected lifespan.
This premature death of RBCs causes hemolytic anemia.
It can also cause other symptoms like jaundice and shortness of breath.
Avoiding certain foods and medications might make this condition more manageable.
G6PD deficiency can manifest in various ways:
In dark-skinned people, paleness might not be very evident.
But it can manifest around the mouth and lips, indicating the presence of this condition.
It might make a person feel extremely tired most of the time.
However, nausea and dizziness also indicate lowered oxygen supply in the body.
The spleen’s function is to remove dead RBCs from the bloodstream.
When RBCs are getting destroyed at an abnormally high rate, the spleen is overloaded and can become enlarged.
It might be either due to the presence of RBCs in the urine or excess bilirubin resulting from hemolytic anemia.
G6PD deficiency disorder can be inherited from either one or both parents.
Men who have the defective gene causing this disorder show symptoms.
Women can become carriers of this disorder if they inherit the faulty gene.
If either or both parents pass this gene to their son, he will likely suffer from the disorder.
However, if they pass it on to their daughter, she will likely become a carrier of this disease.
Vaccines can immunize G6PD-deficient patients against several microbes.
They can be safely administered without the additional need to monitor the patient.
G6PD-deficient individuals are more susceptible to coronavirus infection.
They can have an altered immune response to viral infections.
People living with G6PD deficiency can be safely administered Covid-19 vaccines.
Clinical trials and research have shown that vaccines do not fall under G6PD deficiency medications to avoid.
There are no specific vaccine brands to choose from if someone suffers from G6PD deficiency.
Research hasn’t identified any vaccines as medication to be avoided. So, people deficient in G6PD can go ahead with recommended vaccinations.
Disclaimer: This article is for informational purposes only. The content of this article should not be taken as medical advice. Consult a qualified practitioner for any advice regarding G6PD deficiency.
Most people with G6PD symptoms can lead healthy lives if they avoid certain foods and medications.
They can cause a faster breakdown of red blood cells in the body, which can be dangerous for people with this condition.
Here is a G6PD allergy list to avoid:
Some G6PD deficiency antibiotics to avoid are sulfa drugs, like Bactrim and Septra.
They are commonly used to treat Urinary Tract Infections or skin infections.
Quinolone antibiotics like Cipro and levofloxacin used to treat pneumonia should also be avoided.
Other common drugs like Nitrofurantoin and dapsone should also be avoided.
Thus, testing the patient for G6PD deficiency before administering this drug is recommended.
G6PD-deficient patients can, however, tolerate many other malaria medications.
However, it can also cause a hemolytic crisis in the body.
Therefore, a patient should constantly undergo screening before administering this drug.
However, it can cause an allergy in patients with G6PD deficiency.
Common over-the-crowd drugs like Pepto-Bismol and Ecodrin also contain this drug.
G6PD-deficient patients can instead use Ibuprofen as a pain medication.
This chemical can trigger hemolysis in the body when inhaled or ingested.
The above list can be used as a G6PD allergy list.
Additionally, here are a few other things that can trigger a reaction in the body for G6PD deficient patients.
Favism is another name for G6PD deficiency.
Other legumes like lentils and peanuts can also potentially cause allergies.
However, it can cause a severe allergic reaction in G6PD-deficient patients.
Caffeine in coffee can interfere with and inhibit G6PD secretion in the body.
In addition, caffeine competitively inhibits G6PD’s binding ability with its coenzyme, NADP.
It can cause a hemolytic crisis (large numbers of blood cells are destroyed quickly) in the body.
So, for G6PD-deficient people, it is better to avoid coffee.
G6PD deficiency is a hereditary disorder that usually affects men.
Due to the under-secretion of G6PD in the body, the person can suffer from hemolytic anemia.
This condition can be managed by avoiding certain foods and common medications.
No vaccination has proven to be dangerous for those with G6PD deficiency.
These include coffee, fava beans, and antibiotics used to treat UTIs.