Depression or major depressive disorder is a mental health condition that affects an individual's behavior, mood, and overall health.
People with depression may experience prolonged feelings of sadness, hopelessness, and emptiness.
Depression usually begins in early adolescence or adulthood but can appear at any age.
Depression is one of the most common mental health conditions in the United States.
It is also more common in women and people assigned female at birth (AFAB) than men and people assigned male at birth (AMAB).
Common symptoms of depression are:
The symptoms of depression may vary slightly in the younger age group.
Common depression symptoms in adolescents and teens are:
Though the exact cause of depression is unclear, the disorder runs in families, hinting that genetic factors may increase one's risk of developing the condition.
Research is still underway to study the genetic variations that increase the risk for depression.
Other factors that may increase one’s risk for depression include:
Genetics plays a central role in the development of depression.
Scientists believe that nearly 40% of people with depression have a genetic link, while environmental and other factors make up for the remaining 60%.
Existing research states that a complex interplay of genes and other environmental (non-genetic) factors determine an individual’s risk of developing depression.
Few studies have reported that people having a first-degree relative with depression (a parent, sibling, or child) are three times more likely to develop the condition than the general population.
This shows that depression runs in families, and the disease has a significant hereditary component.
Some people can also develop the condition without a family history.
Though genetics influences the development of depression and anxiety, no single causative gene has been identified.
Research states that genetic variations on multiple genes contribute to the development of depression.
However, having a genetic variant does not confirm you will develop the condition.
Besides genetic variations, how genes are passed down to the next generation (mode of inheritance) may also affect an individual’s risk for depression.
A study published in The American Journal of Psychiatry reported that the research team isolated a gene prevalent in several families with a history of depression.
Chromosome 3p25-26 was found in over 800 families with recurrent depression.
Standard treatments used for depression are:
Most people require a combination of two or more treatments.
Did you know that your genes influence how well a treatment works for you? Several studies show that genes affect how your body absorbs, uses, and eliminates drugs like antidepressants.
Many genes influencing drug metabolism have been studied and are of specific interest to doctors and researchers.
If you have depression, it is essential to understand that treatment for this condition may take time.
You may have to undergo a couple of treatments to determine the most suitable one.
If you experience one or more symptoms of depression, it is important to seek medical care.
Before starting any antidepressant medications, informing your doctor about your medical history and current medication and supplements is essential.
This information will help your doctor determine the best treatment for you.
Learning about the genetic background of depression can help understand the condition better and provide optimal treatment options.
Caffeine is a psychoactive stimulant consumed worldwide mostly via two beverages, tea, and coffee. Pregnant women have always been advised to limit their caffeine intake since they may metabolize caffeine slowly. Studies also suggest that it can cross the placenta and enter the baby's bloodstream. A recent study published in the International Journal of Epidemiology reported that caffeine consumption alone might not contribute to adverse outcomes in pregnancy.
Pregnant women are often advised to cut off or limit their coffee consumption, owing to the reduced clearance of caffeine during pregnancy.
Pregnant women require a 1.5 to 3.5 times longer half-life to eliminate caffeine than non-pregnant women.
Caffeine, being a stimulant, increases the heart rate and blood pressure, because of which some people may experience jitters.
Further, since caffeine can cross the placenta to enter the baby's bloodstream, it is thought to endanger their health.
The safe upper limit for caffeine consumption in pregnancy is still a bit hazy.
According to the current WHO guidelines, pregnant women should restrict their caffeine intake to less than 300 mg/day (approximately 2-3 cups/day).
In comparison, the World Health Organization (WHO) allows up to 400 mg of caffeine per day for non-pregnant healthy adults.
On the other hand, the NIH advises pregnant women not to consume more than 200 mg of caffeine daily.
Studies on the effects of moderate caffeine consumption (≤200mg/day) report contradictory results.
Some find an increased risk for low body weight at birth and other poor outcomes, while others report no such risk.
Yet another study reported an average of 66 grams of lower birth weights in infants born to mothers who consumed about 50 milligrams of caffeine daily.
But it's important to note that such observational studies may not separate caffeine consumption from other risk factors such as alcohol consumption and smoking.
Thus, the unfavorable outcomes in pregnancies could also be attributed to other risk factors.
The CYP1A2 gene has the largest association with caffeine-related traits as the CYP1A2 enzyme is responsible for 95% of caffeine metabolism.
The CYP1A2 gene exists in different forms in different people.
Depending on the CYP1A2 gene variant one carries, they may metabolize caffeine slowly, at a normal rate, or fast.
This, in turn, impacts a person’s risk for caffeine-associated negative side effects.
Also Read Coffee And CYP1A2: 3 Ways High Caffeine Intake Can Affect You!
AHR is another gene that influences caffeine consumption.
This gene produces an enzyme that induces the activity of the CYP1A2 enzyme.
The more the AHR enzyme, the more the CYP1A2 enzyme, and the more the tendency for increased caffeine consumption.
The ADORA2A gene is associated with the wakefulness-promoting property of caffeine.
It also influences the effect of caffeine on sleep.
The A2A receptor produced by this gene is the main target for caffeine.
Typically, a molecule called adenosine binds to the A2A receptor and helps with sleep regulation.
Upon caffeine consumption, the caffeine molecules displace adenosine molecules from their receptors and sit in their place, promoting wakefulness.
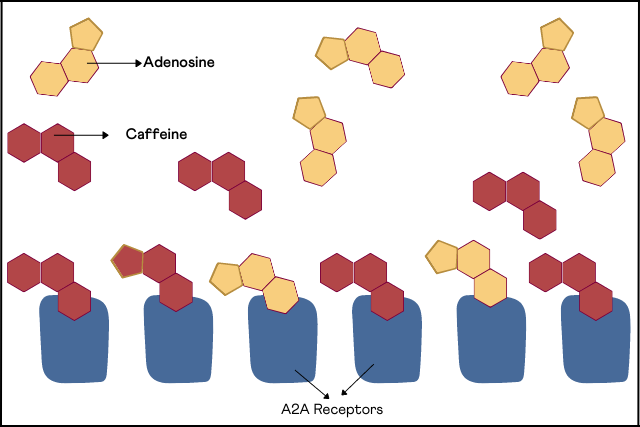
Image: Interaction of Caffeine with A2A Receptors
Certain changes in this gene increase the risk for caffeine-induced insomnia.
The study, published in the International Journal of Epidemiology, investigated a potential causal relationship between caffeine consumption and adverse pregnancy outcomes.
While many previous studies have reported an increased risk of poor pregnancy outcomes with caffeine consumption, it’s been difficult to separate coffee drinking from other risk factors.
The researchers analyzed 8 genetic changes associated with caffeine consumption.
Additionally, they examined whether these changes were associated with birth outcomes (miscarriages, stillbirths, or pre-term birth).
Genome sequencing was performed in individuals who reported these outcomes, and the results were referenced against the controls.
The study reported that there was no greater risk of miscarriage, stillbirth or premature birth for women who drank coffee.
The study looked at the effects of caffeine only in terms of adverse outcomes.
Caffeine could still affect other aspects of fetal development.
So, Dr. Moen, one of the authors of the study, says, "we don't recommend a high intake during pregnancy, but a low or moderate consumption of coffee may be safe."
Certain genetic changes influence caffeine consumption in an individual.
These changes may be why one can consume 7 cups of coffee and still go to bed by 10, and another struggles to sleep even after a couple of cups.
They affect caffeine consumption in both the general population and pregnant women.
The current recommendations for caffeine consumption during pregnancy are based on observation studies where it's difficult to separate coffee drinking from other risk factors like smoking, alcohol, or poor diet.
But caffeine alone doesn't seem to increase the risk for pregnancy-related adverse outcomes.
https://academic.oup.com/ije/advance-article/doi/10.1093/ije/dyac121/6605011#358171758
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4507998/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7209255/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6947650/
Vitamins are essential micronutrients and form an integral component of a balanced diet.
They are organic substances that are not produced by the body.
So, they are derived from the food we eat.
Vitamins are classified as:
Though several diseases are studied in association with vitamin deficiency, few people know the impact vitamins have on mental health.
Mental health illnesses are any condition or disorder that affects an individual’s mood, behavior, or thinking.
While several treatment modalities are available for treating mental health illnesses, nutrition therapy may be effective in some.
Depression is one of the most common mental health conditions and affects nearly 8% of Americans.
Deficiency of one or more B vitamins may contribute to symptoms of depression and anxiety.
Several vitamin deficiencies have been associated with anxiety and other mental health symptoms. These include:
Thiamine or vitamin B1 belongs to the B complex vitamins.
This vitamin participates in energy metabolism, cell function, development, and growth.
A study published in the International Journal of Clinical Medicine in 2011 stated that 100 mg of vitamin B1 daily in the participants improved their Hamilton Anxiety Rating Scale (HARS) scores.
The study also reported that these patients showed improved appetite and energy levels and reduced fatigue.
Vitamin B6 is also called pyridoxine and is essential for the metabolism and health of the central nervous system.
A study published in the International Journal for Vitamin and Nutrition Research in 2019 stated that low intake of vitamin B6 was associated with increased risk for mental health conditions like depression and anxiety.
The study recommended adequate intake of nutritional status of the individual, including vitamin B6.
Vitamin B12, or cobalamin, is a vital B vitamin as it plays a role in red blood cell formation and acts as a co-factor in DNA synthesis.
A deficiency of vitamin B12 results in pernicious anemia, characterized by a problem in oxygen transport in the body.
Since vitamin B12 also acts as a co-factor in synthesizing neurotransmitters like serotonin and dopamine, vitamin B12 deficiency causes symptoms like mood swings, paranoia, irritability, and confusion.
Vitamin D is a fat-soluble vitamin produced by the body on exposure to sunlight.
You can also get this vitamin via diet and supplements.
People with anxiety and other psychiatric disorders tend to have lower vitamin D levels.
Since nearly 50% of the general population is at risk of vitamin D deficiency, the risk of developing associated anxiety is also relatively high.
Vitamin C plays an essential role in mental health.
People who are deficient in vitamin C experience depression and chronic fatigue.
Studies show vitamin C improves mood, lowers stress and anxiety symptoms, and boosts cognitive function.
Image: Vitamin deficiencies that play a role in anxiety
Besides vitamins, minerals are the other essential micronutrients that may contribute to mental health conditions, including anxiety.
Magnesium is the fourth most abundant mineral in the body.
Since magnesium plays a role in optimal neurotransmitter activity and proper nervous system functioning, it affects brain function and mental health.
Research states that low magnesium levels can contribute to and aggravate neuropsychiatric conditions, including anxiety, primarily due to changes in the composition of gut bacteria.
A study found that magnesium has a calming effect as it activates the GABA (A) receptors, so this mineral is often found in anti-anxiety medications.
Iron is a trace mineral found in every cell of the body.
It is an integral part of hemoglobin, the blood pigment responsible for carrying oxygen to all parts of the body.
Iron is also a co-factor in synthesizing the neurotransmitter serotonin ( a chemical found in the brain).
A deficiency of iron has been shown to increase the risk of developing anxiety, mood, and panic disorders.
Studies have shown that people with iron deficiency have increased anxiety and fearfulness.
Zinc is another mineral that is required as a co-factor for various enzymes in the body.
It is also essential for mental health as it participates in the production of neurotransmitters and is required for the normal functioning of the nervous system.
Studies have shown that people with lower levels of zinc have a higher tendency for anxiety.
Taking zinc supplements can help reduce anxiety symptoms.
Omega-3 fatty acids are called essential fatty acids as the body does not produce them and have to be obtained through diet.
These fatty acids are vital for the normal functioning of the brain and nervous system.
Some studies have shown low levels of omega-3 fatty acids in anxious individuals, and extremely low levels correlate to severe anxiety.
Nutritional therapy uses dietary recommendations to prevent and manage anxiety.
If you are struggling with anxiety, here are a few foods that you can include in your anti-anxiety diet:
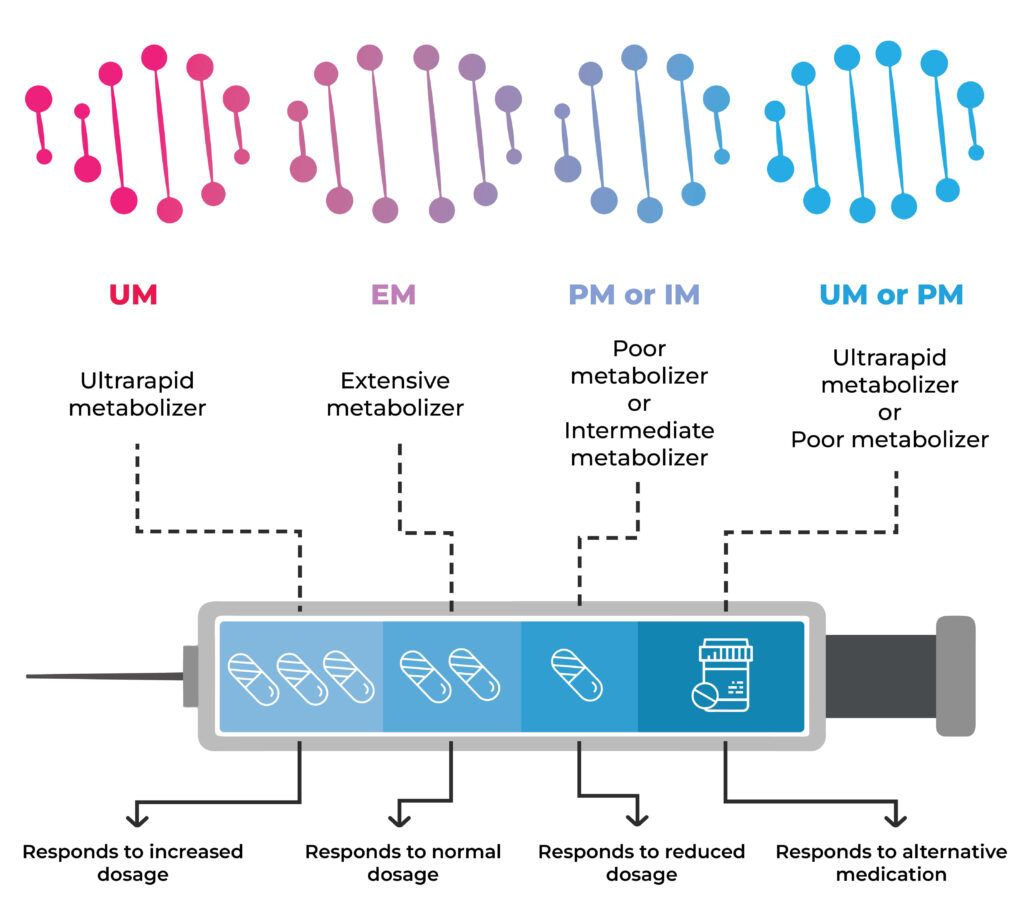
Pharmacogenetics is the study of how certain changes in the genes influence drug responses.
This can be due to variations in the genes that produce proteins or enzymes involved in drug metabolism or interaction.
This field of research is increasingly important as it allows for personalized treatment based on an individual's genetic makeup.
Why personalized treatment?
We all are similar, but of course, we are also different.
And the idea of a "one size fits all" approach to diagnostics and treatment is very flawed.
Different people respond to the same drug differently.
Because of the aforementioned genetic variants, some people may be at increased risk for adverse drug reactions (ADRs) for certain medications.
Others may not experience the desired effect of the drug because they clear it from their body too quickly.
Pharmacogenetic information can help identify medications best suited for a particular person.
It can also factor in when clinicians choose the appropriate dosage for individual patients.
In clinical trials, pharmacogenomics can help identify new targets for drug development.
The benefits of knowing how you'll respond to a medication or which drug will work best for you before you even consume it are not hard to imagine.
One of the popular choices of mental health providers for treating anxiety is psychiatric medications.
Implementing pharmacogenomics here lowers the room for trial and error.
It can also help discover what drugs could potentially cause ADRs in an individual.
The pharmacogenomic approach also helps lower the economic burden as less, or no money will be wasted on drugs that aren't effective for an individual.
Some key players in anxiety medications fall into the following categories:
Serotonin Reuptake Inhibitors (SSRIs): SSRIs, originally designed to treat depression, have revolutionized the treatment of anxiety. They work by blocking serotonin (happy hormone) reuptake, thereby increasing its availability for nerve signaling.
Changes in the CYP2C19 gene link to differences in the metabolism of SSRIs.
People who are ultrarapid metabolizers may not experience the therapeutic effects of the drugs due to their quick elimination from the body.
In contrast, poor metabolizers may have a build-up of the medication in the body and experience side effects, some of which may be adverse.
Tricyclic Antidepressants (TCAs): Physicians use TCAs to treat panic disorder, PTSD, anxiety, and depression that occurs with anxiety. They act on 5 brain chemicals (or neurotransmitters). They block the reuptake of serotonin and norepinephrine.
Changes in the CYP2D6 and CYP2C19 genes affect TCAs' exposure time, effectiveness, and safety.
Other medicines used to treat anxiety, like benzodiazepines and serotonin norepinephrine reuptake inhibitors (SNRIs), also have a pharmacogenomic aspect.
Having this information in hand provides many benefits.
Genetic testing for psychiatric medications is a pretty straightforward procedure.
The DNA raw data (the particulars of your DNA in text format) is obtained through a saliva or cheek swab sample.
The raw data is then matched against a database that contains information about the gene changes influencing drug metabolism.
For each drug, the sample DNA data is referenced against the database, and depending on the genetic changes, the metabolizer classification (slow, moderate, normal. Rapid, ultrarapid) is entered.
This report can then be interpreted with the guidance of a qualified medical practitioner and used to understand which drug may work the best for you.
The overall efficacy of genetic testing has improved by leaps and bounds over the years.
However, no genetic test for psychiatric medications has a 100% effectiveness rate.
Genetic testing for medication can be quite expensive.
Studies have found that people would be more inclined to have the test done if the costs were lower or covered by insurance.
A 2017 survey conducted in Singapore reported cost as the biggest concern for pharmacogenomic testing, with over 94% of respondents concerned about cost.
The main concern for mental health practitioners about implementing genetic testing for psychiatric medications is the lack of pharmacogenomic knowledge.
In a survey conducted on psychiatric pharmacists in the US (2015), half of them reported being completely or partially unaware of pharmacogenomics.
Another main concern in employing pharmacogenomics in clinical practice seems to be a lack of clear guidelines about using genetic test results in prescribing psychiatric medications.
Currently, most reports adopt a “traffic light” style for displaying the results.
This leads to a wrong interpretation of ‘green meaning the drug will work’ and ‘red, the drug won't.’
Both clinicians and patients may misinterpret the results.
Alcohol is one of the most commonly used substances globally and has been linked to a wide range of negative consequences.
It can harm mental health, including increased risk for anxiety, depression, and other mental illnesses.
Understanding the relationship between alcohol and mental health is important because it can help reduce the prevalence of these conditions and improve people's lives.
Alcohol can exacerbate anxiety in several ways.
Alcohol causes a temporary spike in heart rate and blood pressure.
Chronic consumption of alcohol can lead to ongoing increased heart rate and blood pressure, weakened heart muscles, and irregular heartbeat.
A Sneak-peek Into the Gene Health Report
Neurotransmitters are brain chemicals.
Alcohol consumption interferes with neurotransmitter levels, throwing your body out of balance.
For example, GABA is a neurotransmitter that reduces energy levels and calms your body down.
When alcohol increases the GABA levels, the sedation effects are amplified, causing wobbly walking and speech slurring.
Alcohol also increases dopamine levels, stimulating the brain's reward centers, thus tricking you into thinking alcohol is pleasurable.
Thus, alcohol consumption throws your neurotransmitter levels off balance, thereby worsening your activity.
Alcohol can induce feelings of relaxation and sleepiness; however, excess consumption can lead to poor sleep quality.
Alcohol is a depressant and results in quick sleep onset. So, people fall into deep sleep quicker, creating an imbalance in the stages of sleep.
This decreases the overall sleep quality, making anxiety management difficult.
Alcohol affects how nerves communicate with each other in a region of the brain called the hippocampus.
The hippocampus plays a role in memory formation.
Alcohol slows down the normal nerve activity here, thereby worsening short-term memory.
This can be very unsettling, even more so for people with anxiety.
Hangxiety is hangover-related-anxiety.
It describes the significant increase in anxiety one may experience after a night of heavy drinking.
Everyone may not experience this.
People with existing anxiety or social phobia are more prone to it.
There are a few hypotheses on why hangxiety happens.
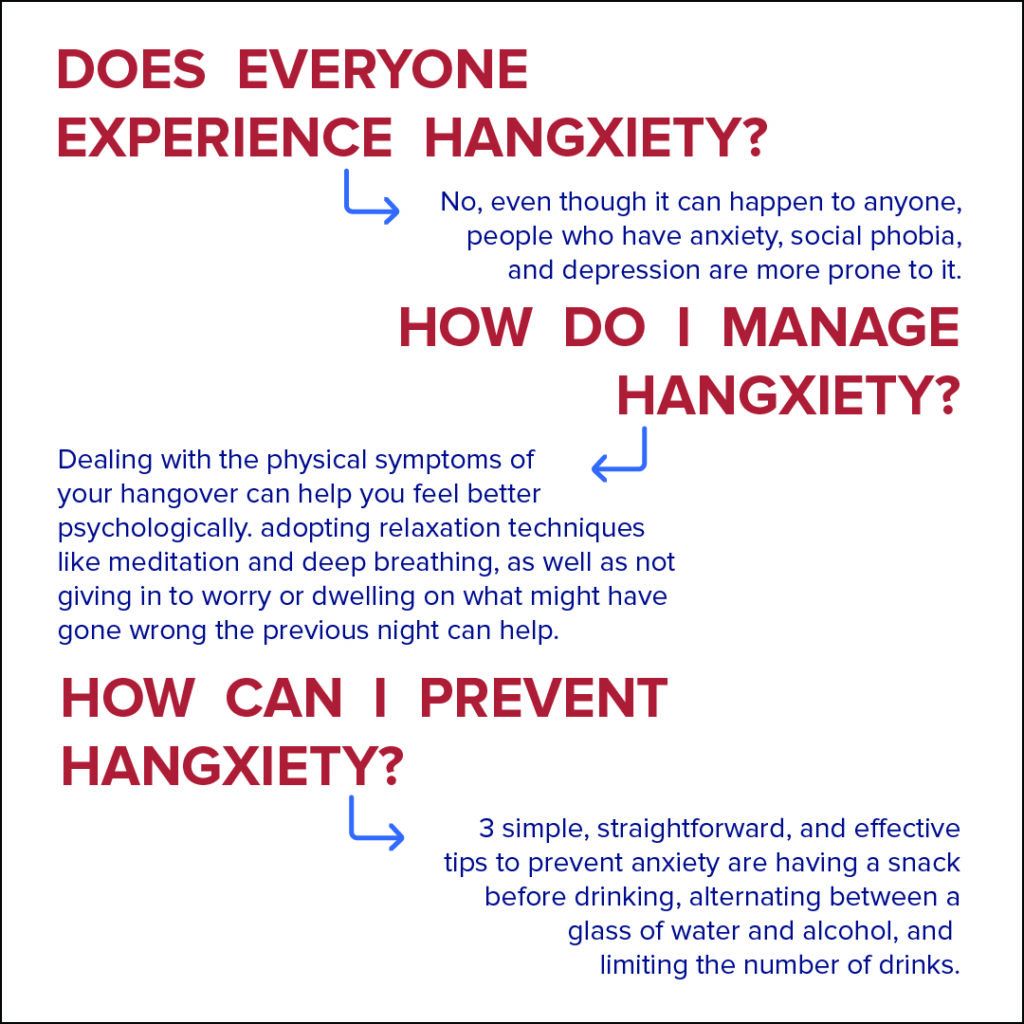
Image: Hangover and Anxiety - Hangxiety Management
For people with anxiety, a few drinks may help them relax.
But alcohol can also make anxiety worse in some people.
Here’s how:
While alcohol may initially relieve anxiety symptoms, they return once alcohol is eliminated from the body.
Over time, the more you drink, the more alcohol it'll take for your body to be in a relaxed state.
This tolerance build-up can put a person at dangerous risk for alcohol addiction.
Anxiety is a normal reaction to stress, but it can interfere with daily life when it becomes excessive or disabling.
There are many ways to manage anxiety; here are a few tips to get started:
https://www.healthline.com/health/alcohol-and-anxiety
https://www.sleepfoundation.org/nutrition/alcohol-and-sleep
https://www.medicalnewstoday.com/articles/hangover-anxiety
Anxiety is a normal emotion that may cause you to sweat, feel restless or helpless, and have a rapid heartbeat.
It is a feeling of uneasiness, fear, or dread.
Most people experience anxiety at some point in their lives.
However, if you have anxiety that does not go away or only worsens with time, you may have an anxiety disorder.


There are different types of anxiety disorders, the most common ones being:
Anxiety is caused due to a complex interplay between different factors, including:
Some factors that may increase the risk of developing anxiety are:
Some common symptoms of anxiety disorder are:
Genetics plays a significant role in anxiety and panic disorder.
A family member with anxiety disorder increases one’s risk of developing the condition.
Several studies conducted over the past few decades have reported a genetic association with anxiety. Some key highlights include:
Anxiety does have a genetic component but is influenced by environmental and social factors.
This means that having a family history of anxiety disorder does not confirm you will develop the condition.
It is also possible to develop anxiety disorder without it running in your family.
Monogenic diseases are caused when mutations or abnormal changes in a single gene are inherited by the Mendelian model of inheritance.
A complex interplay between several genes and external factors contributes to the development of anxiety disorders. For this reason, anxiety disorders are said to have a polygenic etiology (caused by multiple genes).
Single nucleotide polymorphisms or SNPs in the following genes have been studied for their association with anxiety disorders:
Those carrying mutations in these genes and subjected to environmental stressors are at higher risk for anxiety than those without the mutations.
Gene-environment interactions emphasize the complex nature of anxiety and its related disorders.
Also Read: Cracking the Anxiety Code Using your DNA Raw Data
Anxiety and anxiety disorders can be treated using medications and counseling.
Treatment options for anxiety include:
The most commonly used medications in the treatment of anxiety disorder are:
This therapy is usually done by a trained psychologist and involves helping you learn about how your emotions affect your behavior.
During psychotherapy, the mental health professional guides you to understand and manage your feelings and fears.
Cognitive-behavioral therapy (CBT) is the most commonly used psychotherapy for anxiety disorder.
Some lifestyle changes to help you manage symptoms of anxiety disorder are:
Anxiety disorders are chronic and cannot be completely cured.
However, with the effective treatment mentioned above, people can manage their symptoms and learn to cope better.