Spit. Seal. Send.
Thanks to the advent of technological innovations, anyone can now buy a genetic test from the comfort of their homes. With these three simple steps, everyone can learn a world of information from their genomes. But despite the many disclaimers and caveats direct-to-consumer genetic testing (DTC-GT) companies put forward, many users can fail to understand their limitations. This begs the question, “is there a downfall to having such easy access to all of the information in our genomes?”
Before going on to genetic testing, let's delve a bit into genetics.
DNA is the blueprint of your body - almost everything about it, from how tall you are to when you are likely to go bald.
Around 3 billion individual letters organized into 23 pairs of chromosomes make up this blueprint.
These letters are arranged in a specific way; some can be used to diagnose a rare disease or provide information about a person's risk of developing a disease.
Some arrangements have clinical significance and may give consumers insight into monitoring their health or potential disease or conditions.
These arrangements (or variants) can be detected through genetic tests. Most of the time, medical practitioners order genetic tests directly from a certified lab. This is called clinical genetic testing.
DTC-GT makes it possible for consumers to directly learn about their DNA by placing orders for DNA kits online or in stores.
If you want to get a diagnosis for a set of symptoms or want to know if you carry mutations for a condition running in your family, you should skip the DTC-GT queue and go for clinical analysis.
But if you are just curious about what your genetic makeup holds for you and, in general, would like to be proactive about your health, then DTC-GT can surprise you with how much you can learn!
From exploring your ethnic roots to learning about your seasonal allergies genes, DTC-GT can offer information on all aspects of health and wellness.
However, you should take these with a grain of salt since there's a possibility that you will notice a few contradictions between what's in your reports and real-life experiences.
Here are the main categories of reports that many DTC-GT companies offer.
Here, it might also help to learn the difference between DNA testing and DNA analysis service.
Companies like 23andMe and AncestryDNA ship DNA kits for saliva collection.
Using the sample provided, they generate what is called DNA raw data, which is your genomic information in the form of letters and numbers given in a text file.
Additionally, depending on the package you choose, you may receive information about your ancestry and other basic health and wellness insights.
DNA analysis services allow you to get additional reports using your existing DNA test information.
For example, if you have your DNA raw data from 23andMe, companies like Xcode Life and DNAfit allow you to upload this file.
They then analyze the contents of the file and give you reports on additional categories like nutrition, fitness, sleep, skin, aging, drug reactions, etc.
DNA analysis services have gained popularity since they do not require repeating your DNA test, saving you a hundred bucks.
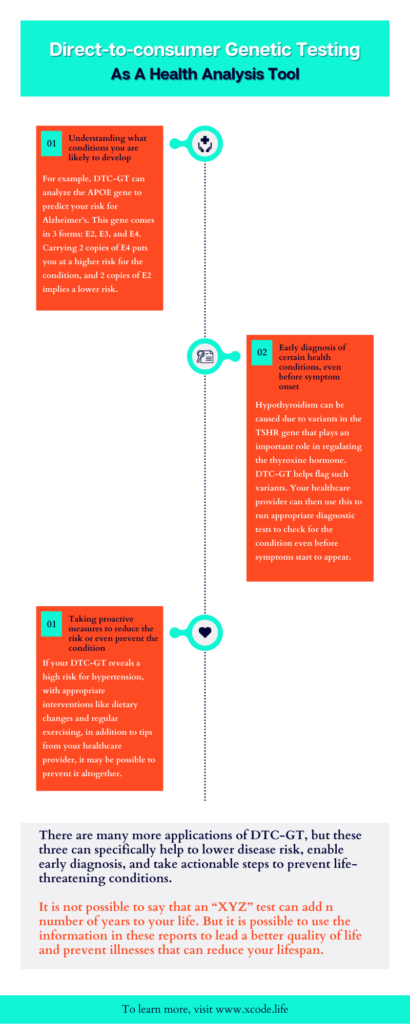
If you are looking for an answer to whether a genetic test can add ten years to your life, the short answer would be no.
And if you come across any company claiming so, you might want to read their fine print.
Having said this, it is possible to use your test results to lower your risk and even potentially avoid serious chronic conditions that may result in premature death.
For example, heart disease is the third most common cause of premature death globally.
Genetic testing helps identify markers that may put you at high risk for this condition. Therefore, you can take timely steps to lower your risk.
Overall, DTC-GT serves as a tool to understand your health profile and disease predispositions.
Disclaimer
Scientific validation of commercially available genetic tests is not standardized. Therefore, it is important to interpret your results with a qualified genetic counselor. Further, the recommendations in your report for specific conditions are to be followed only after consulting a qualified medical practitioner. The information in the reports does not include factors like family history, medical history, and other lifestyle factors.
We will discuss more on this in the upcoming sections.
What do genetic counselors (GCs) do? GCs are healthcare professionals who play multiple integral roles in genetic testing: A. assess an individual’s risk for a variety of inherited conditions, B. review genetic test results with individuals and families, C. support people in making decisions based on those results, and D. provide information to other healthcare providers in terms of treatment options and future courses of action.
While these roles are of high importance in clinical genetic testing, there’s a bit of controversy regarding the role of genetic counseling in DTC-GT.
We are not looking to take sides in this; rather, let’s have a look at the roles genetic counselors assume in the DTC-GT industry.
Genetic counselors help general consumers understand the basics of genetics and genetic testing and help them choose the right product for their needs through pre-test genetic counseling.
They also give product advice to other healthcare providers. Many doctors receive limited training in genetics in some parts of the world.
This explains genetic counselors’ involvement in product advice to doctors.
Many customers have reported wanting guidance on what to do with their DTC-GT results, especially with the disease predisposition part.
Genetic counselors fill this need by giving advice that promotes informed choices and adaptation to the disease risk.
They also further explain what their results mean.
For example, if the report indicates a high risk for colorectal cancer, the genetic counselor may explain what this means for their future. They also touch upon the screening, treatment, and management options available.
Further, they may recommend following some healthy choices like increasing physical activity, keeping a healthy weight, limiting alcohol consumption, and avoiding tobacco to lower colorectal cancer risk.
DTC-GT can reveal a lot of information that can often puzzle the users regarding what they should discuss with their doctors.
Genetic counselors can help by guiding the consumer on what to focus on with their doctors.
Outside these roles, genetic counselors are also involved in the architecture of DTC-GT products.
Overall, with the growth of the DTC-GT industry, we are seeing more and more genetic counselors assuming roles other than what are considered to be the “traditional” aspects of genetic counseling.
We have come a long way from Mendel and his peas, the first set of experiments that identified genes as units of inheritance.
However, we still have a long way to go in interpreting and understanding the world of information our genomes contain.
DTC-GT promotes awareness and interest in genetics and inherited conditions and helps consumers take a proactive approach to their health.
Further, services like ancestry reporting and ethnicity estimation bring the fun element to the DTC-GT field.
However, DTC-GT comes with its risks and limitations.
Let’s explore each of them in detail now.
Most of the DTC-GT services are not diagnostic in nature. They provide an overview of comprehensive genetic risk of health conditions.
They attempt to answer questions like “how likely are you to develop type 2 diabetes,” “how likely are you to carry autism-associated gene variants,” and “how likely are you to have the enzyme deficiency that causes lactose intolerance.”
However, there's no statistical model for risk interpretation, making it difficult for users to understand what it means to have "a high risk for type 2 diabetes."
This can create unnecessary anxiety for the consumer.
Genetic counselors can neutralize this by helping the consumer with risk interpretation and providing further courses of action.
Note: A high risk on your DTC-GT report does not mean that you will definitely go on to develop the condition. At the same time, low risk doesn’t guarantee that you will not develop the condition.
A highly prevalent concern among DTC-GT consumers is the possibility of their DNA data getting into the wrong hands.
What happens to the DNA data after its extracted from the sample? Or what happens when uploading it to a DNA analysis service?
Many DTC-GT companies promise data privacy and not sharing the information with any third parties without consent. While this provides a level of security for your data, there still have been reports of data breaches by some DTC-GT companies.
Some countries do have laws set in place that aims at protecting consumers' genetic information. One example would be the Genetic Information Non-Discrimination Act (GINA) of 2008 in the USA, which protects the user from discrimination based on the findings of a genetic test.
If you are concerned about data misuse/leak, read the company's privacy policy before opting for their services.
You can also reach out to the company directly via email or social media to address all your questions about privacy.
Ten years ago, it cost about $10,000 for whole genome sequencing. It subsequently fell to $1,000 a few years ago. And today, you can get it for $300-$600.
However, not many DTC-GT companies offer whole genome sequencing. Many employ genotyping analysis, which captures only 0.03% of the whole genome.
While this reports around 700,000 variants, if you have disease-causing variants outside this, they may not be reported.
Further, due to errors in DNA data generation, certain variants may not be called in, and as a result, you may not find the trait/condition of interest in your report.
This is why it is important to remember that your reports are not diagnostic.
DTC-GT services provide a lot of information. This may include information on a condition you were not necessarily keen on learning about.
For example, you might have taken a test to learn about your risk for anxiety, but your report may also indicate a high risk for schizophrenia.
This can cause unnecessary alarm and emotional unrest.
Unexpected findings are more common with ancestry genetic tests.
Many people have found and connected with their biological parents through services like 23andMe.
While some of them sign-up to connect with the biological family, for those who are not aware that they were adopted, the results can be quite shocking!
It is no secret that you share your DNA with your family members.
So if you carry a variant associated with a health risk, it increases the chances that your family members (especially the first and second-degree members) have it too.
For example, if your genetic test reveals variations in BRCA1 and BRCA2 genes associated with higher breast cancer risk, there’s an increased likelihood of other family members having these variants.
This can result in a moral dilemma on whether or not to disclose this information to the concerned people.
On the one hand, giving them this information can enable them to take measures for screening and early diagnosis. This can result in better treatment options and prognosis if they develop breast cancer.
On the other hand, the mere presence of these variants doesn’t guarantee that the condition will occur. So sharing the result can result in years of anxiety, and not to forget the cost implications of screenings and tests.
Finally, some people consciously choose not to be aware of such information. Sharing your DTC-GT results with them can violate their right “to not know.”
The choice of opting for a DTC-GT is a very personal one.
DTC-GT can cost anywhere from $100 to $2,000. And for many, this may not be just “some change in the pocket.”
So, deciding to take a DTC-GT cannot be made on a whim.
It is important to define the purpose of the test.
If you are planning a family and are concerned about a health condition running in your family, a medical doctor may point you to a diagnostic genetic test.
DTC-GT shouldn’t be considered an option in this case.
Or if you or your child are exhibiting unexplained symptoms, turning to DTC-GT for an answer may not be the wisest choice.
Your healthcare practitioner can get your medical and family history details to recommend appropriate testing.
Who’s it right for?
Whether or not you need a test also depends on your intent to get a test done and what you plan to do with the results.
DTC-GT can be a great tool for your health if your expectations going into the test are in the right direction and you know what to do with the results.
Here are some tips to get the most out of your genetic test results.
Overall, to make the most out of your test, it is important to take your DTC-GT results with a grain of salt and talk to the necessary healthcare providers for result interpretation and other advice.
According to a report, DTC-GT surpassed USD 3 billion in 2022 and is expected to grow at the rate of 11.5% CAGR from 2023-2032.
In the DTC-GT market, predictive testing held >19% share in 2022.
Several factors are attributed to boosting product development in the forthcoming years.
Technologies in genetic testing have come a long way since its advent enabling millions of users to avail DNA tests from the comfort of their homes. DTC genetic tests are an exciting way to discover more about yourself and your health. However, it's important to understand the limitations of these tests—and the potential for misinterpretation. Although DTC tests may provide a window into your genome, they are not a means to diagnose health conditions or predict the future. Ultimately, it is up to you and your healthcare provider to decide how best to use this information to improve your well-being.
Did you know hypertension is the number one risk factor for death globally? Prevalent in 1 billion people, this silent killer reportedly has genetic roots and can run in families.
In our bodies, blood flows through pipes called blood vessels, during which they exert a certain force on the inner walls of the vessels.
This force is called blood pressure.
Due to certain factors, blood can sometimes exert additional stress on the blood vessels and heart muscles, increasing the risk for stroke, kidney failure, and heart disease.
Genetics does play a role in high blood pressure.
In fact, studies have identified over 100 genetic changes associated with high blood pressure.
This means that carrying a certain set of genetic variants can increase your risk for this condition.
Family history also plays a role in influencing this risk.
If either or both of your parents (or other first-degree family members) have high blood pressure, you are more likely to develop the condition.
This risk further increases if the age of onset in your parents is before 55 years.
Other than genetics, certain lifestyle and environmental factors can influence the risk of high blood pressure.
Some of them are:
There are simple yet effective tips that can be followed to lower blood pressure.
High blood pressure is more common among African Americans than most other ethnicities.
Curious about your high blood pressure genes? Here’s how you can learn about it in 3 simple steps:
Do your cheeks turn red like an apple whenever you drink? You may be experiencing what is called an “alcohol flush reaction.” Due to specific genes, some people cannot process alcohol normally, leading to a red face.
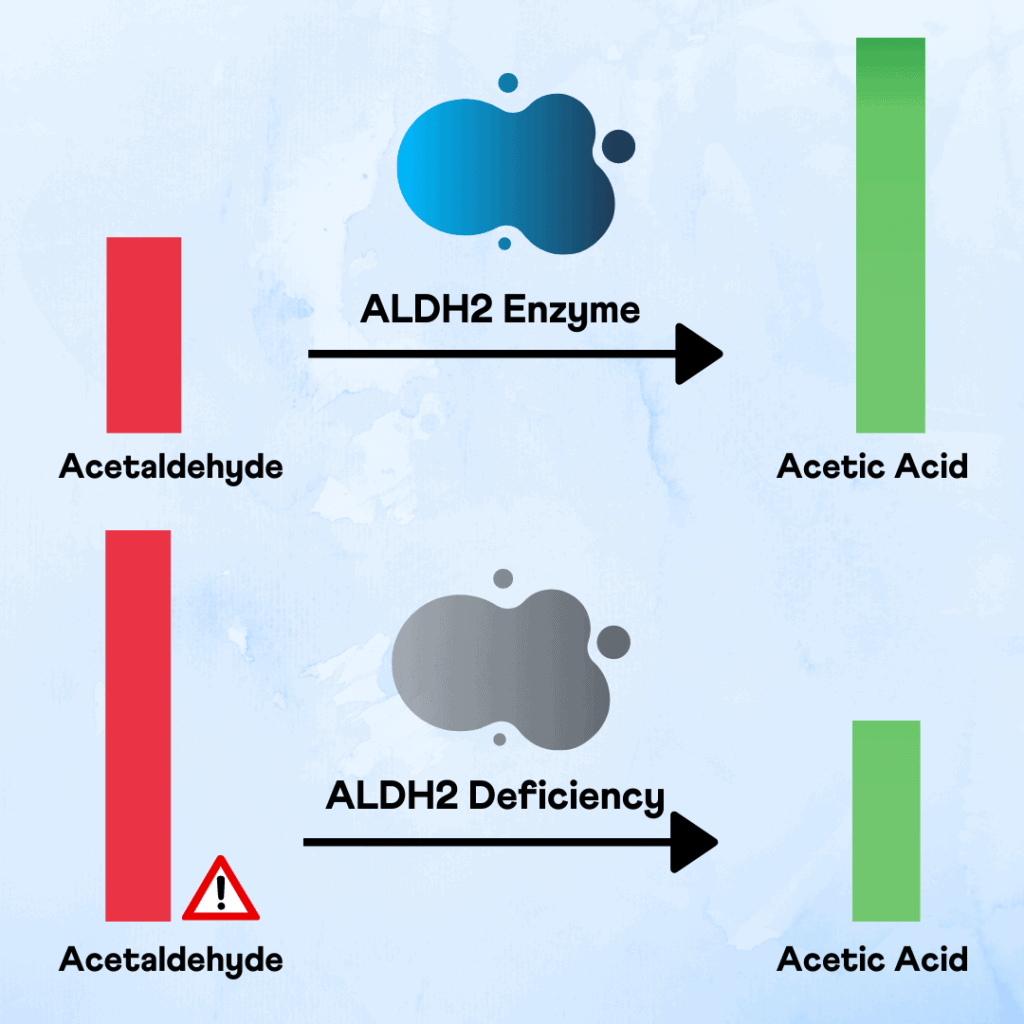
Whenever you drink, the alcohol is converted to a compound called acetaldehyde, which is toxic.
Acetaldehyde is also what causes the dreaded hangover symptoms.
Usually, acetaldehyde is broken down into a non-toxic compound called acetic acid, which is excreted through urine.
But some people have difficulty breaking down the acetaldehyde, which leads to the alcohol flush reaction.
The ALDH2 gene produces aldehyde dehydrogenase 2, the enzyme responsible for converting acetaldehyde to acetic acid.
Some people have a change in the ALDH2 gene, leading to a deficiency in this enzyme. This leads to a slower conversion of acetaldehyde to acetic acid.
This can lead to unpleasant side effects like hangovers, flushing, and heart palpitations.
The alcohol flush variant is the most common in the East-Asian population, with nearly 45% of people experiencing it.
Curious about your alcohol-flush genes? Here’s how you can learn about it in 3 simple steps:
With the COVID-19 pandemic a bit under control as we began 2022, the world still saw the Omicron wave looming.
The first half of the year was rough, with the COVID raging in waves across different parts of the world.
However, as the year progressed, biology and medicine saw some exciting innovations and advances in diverse fields- immunology, transplants, vaccines for malaria and respiratory syncytial virus to human evolution, and artificial intelligence.
Let’s look at ten of the biggest health and biology breakthroughs of 2022.

In January 2022, doctors at the University of Maryland Medical Centre replaced the heart of Mr. David Benett (57) with one from a pig.
The pig had gene editing done and was raised and bred to transplant its heart.
Though the process went well, Mr. Bennett passed away two months later.
Doctors suspect he got the cytomegalovirus infection from the pig.
This process of transplanting from an animal to a human is called xenotransplantation.
While this procedure has hope for people waiting for organ transplants, scientists still need to work on several aspects to make this process safe.
Though COVID wreaked havoc all through 2020-21, 2022 brought some development in COVID vaccines.
The world had access to some effective vaccines, including the two most effective mRNA vaccines.
However, the virus continued to evolve and bypass the vaccine defenses.
Fortunately, vaccine manufacturers had their eyes on this growing trend and developed newer shots for the Omicron variant and the original strain.
The bivalent (containing two strains of the virus) vaccines boosted protection against the virus.
With the COVID-19 vaccines, there has been an acceleration in innovation in immune research.
With a drastic increase in immunology knowledge, we can now innovate and create vaccines on a war footing.
Immunology is the branch of biology that studies the immune systems in humans and other organisms.
One example of this is the autumn COVID-19 boosters.
These bivalent vaccines target the original strain of the SARS-CoV-2 alongside the Omicron variant.
Bivalent vaccines are advantages over the original vaccine as they have broader coverage and offer better protection against the virus.
To further enhance immunity, the COVID-19 vaccines have been coupled with multiple strains of the flu virus to create a multivalent vaccine for COVID-19 and the flu.
Mucosal vaccines are sniffable or inhalable vaccines that have already been launched in countries like China.
These vaccines promise to offer long-term protection against respiratory infections.
Artificial Intelligence (AI) has been transforming the world before our eyes, including molecular biology.
In 2022, AI contributed to developing several drugs to help deal with resistance by microbes.
The overuse and misuse of antimicrobials have resulted in a phenomenon called antimicrobial resistance (AMR).
Yue Ma and colleagues from the Chinese Academy of Sciences used machine-learning techniques to identify antimicrobial peptides (smaller proteins) in the human gut.
AI was able to identify 181 of 216 peptides that showed antimicrobial activity.
More than half the peptides discovered by AI were found to be new, without any similarities to existing antimicrobials.
This increases the chances of overriding existing resistance mechanisms contributing to AMR. With this knowledge, it is possible to develop more effective medications against harmful microbes.
Type 1 diabetes or juvenile diabetes usually develops in adolescence.
In November 2022, the FDA approved a monoclonal antibody drug called teplizumab that could delay the onset of type 1 diabetes for several years.
This drug has been prescribed as a 14-day treatment, a 30-minute infusion for adults and children eight years and older with stage 2 type 1 diabetes.
Stage 2 type 1 diabetes is one step before a clinical diagnosis.
Research states that teplizumab delays the onset of stage 3 of type 1 diabetes for two years, compared with the placebo group.
The only current concern with this drug is its high cost.
Researchers at the Weizmann Institute of Science in Israel created a mouse embryo inside a bioreactor without sperm and egg cells.
This was possible as the embryos were created from stem cell cultures in a Petri dish.
The resultant embryos were normal and began elongating on day three, developing a heart by day eight.
This was the first time scientists could grow a synthetic mouse embryo outside the womb.
This experiment is significant as it gives scientists the power to create various organs for transplanting and understand how genetic changes develop.
The Nobel Prize in Physiology or Medicine in 2022 was awarded to Svante Paabo for his discovery showing genetic relationships among hominin ancestors.
He developed methods of reconstructing ancient DNA.
Paabo and his colleague sequenced the genome of the Neanderthals and discovered a new hominin species called the Denisovans.
This discovery revealed that early humans interbred with this now-extinct species.
These interbreeding trysts gave us traits like the ability to survive at higher altitudes and the vulnerability to infections like COVID-19.
Before the pandemic, most people did not bother or give a thought about the air they breathed when indoors.
However, today, people are more aware and concerned about their indoor air quality.
With greater awareness about how droplet infections and airborne particles can spread infections in indoor spaces, people are more willing to reduce the risk.
People understand the importance of improved indoor air quality, from ventilating buildings to using indoor air purifiers.
The ability of cells to sense and respond to their mechanical environment has been known for several decades.
Early signs of diseases like cancer and Alzheimer’s are often associated with changes in cell stiffness.
Since determining cell stiffness inside the body is difficult and invasive, this test is not performed inside animals or humans.
However, in 2022, two research groups, one from Germany and one from the USA, published separate studies demonstrating improvements in the measurement of cell stiffness using Brillouin microscopy.
Brillouin microscopy is a non-damaging, non-invasive technique that allows one to ‘see’ cell stiffness without touching them.
This tool can be widely applied to observe changes in the mechanical properties of cells in living organisms.
It increased the potential for early diagnosis of several diseases.
Scientists detected viruses like those that cause polio in sewage systems in the UK and New York.
They were also able to spot COVID cases and new types of SARS in these regions before they developed into surges or caused a rise in cases.
These secrets were unearthed from our poop!
Though it sounds gross, the human waste contains a large amount of information on infectious diseases that are very important to scientists.
With an exciting 2022 that went by, 2023 is beaming with more potential. Here’s what’s in store for 2023:
This may be the last year without adequate tools to fight this virus.
A new study showed that the drug tripeptide, approved for treating type 2 diabetes, effectively reduces obesity.
2.4 mg of semaglutide provides an average of up to 15% weight loss.
While the human lifespan has increased in the last few decades, the number of older adults living with coronary and circulatory conditions has increased too. According to the Centers for Disease Control and Prevention (CDC), 21.7% of all Americans over 65 have been diagnosed with Coronary Heart Disease (CHD), stroke, or both. Thus, the topic of heart health in the elderly has earned a spotlight in the research field.
CHD is the most common type of heart problem affecting older adults. According to CDC, about 20.1 million people worldwide have this condition.
In the United States, one person gets a heart attack every 40 seconds, making this a prevalent heart problem too.
Heart failure happens when the person’s heart cannot pump enough blood, which can turn fatal if not treated early on. About 6.2 million in the United States are diagnosed with heart failure yearly.
A stroke happens when the blood supply to the brain is cut off. One in every six cardiovascular deaths is due to stroke. Even if not fatal, stroke can lead to permanent disabilities and reduced mobility.
The following factors can interfere with your heart health and increase your risk for heart problems.
Recently, everyone has been talking about increasing the daily steps people take to stay healthy. There are many fitness monitors and applications to monitor this.
The person is more active when the step count/day is higher—being physically active benefits multiple ways, including reducing the risk of heart disease and other lifestyle disorders.
Recently, scientists from the Department of Kinesiology conducted a study at the School of Public Health and Health Sciences. Kinesiology is the study of body movements.
According to this study, older adults who walked at least 6000-9000 steps a day had a 40-50% lower chance of developing cardiovascular problems than people who only walked 2000 steps a day.
This study was a meta-analysis, combining eight prospective studies. 20,152 adults aged 18 and above were part of the analysis.
The mean age of the study participants was 63.2±12.4 years. Of these, 52% were women, and the rest were men.
The individuals’ daily step count was measured, and the follow-up happened after 6.2 years.
The study reported about 1523 cardiovascular disease incidents in these participants in this time.
This adds to about 12.4 incidents per 1000 participants.
The researchers considered the following cardiovascular incidents.
According to the results, older adults who took 6,000-9,000 steps every day had a 40-50% lowered risk of developing heart conditions compared to those who only took 2,000 steps per day.
This study found this relationship between steps and cardiovascular disease risk applicable only in older adults. In younger adults, other co-factors like weight and diet could also influence cardiovascular risk, apart from the step count.
The study recommends that older adults focus on increasing their step count, whatever the present number is. People walking 2K steps a day would benefit by increasing it to 3,000 to 4,000 steps.
Those already in the 6K range can still decrease their risk of developing heart conditions by increasing the step count slightly more every day.
According to the study, average step count could be an easy metric for doctors to analyze the potential risk for developing cardiovascular diseases in older adult patients.
It is wiser to get at least 2-3K steps done first thing in the morning, so it is easy to complete the goal by the end of the day.
If possible, you could wake up and take a brisk walk inside the community. If not, you could walk in your garden or patio.
Find a walking buddy in the neighborhood. If you have a friend to walk with, you may do it more regularly. Having company while walking makes the process stress-free and enjoyable.
Many older adults talk to their family or friends on the phone at least once a day. Try walking around the room while talking on the phone to increase the step count.
This can help increase the step count gradually throughout the day.
You can schedule an alarm to remind you to take a walk. This way, you will remember, and even if you are feeling sluggish, the alarm may encourage you to get up and step outside the house.
This is an effortless way to increase step count. Walk to the neighborhood stores to buy groceries or vegetables daily instead of ordering in or taking the car. Using the four-wheeler lesser would help increase step count over the day.
Older adults who cannot independently walk outside the house can try spot walking. Spot walking is imitating walking while standing in the same spot. This gives the same benefit as actual walking and is safer for adults at risk for falls.
Do you struggle to wake up early, no matter when you go to bed? Turns out it may not be due to laziness, but because of something called the chronotype. You may be genetically wired to wake up at a certain time. This is highly influenced by your genetic makeup.
The internal sleep-wake cycle, also known as the circadian rhythm, is the natural pattern of physiological processes that occur in the body over 24 hours.
These processes include the sleep-wake cycle, body temperature, hormone production, and metabolism.
The circadian rhythm is regulated by an internal "biological clock" located in the hypothalamus of the brain, which is influenced by external cues such as light and temperature.
Disruptions to the internal sleep-wake cycle, such as those caused by shift work or jet lag, can negatively affect health and well-being.
Genetics plays a significant role in determining an individual's natural wake-up time, also known as their chronotype.
Studies have identified several specific genes that influence the circadian rhythm, including those that regulate the production of melatonin and the sensitivity of the body's internal clock to light.
One of the key genes identified in this regard is the RGS16 gene, which regulates the period of the circadian rhythm.
Variations of this gene have been linked to differences in sleep timing.
Other genes, such as RASA4B, HCRTR2, CA14, EXD3, CLN5, NOL4, and PLCL1, also regulate the internal clock.
It's worth noting that while genetics play a big role in determining an individual's chronotype, environmental factors such as exposure to light, work schedule, and lifestyle habits can also have an impact.
Resetting your wake-up time can be done by making changes to your daily routine and environment. Here are a few tips that may help:
Keep in mind that adjusting to a new sleep schedule can take a few days to a couple of weeks, so be patient and consistent in making these changes.
Curious about your sleep genes? Here’s how you can learn about it in 3 simple steps: