Our body is made up of cells.
All cells comprise smaller components called cell organelles, each with a specific function that it performs within the cell.
One such organelle is the mitochondria, responsible for converting energy from food into a form the cell can use.
Since the mitochondria produce energy, it is also called the powerhouse of the cell.
Each cell contains hundreds of mitochondria floating in a fluid in the cell called the cytoplasm.
While most of the DNA in a cell is packed into a structure called the nucleus, a small amount of DNA is also found to occur in the mitochondria.
This genetic material is called mitochondrial DNA or mtDNA.
Almost all the cells in our body contain hundreds of copies of mitochondrial DNA, unlike 23 pairs of chromosomes in autosomal, Y- and X-DNA (the DNA you receive from your parents).
The mitochondrial DNA contains 37 genes, all of which are required for normal mitochondrial function.
13 of these genes give instructions for making enzymes involved in oxidative phosphorylation.
Oxidative phosphorylation is a process that uses oxygen and simple sugars to create ATP (the main source of energy for the cell).
The remaining genes in the mitochondrial DNA provide instructions for producing molecules responsible for protein synthesis and other functions.
We inherit our mitochondrial DNA from our mother. For this reason, we share our mtDNA with our mothers, sisters, brothers, maternal grandmothers, aunts, uncles, and other maternal relatives.
Since mitochondrial DNA undergoes a high frequency of abnormal changes (called mutations), the mtDNA sequences between closely related maternal relatives may differ.
Mitochondrial DNA is complex; therefore, it may be difficult to predict how mtDNA mutations pass from the mother to her child.
These are chronic (long-term) genetic disorders that occur when the mitochondria cannot produce enough energy for the cell to function.
These disorders are usually inherited from the mother.
Mitochondrial disorders can affect any part of the body. A few common mitochondrial disorders are:
Mitochondrial disorders are fairly common; around one in 5,000 people are diagnosed with a condition yearly.
Mitochondrial inheritance
Mutations in the mtDNA that cause mitochondrial disease are inherited exclusively from the mothers, and there is a 100% chance that every child in the family will inherit the condition.
This test helps people trace their matrilineal or mother’s line of ancestry through their mitochondria.
Since everyone has mitochondria and each individual inherits them from their mother, people of all genders can take an mtDNA Test.
Mitochondrial DNA testing uncovers an individual’s mtDNA haplogroup (the ancient group of people from whom their matrilineage descends. Apart from this, mtDNA testing also helps determine a common maternal ancestor or look for diseases inherited from this line.
Once a blood sample is collected for the mtDNA testing, it is transported safely and securely to the laboratory.
In many cases, the sample collection may happen in the lab.
Once the sample has been prepared and the circular mtDNA isolated, it is divided into three sections:
Several genetic laboratories and companies perform mtDNA testing.
You can look for the one closest to you.
Always check for the necessary accreditations and certifications of the laboratory before going through with the test.
Anyone can take an mtDNA test for the following reasons:
The cost for mitochondrial DNA testing varies at different laboratories based on their machines, technology, and experience.
The cost of the test can also vary depending upon whether you choose to use a self-test kit or a laboratory-based one.
While regular DNA gives plenty of information about our ancestry and lineage and helps establish paternity, mitochondrial DNA offers several benefits as well:
The primary challenge in mtDNA analysis is that mtDNA shows heteroplasmy or the possibility of mutations.
This gives rise to two different mtDNA sequences.
So, at the time of analysis, there should be at least two differences between the sample and reference material.
Autosomal DNA testing is a powerful tool that can be used to learn about your family history. This test looks at your DNA, the unique genetic code that makes up your identity. By looking at your DNA, experts can tell you what countries your ancestors came from and how they are related to you. Autosomal DNA testing can also be used to find out if you have any genetic diseases or conditions. Autosomal DNA tests are relatively new and are becoming more popular as they become more affordable. If you're considering getting an autosomal DNA test, here's what you need to know.
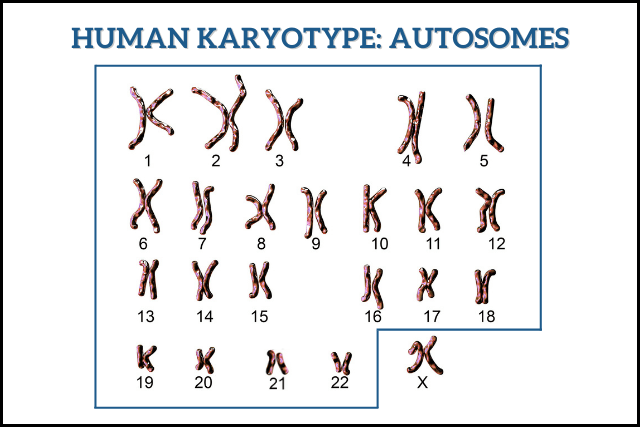
Almost all humans (with some exceptions) are born with 23 pairs of chromosomes.
The X and the Y chromosomes, also called the sex chromosomes are a part of the 23rd pair.
The other 22 pairs are called the autosomal chromosomes or the autosomes.
Autosomes are numbered roughly according to their sizes.
Chromosome 1 has approximately 2,800 genes, while chromosome 22 has approximately 750 genes.
Autosomal DNA is the DNA inherited from the autosomal chromosomes.
These genes in the autosomal DNA are 99.9 percent identical in every human being.
But small changes in these genes determine the rest of your genetic makeup, whether you inherit certain traits and your risk for several health conditions.
Genetic material is passed on from parents to children, and so are certain genetic conditions.
However, not all health conditions have the same inheritance pattern.
Autosomal dominant and autosomal recessive inheritances are two ways a genetic condition could pass on from one generation to the next.
Autosomal dominant inheritance
In autosomal dominant inheritance, one copy of the altered gene is sufficient for the trait/condition to express itself.
Only one parent needs to pass the altered gene.
Every child of this parent will have a 50% chance of inheriting the altered gene and thus the genetic condition.
Only changes that occur in the DNA of the sperm or egg can be passed on to children from their parents.
Autosomal recessive inheritance
Conditions inherited in an autosomal recessive pattern need two copies of the altered gene for expression.
To pass it on to their children, both parents must carry at least one copy of the altered gene.
They may not express the conditions themselves if they carry a single altered copy of the gene.
In other words, they are “carriers” of a particular genetic condition.
If two carriers of the same condition have children, each child has a 25% chance of being affected by the condition, a 50% chance of being a carrier of the condition, and a 25% chance of receiving 2 normal copies of the gene.
Autosomal DNA tests look at the autosomes, the 22 pairs of chromosomes that mostly everyone has.
Typically, experts use a DNA array to examine several thousand genetic regions or markers across all the 22 pairs.
Once this information is collected, they match it in their database with similar information from others.
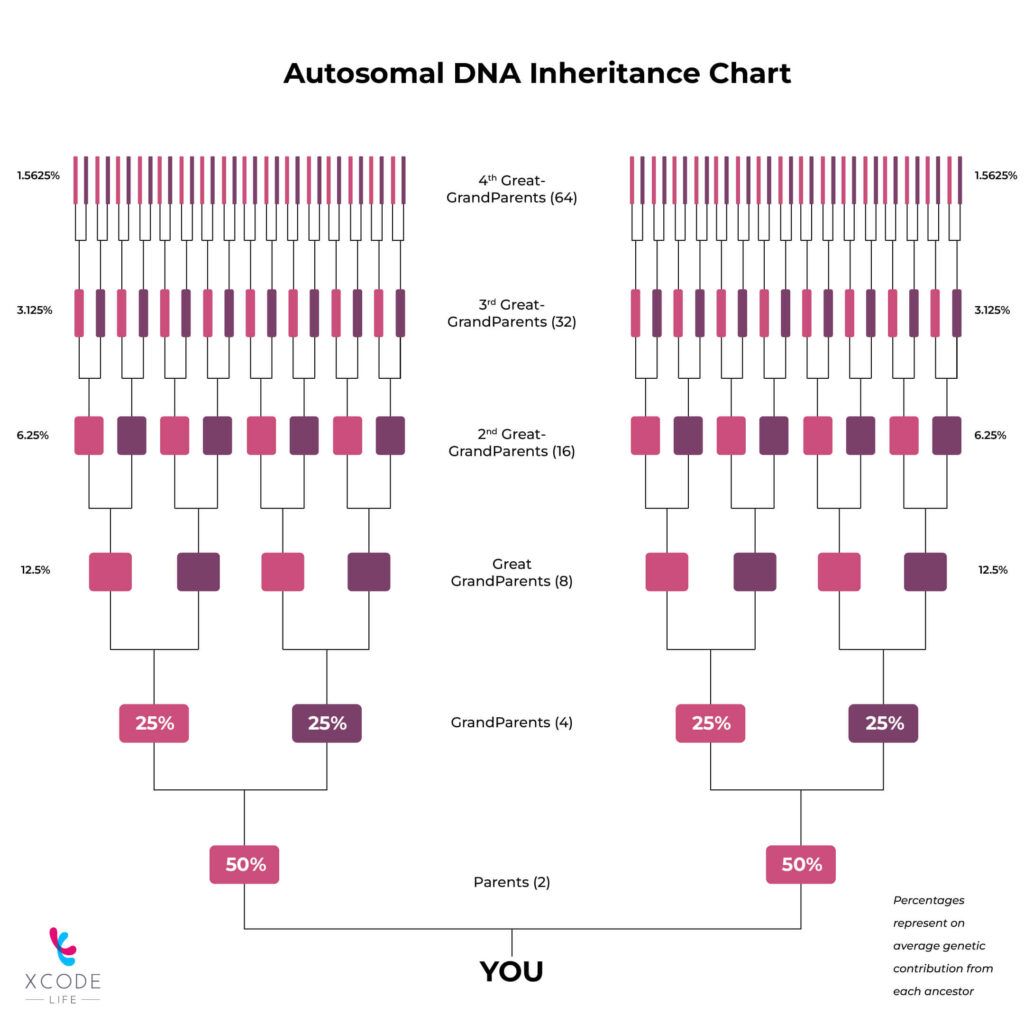
The larger the area of the genetic region you share with another person, the more closely you are related.
Autosomal DNA tests provide greater genetic information than Y-DNA and mitochondrial DNA (mtDNA) tests, which cannot reveal much information about close relatives or recent ancestry.
As mentioned above, scientists look at shared regions of DNA between you and several other people in the database to determine how closely you are related to someone.
The more shared markers you have with someone, the closer you are related to that person.
Scientists compare your DNA to DNA from people deep-rooted in several parts of the world to determine ethnicity.
If your DNA resembles that of people from Italy, that part of your DNA is said to have an Italian lineage.
This is how it is possible to learn where your ancestors lived centuries ago.
An autosomal DNA test is ideal for someone in the following scenarios:
Everyone can take an autosomal DNA test regardless of age and gender.
Autosomal DNA tests are popular options for identifying your close and distant relatives.
In fact, this test can reveal almost all your second and most of your third cousins.
It is pretty accurate to confirm parent/child relationships.
Distant relatives may be harder to find, but some tests can reveal even up to the eighth and tenth cousin!
Depending on the service provider you choose, the process may be slightly different.
However, there are some common steps in taking an autosomal DNA test.
Each service will use a different algorithm and have different reference genomes to define particular ethnicities and geographic regions.
So, the same person can get different ethnicity providers from different companies.
In fact, siblings can get dramatically different results from the same company.
In conclusion, autosomal DNA testing can be useful for those looking to learn more about their ancestry. It can also be used to help identify relatives, both close and distant. With the advent of online databases, such as 23andMe and AncestryDNA, DNA testing has become more accessible and affordable than ever. However, it is important to remember that the results of this type of test are not always accurate and should be interpreted with caution. If you are considering taking an autosomal DNA test, you should speak to a genetic counselor or other healthcare professional first.
It's no secret that some people are just better at napping than others. But have you ever wondered if there's a scientific reason for why some people can fall asleep anywhere, anytime? Turns out, there might be. A new study suggests that a excessive daytime sleepiness may be linked to your genes.
Researchers have identified a number of genes associated with excessive daytime sleepiness (EDS).
In the sample report below, we've attempted to analyze some important genes that increase the risk for EDS.
You can identify your genetic risk of EDS by using your 23andMe DNA data and placing an order for the Gene Sleep Report.
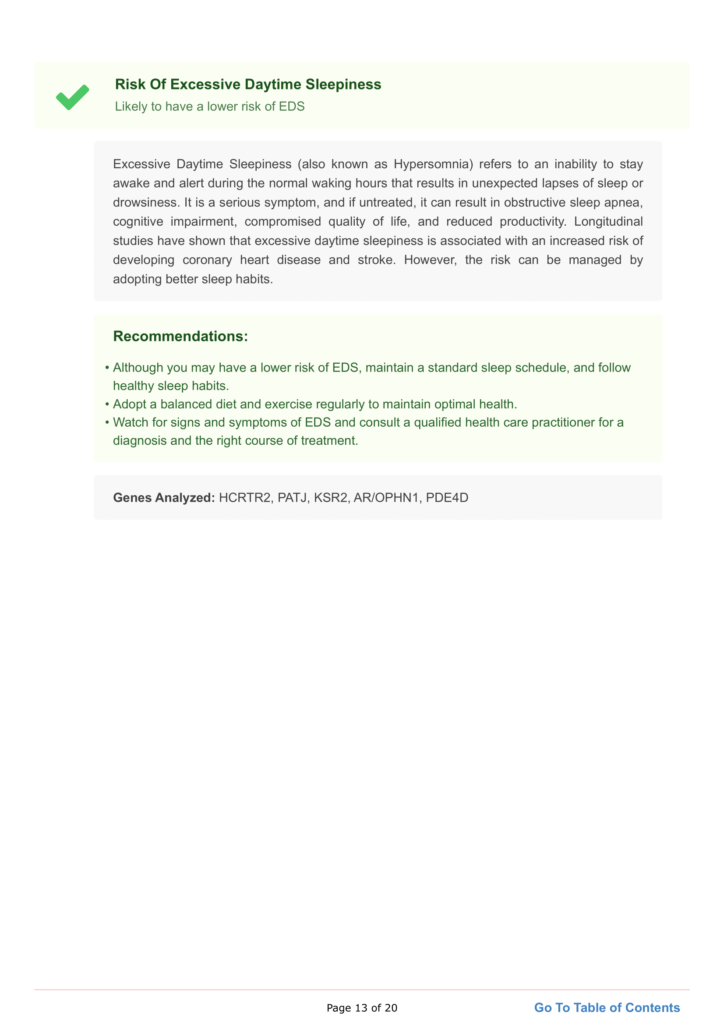
EDS (also known as hypersomnia) refers to the inability to stay awake and alert during normal waking hours, resulting in unexpected sleep or drowsiness lapses.
It can even occur after long stretches of sleep.
There are two types of hypersomnia; primary and secondary.
Some symptoms of hypersomnia include:
A 2019 study in Nature Communications documented that nearly 10–20% of people deal with excessive sleepiness to some degree.
Studies have shown that certain genetic variants influence daytime sleepiness, which explains why some individuals need more sleep than others.
Twin study results have estimated a 38% genetic variance in daytime sleepiness.
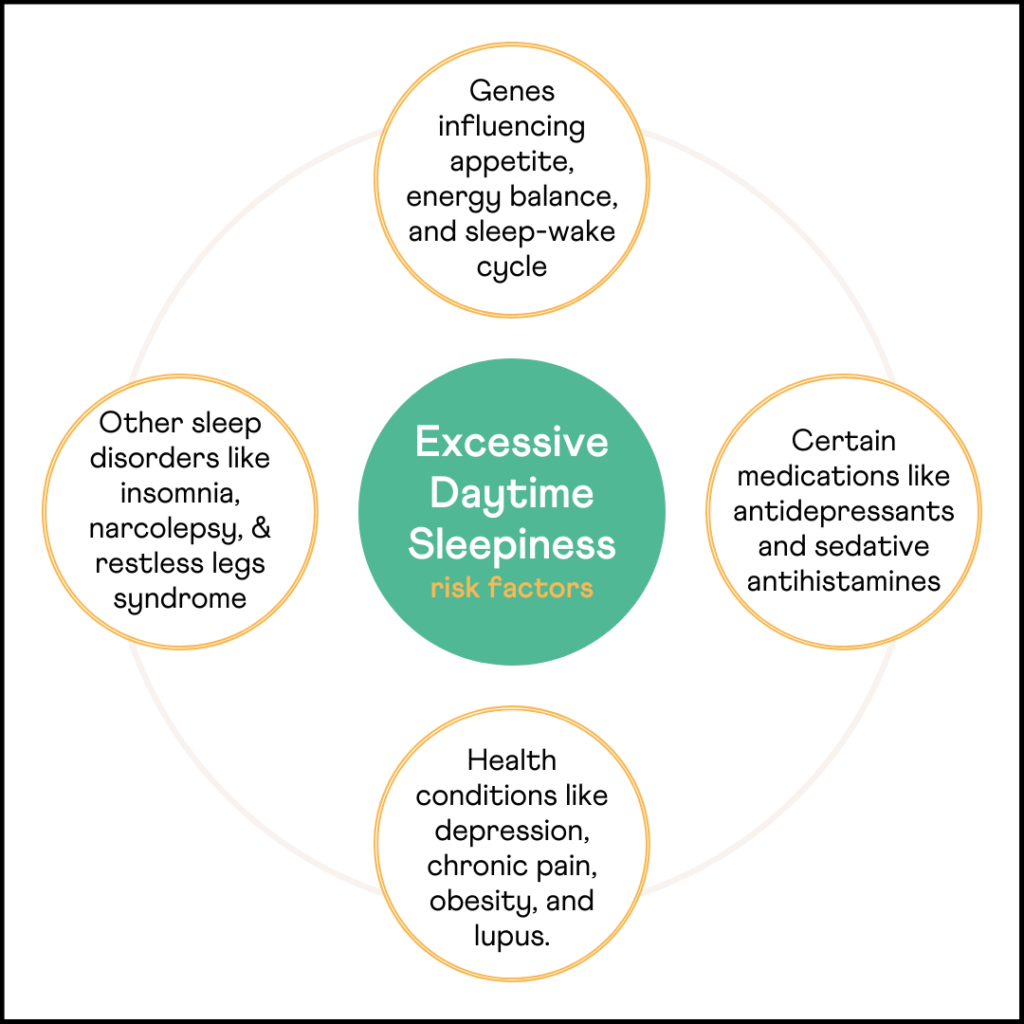
Studies have found an association between EDS and changes in certain genes like HCRTR2, PATJ, AR-OPHN1, KSR2, and PDE4D.
The HCRTR2 gene encodes a protein belonging to the G-protein coupled receptor, involved in regulating appetite, energy balance, neuroendocrine functions, and wake promotion.
Latest research studies suggest that variations in the HCRTR2 gene may influence the sleep-wake process.
The most common causes of excessive sleepiness include:
Research has also indicated that other health conditions can increase the risk of excessive sleepiness. Some of them include:
Studies have shown that EDS is associated with an increased risk of developing coronary heart disease and stroke.
However, the risk can be managed by improving the quality of sleep.
People with EDS also have poorer health than comparable adults.
According to a study, EDS is associated with negative effects on cognitive function.
In fact, EDS is a common symptom in neurological conditions like Parkinson’s and psychiatric conditions like depression.
Sleep disorders like insomnia, narcolepsy, and restless leg syndrome and other conditions like depression and obesity can cause EDS.
Identifying and treating these conditions can help shorten daytime naps.
Ensuring a dark and cool sleep environment, getting adequate physical activity during the daytime, reducing alcohol consumption and smoking, and adopting a calming bedtime routine can improve overall sleep hygiene and reduce the effects of sleep-related disorders.
Several medications are used to treat sleep disorders, but doctors most commonly prescribe this along with another treatment.
Commonly prescribed medications for EDS are modafinil, sodium oxybate, melatonin, and methylphenidate.
https://pubmed.ncbi.nlm.nih.gov/31409809/
https://pubmed.ncbi.nlm.nih.gov/27992416/
https://pubmed.ncbi.nlm.nih.gov/29783161/
Polycystic ovarian syndrome (PCOS) is a common condition that affects hormones in women in their childbearing years.
Most women with PCOS produce excessive amounts of androgens (male sex hormones), a condition called hyperandrogenism.
In this condition, one or both ovaries produce multiple small, immature ovarian follicles that appear like cysts on medical imaging.
This happens because abnormal hormone levels prevent follicles from growing and maturing to release egg cells.
PCOS is one of the leading causes of female infertility and increases your risk for other conditions like diabetes and hypertension.
By 40 years, around 10% of overweight women with PCOS develop high blood sugar levels, and around 35% develop prediabetes (high blood sugar levels but not high enough to be called diabetes).
Though many women with PCOS do not show any signs or symptoms, a few common symptoms of this condition include:
Around 70% of women with PCOS show abnormal hair growth.
Image: Is PCOS Genetic? Symptoms of PCOS
PCOS is common and affects around 6 to 10% of women worldwide.
The exact cause of PCOS is unknown. However, sufficient research shows that the condition runs in families.
Evidence shows that genetics plays a role in the development of PCOS.
Few other causes that may contribute to the development of PCOS are:
High androgens released by the ovaries result in irregular menstrual cycles, excess hair growth, and acne. The excess androgen also contributes to immature ovarian follicles that form cysts.
Women with PCOS tend to have a higher amount of insulin in their blood.
Increased insulin causes the ovaries to produce greater amounts of androgens and increase insulin resistance.
Being overweight or obese increases the amount of insulin produced by the body, further increasing insulin resistance and resulting in diabetes.
Women with PCOS have chronic low-grade inflammation that can further aggravate the condition.
Since women who develop PCOS have a family member with the same condition, it is said that PCOS may have a genetic component.
In fact, around 20% to 40% of women with PCOS have an affected family member.
Currently, it is believed that PCOS occurs due to an interplay between genetic and environmental factors.
PCOS is a polygenic (caused by multiple genes) and multifactorial condition.
Several genes are said to be associated with PCOS, such as
A few other genes that may contribute to the development of PCOS include:
Factors that increase a woman’s likelihood of developing PCOS can be lifestyle or genetics-related. Common risk factors for PCOS include:
If you know your risk for PCOS, here are some effective ways to prevent it:
While there is no cure for PCOS, appropriate and timely measures can help manage symptoms.
Image: Is PCOS Genetic? PCOS management at home
Polycystic ovarian syndrome (PCOS) is the most prevalent hormonal disorder affecting females. It is a common cause of menstrual irregularities and infertility during reproductive age. It causes symptoms affecting various body parts, from the skin to the hair. Emerging research suggests an association between PCOS and autoimmune disorders; This raises an important question: Is PCOS an Autoimmune Disease?
PCOS is a common hormonal disorder that can affect women of reproductive age.
The condition is caused by an imbalance of hormones, which can lead to irregular periods, excess hair growth, and difficulty getting pregnant.
The ovaries produce excessive male hormones (testosterone), which can cause the ovaries to become enlarged and develop cysts.
Although there is no cure for PCOS, treatment can help manage the symptoms.
Sometimes the immune system makes a mistake and attacks the body's tissues or organs. This is called autoimmunity.
Although the exact reason for autoimmunity is unknown, various mechanisms have been suggested for its development.
Sequestered antigens are some proteins in the body that are hidden from cells of the immune system, and thus the immune system never encounters them.
When these proteins are released due to accidental trauma or injury, they can initiate an immune response that may trigger autoimmune diseases.
Molecular mimicry is one of the leading mechanisms by which infectious or chemical agents may induce autoimmunity.
Here, autoimmunity occurs due to the close similarity between environmental substances and certain components in the body.
When the immune system generates a response against these foreign substances, it cross-reacts with the body's tissue.
In some cases, drugs can bind to normal proteins and change their properties, making them targets for immune attacks.
Tregs or regulatory T cells are important in suppressing unnecessary immune reactions and maintaining homeostasis.
Failure or decrease of Tregs can cause autoimmune disease.
Although research doesn’t conclusively state that PCOS is an autoimmune disorder, studies point out many similarities between both.
Autoantibodies
Both in PCOS and autoimmune diseases, autoantibodies can be detected.
In fact, autoantibodies are the hallmark of the latter.
Some common autoantibodies seen in both conditions are antinuclear antibodies, anti-thyroid antibodies, and anti-islet antibodies.
Insulin resistance
Insulin resistance is a significant risk factor for PCOS and is seen in several autoimmune disorders, such as rheumatoid arthritis and systemic lupus erythematosus (SLE).
The hormone insulin regulates blood sugar levels by storing excess sugar as fat.
With insulin resistance, the cells stop responding to the hormone insulin; as a result, more and more insulin is secreted.
In PCOS, excess insulin causes hormonal fluctuations and disrupts ovulation.
In autoimmune diseases, increased inflammation may drive insulin resistance.
There’s not too much clarity on what causes insulin resistance in PCOS, but an underlying autoimmune reaction could be the cause in some people.
Systemic Inflammation
Inflammation is the first line of defense against infection and is crucial for injury healing.
Scientific evidence suggests that irregular inflammatory responses can underlie autoimmune diseases like inflammatory bowel disease and rheumatoid arthritis.
Studies have shown that women with PCOS are more likely to have low-grade systemic inflammation.
Women with PCOS tend to have low levels of progesterone.
Progesterone is a hormone that occurs naturally in the body. It's involved in pregnancy and is produced mainly in the ovaries.
Progesterone is stimulated after ovulation.
Many people with PCOS have ovulation issues and therefore have lower progesterone levels.
With lower progesterone levels, estrogen is “unopposed,” leading to its excess levels in the body.
Increased estrogen production can trigger the secretion of autoantibodies.
Further, excess estrogen has also been tied to increased production of several proteins associated with inflammation like IL-4, IL-1, IL-6, and interferon-γ.
These effects are seen even after menopause.
Even with all these similarities, there’s no conclusive evidence to prove that PCOS is an autoimmune disorder.
Therefore, it still comes under the classification of endocrine (or hormonal) disorder.
Having said that, whether you have PCOS or autoimmune disorder, working on your immune system, lowering inflammation, and building up insulin sensitivity work well to manage the symptoms.
The presence of varying levels of autoantibodies in people with PCOS blows open a new avenue of research at a molecular level.
Since autoantibodies seem to affect long-term clinical management of PCOS, this new chapter of research can help discover better treatment options for those with PCOS.
Additional studies need to be performed at a genetic level to understand the contribution of autoimmunity to PCOS.
Tourette syndrome or disorder is a complex neurological condition characterized by sudden, repetitive, involuntary movements and noises called tics.
Tics usually show up in childhood, and their severity varies with time.
In most people with Tourette syndrome, the tics become milder and less frequent as they grow older.
People with Tourette syndrome show motor tics (uncontrolled body movements) and vocal tics (outbursts of sound).
One to ten in 1000 children may develop Tourette syndrome, but its exact incidence is unknown.
Tourette syndrome is also more common in people assigned male at birth (MAB) than those assigned female at birth (FAB).
The symptoms of Tourette syndrome begin between ages 5 and 10.
In children, the initial symptoms are usually mild, simple tics of the face, head, or arms.
Over time, the child may develop different tics that may happen more often and involve other body parts, like the trunk and legs.
Though symptoms vary in each child, a few involuntary, purposeless motor movements observed in Tourette syndrome include:
Vocal tics usually appear much later than motor tics and include:
Some people show complex tic behaviors that may look purposeful, such as:
Image: Is Tourette Syndrome Genetic? Symptoms of Tourette’s
Though the exact cause of Tourette syndrome is unknown, genetics and environmental factors are said to play a role in its occurrence.
The cause of Tourette syndrome is poorly understood.
Although environmental factors may play a role, genetic factors are thought to be the primary drivers of the pathogenesis of this disorder.
The fact that Tourettes has been seen running in families further substantiates the underlying genetic role.
Laboratory research has uncovered several loci (genetic regions) and genetic mutations associated with Tourette syndrome.
The several genetic changes identified may play an important role in explaining the variable symptoms observed in people with Tourette’s.
So far, no gene has been identified that is directly said to cause Tourette syndrome.
However, mutations in the SLITRK1 gene have been identified in a small group of people with Tourette syndrome.
The SLITRK1 gene gives instructions for producing a protein that probably plays a role in nerve cell development.
However, how the SLITRK1 gene causes Tourette syndrome is unknown.
Though the condition has a strong genetic link, the inheritance pattern of Tourette syndrome is unclear.
Tourette syndrome was previously thought to have an autosomal dominant pattern of inheritance (one affected or mutated gene copy in each cell is sufficient to cause the condition).
However, several decades of research have shown this is not the case.
Studies have shown that almost all Tourette syndrome cases result from genetic and environmental factors and not a single gene.
The risk factors for Tourette syndrome are unknown, but genes play a significant role.
Few suspected risk factors that may cause Tourette syndrome are:
Image: Is Tourette Syndrome Genetic? Children with Tourette’s
Tourette syndrome is usually diagnosed by a pediatrician or a qualified mental health professional who can identify the symptoms in children and adolescents.
The professional performs a comprehensive evaluation of the child or adolescent to diagnose Tourette syndrome, including
Most children are around seven years old when diagnosed with this disorder.
The treatment for Tourette syndrome in children depends upon several factors, including the severity of the condition.
While many children may not require treatment, some may require special classes, psychotherapy, and medications.
Comprehensive behavioral intervention for tics can help children manage and reduce tics.
Children with ADHD, OCD, or mood disorders may require medications.