Losing hair can be a distressing experience, with many potential causes, including hormonal imbalances, genetics, and nutritional deficiencies.
One nutrient linked to hair health is magnesium, a mineral that plays a vital role in many bodily functions.
However, can magnesium deficiency lead to hair loss, and if so, what can you do about it?
In this article, we'll take a closer look at the connection between magnesium deficiency and hair loss, the role of magnesium in the body, and what steps you can take to prevent or address a potential deficiency.
Did You Know? Your genes influence how much your body absorbs and utilizes magnesium from food. Certain gene changes can increase your risk for magnesium deficiency. Learn more. Learn more.
Magnesium is an essential micronutrient that is required by the body to perform several functions.
This mineral participates in:
Low magnesium levels result in a deficiency of the mineral.
While magnesium deficiency is rare, it may be caused by:
7 Most Significant Magnesium Benefits For Men
Magnesium plays a central role in protein production in the body, which governs various processes like cell division, growth, and maturation.
It has also been found to play a vital role in immunological and inflammatory reactions in the body.
Due to these functions, magnesium, directly and indirectly, affects hair growth and health.
A deficiency of magnesium can disrupt protein metabolism and alter immune response, both of which can cause hair loss.
Magnesium and hair growth has a strong association, as the mineral affects hair follicle growth and the overall growth cycle.
Magnesium prevents calcium build-up in the scalp - this restores blood flow back to the hair follicles.
It has been suggested that magnesium’s role in protein synthesis may affect hair growth.
The Recommended Dietary Allowance for magnesium is around 320 mg daily for females and 420 mg daily for males.
Consuming magnesium-rich foods like bananas (which contain around 32 mg of magnesium) is great for hair loss.
There are different types of magnesium compounds used in varying products.
Magnesium citrate and magnesium glycinate are the two most common magnesium salts for managing its deficiency.
Both these salts have excellent bioavailability and do not trouble the digestive system.
One of the best ways to use magnesium for hair loss is hair oil containing the mineral.
You can use magnesium hair oil once you have consulted your dermatologist and determined if it is safe and effective for your hair loss.
Magnesium hair oil offers several benefits:
Have you ever wondered why some people seem plagued by allergies while others breeze through life without a sneeze?
Are allergies merely a matter of chance, or is something deeper at play?
As we are nearing the halfway mark of 2023, a new wave of scientific revelations is reshaping our understanding of this intricate relationship.
This article explores the fascinating discoveries that shed new light on the age-old question: "Are allergies genetic?"
Genetic ancestry tests are becoming increasingly popular. While your DNA can be used to learn about your roots, did you know that it can also reveal important things about your health risks and wellness aspects? This allows you to take proactive measures for health conditions, even before the symptoms appear, thereby preventing it. You can upload your DNA data to learn 1,500+ things about your health. Learn more.
Allergic reactions happen when our body's defense system, called the immune system, gets confused.
Normally, the immune system protects us from harmful things like germs.
Sometimes it overreacts to things that are harmless, like pollen, dust, or certain foods.
When our body encounters one of these harmless things, it can trigger a response where our immune system tries to fight it off.
Our immune system produces special substances called antibodies, specifically one type called IgE. These antibodies attach themselves to certain cells in our body called mast cells.
The next time we come into contact with that same harmless thing, the antibodies on the mast cells recognize it and send signals to release chemicals like histamines.
These chemicals cause the symptoms we associate with allergies, such as sneezing, itching, and swelling.
Scientists are still studying allergies to understand why our immune system reacts this way and how we can prevent and treat allergies better.
It's an ongoing puzzle that they're trying to solve to help people who have allergies feel better.
Allergies can be grouped into several common types based on what triggers them. Here are some of the most common types of allergies:
It's important to note that individuals can have multiple allergies or different sensitivities to various allergens.
If you suspect you have an allergy, it's advisable to consult with a healthcare professional for proper diagnosis, management, and advice on avoiding triggers.
Research suggests that genetics can play a significant role in determining a person's susceptibility to developing allergies.
Studies have shown that if one or both parents have allergies, their children are also more likely to have allergies.
Having one biological parent with an allergy increases the risk for the child by 50%; when both parents have allergies, the risk jumps to 75%.
This familial pattern indicates a potential genetic component.
Genes regulate the functioning of the body's immune system, which plays a crucial role in recognizing and responding to allergens.
Changes in certain genes involved in immune system regulation and the production of antibodies, such as immunoglobulin E (IgE), have been identified as potential contributors to an increased risk of allergies.
These changes can make individuals more prone to mounting an allergic response when exposed to allergens.
However, it's important to note that genetics alone do not fully determine whether someone will develop allergies.
Environmental factors also play a significant role.
Exposure to allergens, such as pollen, dust mites, pet dander, or certain foods, is essential for an allergic reaction.
Environmental factors can interact with genetic factors, triggering or worsening allergies in susceptible individuals.
Ongoing research aims to unravel the intricate relationship between genetics and allergies, shedding light on the specific genes and mechanisms involved.
This knowledge could lead to improved understanding, prevention, and treatment strategies for allergies in the future.
HLA Gene And Allergies: The Ever-Evolving Love Story
Certain allergies have a hereditary component, which can be passed down from parents to children. Here are some examples:
Recent research on allergies has yielded significant insights into the development and management of allergic conditions.
Anaphylaxis is a life-threatening allergic reaction. Researchers from Indiana University School of Medicine have found a way to block this reaction to peanuts.
The experiment has been carried out successfully in an animal model.
The researchers have developed an inhibitor called cHBI that specifically binds to molecules known to elicit immune responses.
This cHBI is specific to treat allergic reactions to peanuts.
However, this inhibitor is yet to be tested on humans.
This year has witnessed an increase in the number of adults in their 30s, 40s and 50s experiencing allergic symptoms to seasonal allergens like pollens.
An interesting thing to note here is that most of them never were allergic to these components before - this condition is called adult-onset allergies.
One of the biggest contributors to this is climate change!
It has resulted in 20% more pollen in the air and added 3 more weeks to pollen season compared to 30 years ago.
The combustion of fossil fuels is only adding to this problem.
With increased carbon dioxide emissions, plants and trees are producing more pollen.
Many people have genetic predispositions (risk) to allergies but have never had to deal with the symptoms since the allergy was "dormant."
However, the increased pollen count and pollen season duration seem to have triggered allergic reactions by overloading the immune system.
The two primary methods are skin tests, which involve applying allergens to the skin and observing for reactions, and blood tests that measure the levels of specific antibodies like immunoglobulin E (IgE).
This may involve making changes to the living environment, such as using dust mite-proof covers, removing pet dander, or avoiding specific foods.
It can be administered through injections (allergy shots) or sublingual tablets/drops.
It's crucial to consult with healthcare professionals for accurate diagnosis, personalized treatment plans, and guidance on managing allergies effectively.
Treatment approaches may vary depending on the specific allergy, its severity, and individual circumstances.
Have you ever pondered the effects of alcohol on your blood pressure? While many know that excess alcohol does raise blood pressure, what about moderate or occasional consumption? Is there a safe threshold for alcohol intake concerning heart health? In this informative exploration, we delve into the latest research on how alcohol raises blood pressure and unveil strategies to mitigate risk factors.
Did You Know? Your genes influence how your body processes alcohol and your risk for being an alcohol dependent. You can use your ancestry test DNA data to learn everything from disease risk and drug sensitivities to nutritional requirements and fitness parameters. Learn more.
Yes, alcohol does affect blood pressure through various mechanisms. Let's explore these in detail:
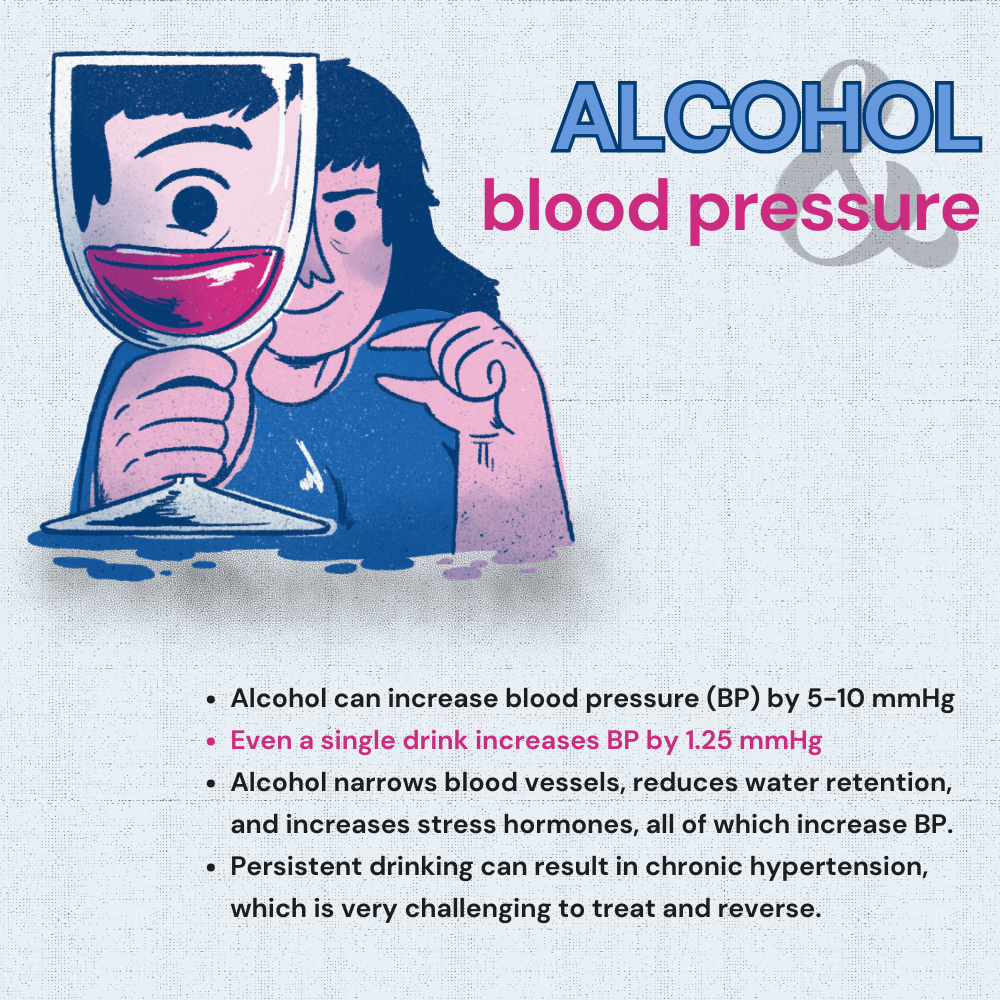
The impact of alcohol on blood pressure is notable among heavy drinkers, typically resulting in an average increase of 5 to 10 millimeters of mercury (mmHg).
Importantly, the rise in systolic blood pressure (during heartbeats) is usually greater than in diastolic blood pressure (during rest between beats).
A comprehensive study involving 19,000 adults in the US, Korea, and Japan found a connection between alcohol consumption and higher blood pressure.
This groundbreaking research combined data from seven diverse international studies between 1997 and 2021. Crucially, none of the participants had been previously diagnosed with high blood pressure (hypertension) or related conditions, ensuring a clean starting point.
The study found that even moderate alcohol consumption is linked to higher systolic and diastolic blood pressure. Systolic pressure rose by 1.25 mm Hg with 12 grams of daily alcohol, increasing to 4.9 mm Hg at 48 grams. Diastolic pressure rose by 1.14 mm Hg at 12 grams and 3.1 mm Hg at 48 grams.
Importantly, this effect was more pronounced in males than females.
This research highlights that even a low level of alcohol consumption can increase blood pressure.
No health benefits were found with moderate consumption. This may heighten the possibility of experiencing cardiovascular events.
While these findings are significant, it's essential to consider certain limitations. The study relied on self-reported alcohol consumption, which can introduce recall bias.
Additionally, the research spanned five years, possibly not capturing longer-term effects accurately.
Determining how much alcohol is too much involves considering various factors, including individual tolerance, gender, and the pattern of drinking.
The instructions from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) provide significant considerations.
Binge drinking: This is a pattern of alcohol consumption that elevates blood alcohol concentration (BAC) to 0.08 percent or higher. This typically equates to:
Heavy alcohol use: Heavy alcohol consumption is defined as follows:
The American Heart Association (AHA) advises that if you consume alcohol, you should limit your intake to no more than 2 drinks per day for males and 1 for females when managing blood pressure.
It's important to understand what constitutes a standard drink:
Exceeding these limits can increase blood pressure.
Managing blood pressure involves lifestyle changes and medical interventions.
Here's a breakdown of key strategies to manage risk factors, including the impact of alcohol on blood pressure:
Do's:
Don't:
In addition to the above, consider these steps to reduce the risk of high blood pressure further:
Can Alcohol Consumption Lead To Hypothyroidism?
Alcohol does raise blood pressure, even with as little as one drink.
It affects through mechanisms like narrowing blood vessels, reducing water retention, increasing stress hormones, and altering baroreceptor sensitivity.
Heavy alcohol consumption can cause a noticeable increase in blood pressure, especially in the systolic reading during heartbeats.
Recent research indicates a relationship between alcohol and high blood pressure, even in people who have never had hypertension.
The study underlines that moderate alcohol consumption can lead to higher blood pressure levels, especially in males.
The American Heart Association advises limiting alcohol to no more than 2 drinks daily for males and 1 for females.
Alongside moderation, a balanced diet, regular exercise, weight management, and stress reduction are essential for blood pressure control.
Regular monitoring and managing related health conditions, such as diabetes and high cholesterol, are also vital to reducing the risk of high blood pressure.
https://www.medicalnewstoday.com/articles/alcohol-and-blood-pressure
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4038773/
https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking
https://www.who.int/news-room/fact-sheets/detail/hypertension
In today's fast-paced world, stress has become an unavoidable companion for many, leading to a surge in the search for natural remedies that can aid in managing it. Enter adaptogenic mushrooms, renowned for their potential to balance, restore, and protect the body. While the idea of using mushrooms for health isn't new—ancient cultures have revered them for millennia—it's their modern promise of ushering in a stress-free life that's capturing attention. In this article, we delve deep into the world of adaptogenic mushrooms, exploring their potential and unveiling if they truly hold the key to a stress-free life.
Did You Know? Your ancestry test DNA data includes 700,000 markers, which can be used to learn about a very important stress gene called COMT which influences if you respond like a "warrior" or "worrier" to stress.
Order Your Personality Report Today!
An adaptogen is any plant substance or herb that may help your body cope with stress, anxiety, or fatigue.
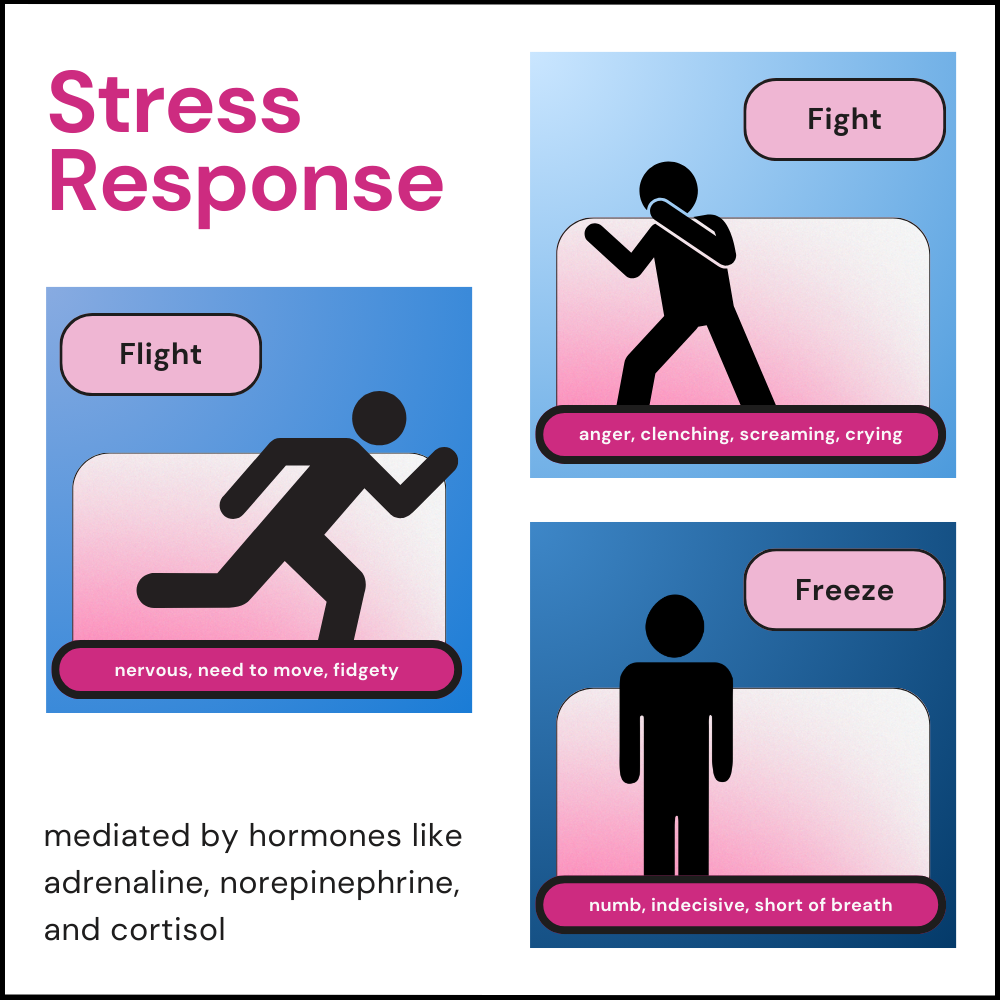
When a person is stressed, the body’s Hypothalamic-Pituitary-Adrenal (HPA) axis releases glucocorticoids as a response.
Cortisol is one of the significant glucocorticoid hormones released during stress, and this causes the flight-fight-freeze response during a stressful phase.
Consistently high levels of cortisol affect every organ in the body and increase the risk of the following:
Specific active ingredients in adaptogens act to bring down cortisol levels when they are high.
The main goal of adaptogens is to maintain a state called homeostasis in the body.
Homeostasis is a state where the living being's physical, chemical, and social conditions are optimally maintained.
In other words, the body and mind are stable and function as they are meant to, without disruptions or instabilities.
One of the most popular types of adaptogens is mushrooms.
Adaptogen mushrooms aren’t ‘magic mushrooms’ that affect the brain and cause psychedelic effects.
Inversely, adaptogen mushrooms work on the body and create resistance against the adverse effects of stress.
These mushrooms help balance homeostasis by affecting the functioning of the HPA axis and reducing the effects of stress hormones.
The following are a few varieties of adaptogenic mushrooms available.
Cordyceps is a type of mushroom that grows in high altitudes.
These fungi grow on insects' larvae, and more than 400 types of these fungi are identified.
Two of them are of significant interest - Cordyceps sinensis and Cordyceps militaris.
Cordyceps may have adaptogenic properties.
A 2014 study reported that consuming 600 mg of cordyceps/day for two weeks helped improve stress response and fatigue in high-altitude trainers.
Reishi is an adaptogenic mushroom known for its ability to improve the immune system and help handle stress.
A 2020 study on rodents reports that reishi may help treat stress-induced brain inflammation and prevent brain damage.
A 22013 study on rats reported that reishi mushrooms may have anxiolytic characteristics (the ability to reduce stress) and may help reduce stress-induced anxiety symptoms.
Lion’s mane, scientifically called Hericium erinaceus, is another type of mushroom known for its adaptogenic properties.
A 2018 study reports that Lion’s mane mushrooms produce antidepressant-like effects in rodents.
According to experts, these mushrooms help stabilize brain-derived neurotrophic factor (BDNF) levels in rodents.
Stress and depression are the two leading causes of low BDNF levels.
Turkey tail, or Trametes versicolor, is a beautiful-looking mushroom with various colors.
Prolonged high cortisol levels may lead to an increased amount of reactive oxidative species (ROS) in the cells and lead to oxidative stress.
Oxidative stress causes DNA level damage to the cells and is one of the significant causes of cancers.
A 2017 study reports that the turkey tail mushroom may have up to 35 phenolic compounds, including flavonoids.
These phenolic compounds help combat oxidative stress in the cells and inflammation in the body.
No. all mushrooms aren’t adaptogenic. You will need to choose the right ones to get the adaptogenic benefits.
The following are some of the benefits of adaptogenic mushrooms.
Is It Possible To Measure Stress?
While adaptogenic mushrooms are edible, the tolerance towards them varies with different individuals.
According to nutritional experts, cordyceps and reishi mushrooms are safer and can be tolerated by most people.
Some of the possible side effects of consuming cordyceps or reishi are:
Lion’s mane mushrooms are also safe when consumed in moderation.
Possible side effects include:
Turkey tail mushrooms may also cause gastric troubles, vomiting, and darker fingernails in a few.
Please consult your doctor if you are trying an adaptogenic mushroom or its supplement.
It is safer to start with a low dose and observe the changes in your body.
If fresh adaptogenic mushrooms are available, you can buy and use them while making your meals.
If not, adaptogenic mushroom powders are available in plenty.
Adaptogenic supplements are also available as capsules or pills on the market.
While choosing these supplements, look for the following features.
Please make sure to talk to your healthcare provider before you decide to try adaptogenic mushrooms.
While few human studies confirm the adaptogenic features of some mushrooms, this is a common ingredient trusted and used in many Asian traditional medicine practices.
Some mushrooms help the body cope with stress and fatigue when consumed right.
Please talk to your healthcare provider if you want to try them out.
Out of all the adaptogenic mushrooms, reishi mushrooms are more commonly used because they are better tolerant and may have holistic benefits to the body.
Adaptogenic mushrooms may lower blood pressure levels. They can also interact with blood pressure medications.
People on hypertension medications must consult their doctors and get approval before trying adaptogenic supplements.
These adaptogenic mushrooms may not be tolerated well by everyone. Some side effects of these mushrooms are gastrointestinal issues, headaches, dizziness, and nausea.
Consuming in excess may make these symptoms severe.
The following individuals aren’t recommended to use adaptogenic mushrooms.
https://pubmed.ncbi.nlm.nih.gov/14714963/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5855563/
https://www.nature.com/articles/s41598-020-65812-5
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4174424/
https://www.apa.org/news/press/releases/stress/2022/concerned-future-inflation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6240259/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6010034/
https://www.tandfonline.com/doi/abs/10.1080/10538712.2016.1123790
https://pubmed.ncbi.nlm.nih.gov/34375514/
https://pubmed.ncbi.nlm.nih.gov/24369991/
The next time you pick up a paper straw and sip your bubbling soda or some water, you may want to be aware of unintentionally ingesting minuscule portions of harmful synthetic chemicals into your body. Recent studies show that paper straws, once considered safer for both the environment and health, may have higher levels of the forever chemicals (poly-and perfluoroalkyl substances (PFAS)) than plastic straws. Keep reading to know more about PFAS and how to stay protected from PFAS toxicity.
The world has become more conscious of sustainable and eco-friendly alternatives over time.
More people worry about how their actions affect the environment and choose to pay premium prices on bio-degradable, organic, and reusable products that are biodegradable.
One such change we see everywhere is the preference for paper straws over plastic ones.
Paper is bio-degradable and disintegrates quickly when dumped in landfills.
Conversely, plastic takes 500 and 116 years, respectively, in land and marine environments to degrade.
Many countries like Australia, Brazil, the UK, and Canada have existing single-use plastic straw bans and encourage the use of paper straws in business places.
So, it definitely makes more sense to switch to paper straws.
Recent studies think otherwise, though.
Compared with bamboo, glass, steel, and plastic straws, paper ones had 90% of poly-and perfluoroalkyl substances (PFAS) content.
PFAS are synthetic chemicals harmful to living beings and the environment.
Paper straws are generally made of food-grade paper, adhesive, dyes, and liquid-resistant coatings.
Three-ply paper is immersed in an adhesive bath and sent into a wounder machine that winds them into thin cylindrical shapes.
Since paper absorbs water quickly and disintegrates, all paper straws are coated using polyethylene (PE) or acrylic resin.
These coating materials could be toxic, laden with chemicals, and unsafe for people and the environment.
Forever chemicals are named adeptly for their inability to disintegrate.
This group of chemicals doesn’t break down in the bodies of living beings or the environment. They aren’t affected by heat, water, or other chemical agents.
These chemicals have the potential to live forever in the world.
These are found in everyday products like clothes, cosmetics, hair products, plastic kitchenware, and toilet paper.
PFAS are forever chemicals.
Poly-and perfluoroalkyl substances are a group of over 15,000 synthetic chemicals used in various production stages of everyday-use products.
PFAS have strong carbon-fluorine bonds that make them harder to break down. Over time, PFAS can leak into water, soil, and air.
Two of the significant sources of PFAS are:
Taylor & Francis Group, a UK-based publishing company, released an analysis in August 2023.
This study compared the levels of PFAS in thirteen brands of straws available commonly in the country.
Paper straws have always been considered a more eco-friendly alternative to plastic straws.
These are also cheaper to produce, causing them to take over the straw production industry quickly.
However, when the levels of PFAS in different types of straws were analyzed, the researchers found that paper straws had the highest levels of toxic PFAS.
Analysts in Belgium tested 39 brands of straws available in Europe for the presence of PFAS.
Five categories of straws were included in the study - paper, glass, plastic, bamboo, and stainless steel.
The samples were obtained from regular places like supermarkets, fast-food chains, and shops.
All the samples went through two rounds of PFAS testing.
The researchers reported that 69% of all straws (27 out of 39 samples) tested positive for PFAS.
The primary type of PFAS found in these samples was PFOA.
PFOA has been banned globally since 2020.
The researchers also reported the presence of water-soluble PFAS like trifluoroacetic acid (TFA) and trifluoromethanesulfonic acid (TFMS) in the straws.
These water-soluble PFAS can quickly leach into the drinks from the straw and get ingested.
According to these experts, PFAS may make the straws more water-resistant.
However, this isn’t proven yet.
The contamination could also occur from the soil and water used to grow the plant or during manufacturing.
The kind of adhesive used could also contribute to PFAS exposure.
This study points to the fact that the levels of PFAS noticed were low.
Since people use straws only occasionally, the levels may not be enough to cause toxic damage immediately.
However, PFAS doesn’t break down in the body. Minimal levels of ingested PFAS can also lead to excess build-up over time.
There are two limitations to this study.
A similar study was published in 2021, analyzing the presence of PFAS in plant-based straws.
Five plastic, 29 paper, and nine other plant-based straws were analyzed.
The study reports that no PFAS were identified in the plastic straws. The paper and plant-based straws, however, tested positive for 21 kinds of PFAS.
Perfluorooctanoic acid (PFOA), perfluorobutanoic acid (PFBA), and perfluorohexanoic acid (PFHxA) were the major PFAS identified.
The following are some other sources of forever chemicals in everyday life.
According to experts, the average consumer may not be able to stay away from forever chemicals because they are everywhere completely.
However, here are some ways to stay protected.
According to this study, all types of straws except stainless steel pose the risk of having PFAS.
It is best to carry a few stainless steel straws and use them whenever needed. These straws can be reused multiple times and are safer than paper straws.
Another easier option would be to avoid straws altogether.
https://www.sciencedaily.com/releases/2023/08/230825122044.htm
https://pubs.acs.org/doi/10.1021/acssuschemeng.9b06635
https://www.niehs.nih.gov/health/topics/agents/pfc/index.cfm
https://www.cdc.gov/biomonitoring/PFAS_FactSheet.html
https://www.sciencedirect.com/science/article/abs/pii/S0045653521007074?via%3Dihub
https://www.fda.gov/food/process-contaminants-food/questions-and-answers-pfas-food
https://www.sciencedaily.com/releases/2023/08/230825122044.htm
https://nypost.com/2023/08/25/paper-straws-more-toxic-than-plastic-study/
Human genetics has fascinated scientists since time immemorial.
In recent years, understanding human genetics has led to the development of medications for many previously incurable diseases.
However, there is a particular facet of these studies that we need to consider.
Who participates in genetic studies, and who does not?
Could these biases affect the study results?
And most importantly, are our genes responsible for such a bias?
We answer all these questions here.
Genetic research analyzes human DNA to identify genes that can cause diseases.
Most health conditions have a genetic component.
They can be either entirely genetic or can be a mix of genetics, lifestyle, and environment.
There are around 25,000 genes that make up the human body.
Genes are made up of DNA.
The DNA has specific codes that determine how a gene works.
When this code is altered, the functioning of a gene changes.
Sometimes, this change can be in a single letter called Single Nucleotide Polymorphism or SNP for short.
Most SNPs don't cause any health issues.
However, the effects of a few or several SNPs put together can contribute to disease risk.
In genetic research studies, scientists aim to find out the exact genetic and environmental contribution to each disease.
Genetic studies can be of different types.
They can involve small or large groups of people or even individuals.
The following are some types of genetic studies.
Research involving families
This type of genetic study is also known as linkage analysis.
Common diseases like autism, Alzheimer's, and cancer affect many individuals worldwide.
1 out of every 110 children will develop autism, while 1 in 10 and 1 in 3 adults will develop Alzheimer's and cancer, respectively.
Often, these diseases run in families.
More than one individual in the family is usually affected by the disease.
When such families are involved in genetic research, scientists can discover the specific gene mutation responsible for the disease.
The region where this mutation is prevalent can also be more specifically identified.
It will better our understanding of these diseases and can assist in developing treatment options.
Research involving large groups of people
This type of genetic study is called association.
In this study, two groups of people are chosen for DNA testing.
One group usually has a disease, while the other group, called the control, does not
Scientists study the SNPs present in the participants.
Sometimes, one type of SNP is found more frequently in people suffering from certain diseases like Alzheimer's.
This variation can be identified in an association study.
This type of research requires the participation of many people.
Research involving candidate genes:
Candidate genes are located on specific DNA parts associated with certain diseases.
Researchers will examine these genes to determine how they contribute to a disease.
A groundbreaking study by Oxford’s Leverhulme Center for Demographic Science and Big Data Institute showed that people participating in genetic studies are more genetically likely to do so.
Currently, genetic studies are conducted using genetic databases containing information on a large population.
However, using this data can lead to what is called an ascertainment bias.
Ascertainment bias occurs when some people are more likely to be included in the study than others, resulting in the representation not reflecting the intended study population.
For example, imagine you are conducting a study on school students to find out the favorite hobbies of 6-12-year-olds. You go into the art class and ask the students there. You likely would have gotten answers like painting, drawing, etc. If you conclude that the favorite hobby of your target population is painting, your answer is clouded by ascertainment bias since those with painting as a hobby are overrepresented in your study population.
The researchers used the UK Biobank, one of the world's largest biomedical databases, to study the connection between genetics and participation bias in genetic studies.
They found that some people have certain gene changes that make them more likely to join these studies.
Professor Kong says this could lead to ascertainment bias since sometimes, only certain types of people join, which can make the study's results a bit off.
Therefore, the genetic data collected from studies might not represent the intended study population.
Genetic research is based on extensive data collection from many people.
However, if only some people participate and others don't, it can lead to inaccurate results.
The study further reported that the genetic trait influencing participation has a 36.6% correlation with the genetic factors underlying educational attainment.
This means there's a link, but participation isn't merely a result of traits like education or body mass index.
The genetic inclination to participate in studies can be inherited, potentially impacting individuals' participation in various studies throughout their lives.
This discovery underscores the need to consider such biases when designing and analyzing genetic research.
Genetic studies offer essential insight into the relationship between genetics and human health.
They help scientists understand how particular genes or specific mutations can cause diseases.
These studies are vital for developing effective medications against some commonly occurring diseases.
However, participation bias can affect the study results.
If only some people participate, the results might not represent the intended study population.
Surprisingly, these biases can run in families.
They can affect people's participation in different studies over their lifetime.
Thus, accounting for this bias is necessary for accurate results from genetic studies.
By accounting for these biases, the results of genetic studies might be complete.
Common diseases like cancer and Alzheimer's run in families.
They are caused by a genetic mutation that can be passed down through generations.
It is where genetic research steps in.
These studies help identify the gene mutations that cause these diseases.
Understanding the nature of these diseases can help develop treatments and medications.
However, a new study has shown that only some people participate in genetic studies.
Genes determine if a person will ever participate in genetic studies in their lifetime.
This phenomenon can give rise to participation bias.
This means the data collected will not represent the intended population and will show inaccurate results.
Understanding who participates in genetic research will help scientists consider such biases.