Sleep is vital for one's health and well-being. Lack of sleep affects growth and stress hormones, our immune system, appetite, blood pressure, and cardiovascular health.
According to studies, not getting enough sleep increases your risk of disease, heart disease, and obesity.
This higher risk of chronic illnesses accompanies one another, leading to multimorbidity.
A new study by the University College London reports that getting <5 hours of sleep in mid-to-late life could be linked to an increased risk of developing at least two chronic diseases.
The ideal quantity of sleep varies by age and depends on the individual.
According to the National Sleep Foundation, these ranges are ideal:
Poor sleep hygiene can impact the quality of sleep.
Here are some factors that have a profound impact on your sleep duration.
The bedroom should be calm, dark, and light-free. A few hours before bed, blue light from devices such as TVs, computers, and phones should be avoided as it increases alertness.
Disorders like insomnia can make it difficult to fall or stay asleep and can result in poor-quality sleep.
The nighttime symptoms of narcolepsy include frightening dreams and frequent awakenings, which can impair sleep quality.
The exact mechanisms that control your sleep-wake cycle and whether you feel alert and awake or drowsy and relaxed are linked to the genes that may cause insomnia.
Serotonin, adenosine, GABA, hypocretin/orexin, and other neurotransmitters that are involved in your circadian rhythm may be impacted by these genes.
Researchers calculate that heredity contributes between 31% and 58% to your likelihood of having a shorter sleep duration.
There are 80 distinct genes with 126 variants associated with sleep duration.
Studies have found that alterations in the ADRB1 gene (Adrenoceptor Beta 1) are unique to naturally short sleepers.
This unique mutation that is inherited within the family seems to have reduced the sleep cycle of whoever received a copy of this mutant gene.
This gene implies further complications like resting heart rate, variation in and short sleep, and familial natural short sleep (FNSS).
Other characteristics of sleep, such as how much sleep you require, your chronotype, or whether you are an early bird or a night owl, are also influenced by your genes.
Researchers at the University of London analyzed the impact of sleep duration on the health of more than 7000 men and women at the ages of 50, 60, and 70.
The study was done over a period of 25 years and recorded how long each participant slept, their mortality, and whether or not they were diagnosed with 2 or more chronic conditions.
Chronic conditions include obesity, heart disease, cancer, diabetes, etc.
People who reported five hours or less of sleep per night at age 50 had:
In addition, it was discovered that a sleep duration of five hours or less at age 50 was linked to a 25% increased risk of mortality over a 25-year period of follow-up.
This association can largely be explained by the fact that short sleep duration increases the risk of chronic disease(s), increasing the risk of death.
Researchers examined if getting a long night's sleep—nine hours or more—had an impact on health outcomes as part of the study.
Long sleep durations at age 50 were not significantly associated with multimorbidity in healthy individuals.
Dyslexia is a neurological disorder that affects reading skills.
It is characterized by difficulty with phonemic awareness, phonology, and word decoding.
People with dyslexia may have trouble with some of the following:
Dyslexia occurs in individuals who have normal intelligence and normal vision.
It is the most common learning disability, affecting approximately 5-12% of the population.
The Gene Health Report gives an overview of your genetic risk for a range of health conditions, ranging from diabetes to heart disease.
Some of the neurological conditions included in the report are autism, epilepsy, Alzheimer’s, Parkinson’s, and multiple sclerosis (list not exhaustive).
Dyslexia in preschool and elementary school kids can manifest as trouble with
In older kids, teenagers, and adults, some common signs include:
Most people thinking of genetics imagine one gene being passed on from the biological parent to the child causing a condition.
While it is true for single-gene disorders, dyslexia doesn’t fall into the bracket.
With dyslexia, differences in multiple genes contribute to the condition.
These genes play a role in forming connections across the brain.
In dyslexia, the connection process is organized differently, contributing to difficulty in reading.
Studies have found 9 chromosomal regions (dyslexia susceptibility 1(DYX1)–dyslexia susceptibility 9 (DYX9)), which the researchers suspect contain the susceptibility genes.
From these regions, two genes, DCDC2 and KIAA03109, seem to have the strongest association with dyslexia.
The DCDC2 gene plays a crucial role in brain development
Changes in this gene have been associated with reading disability (RD), also referred to as developmental dyslexia.
Children with reading and writing difficulties are often found to harbor DCDC2 gene changes.
However, a more recent study challenged this association and reported that “DCDC2 deletion is not a strong risk factor for dyslexia.”
The KIAA0319 gene help with the formation of a part of the brain called the cerebral neocortex.
Changes in this gene are associated with developmental dyslexia.
Studies suggest that KIAA0319 is the most likely susceptibility gene for dyslexia from the DYX-1 to DYX-9 cluster.
Changes in this gene also play a role in specific language impairment.
There’s no clear inheritance pattern for dyslexia.
Reports suggest that about 40% of siblings of children with dyslexia tend to have reading issues.
49% of children born to biological parents with dyslexia also have dyslexia.
The risk increases when there are more affected family members.
There is an estimated 3–10‐fold increase in the relative risk for a sibling.
Both biological mothers and fathers can pass dyslexia on to their children if they have it.
There is roughly a 50%–60% chance of a child developing dyslexia if one of their biological parents has it.
There's no single gene that causes dyslexia.
However, biological parents with dyslexia have up to a 50-60% chance of having a child with the condition.
Studies have identified a gene called KIAA0319 that shows one of the most significant associations with dyslexia.
Emphysema is a type of Chronic Obstructive Pulmonary Disease (COPD).
About 16 million Americans have COPD. Millions of others show the symptoms but are still undiagnosed or untreated.
It is a condition that causes breathing difficulties due to air sac (alveoli) damage in the lungs.
The alveoli are like tiny balloons. They expand when they are filled with air and deflate when it flows out.
Due to certain conditions, the alveoli walls may become weak and saggy and cannot fully inflate and deflate.
As a result, the lungs cannot receive the needed oxygen or send out carbon dioxide.
Emphysema may go unnoticed in the early stages. Breathlessness sets in gradually, and people tend to ignore the symptoms until they worsen.
Emphysema often leads to lung failure and can be life-threatening. Therefore, it is important to get medical help early on.
Researchers have identified several genes associated with COPD.
In the sample report below, we've attempted to analyze some important genes that increase the risk of COPD.
You can identify your genetic risk of COPD by using your 23andMe DNA data and placing an order for the Gene Health Report.
The first symptom of emphysema that people notice is breathlessness or breathing difficulties.
Initially, the person may get breathless while performing physical activities like walking or climbing stairs.
Over time, the person may face breathing difficulties even while resting.
Other symptoms of emphysema are:
Smoking
Smoking remains the most common cause of developing emphysema.
Studies mention that about 10-15% of smokers develop the condition. The risk increases with the intensity of smoking.
Genetics may also play a role in causing the condition. We will discuss more on this in the coming sections.
Besides, environmental pollution could also lead to alveoli damage and emphysema.
Some of the common risk factors of emphysema are:
Intensity Of Smoking
According to studies, people may develop emphysema after 20-pack years of smoking. This means smoking one pack/day for 20 years or two packs/day for ten years.
Age
The average age of onset of symptoms is around 40, and the risk increases with age.
However, in people smoking marijuana, a type of drug, emphysema occurs at a young age.
Exposure To Irritants
Chronic exposure to second-hand smoke, workplace chemical fumes, and air pollution can all increase the risk of developing emphysema.
Emphysema could also be inherited and be a result of abnormal gene changes.
Alpha-1 Antitrypsin deficiency is a condition that leads to inherited emphysema.
Alpha-1 Antitrypsin (AAT) is a protein produced by the liver. Apart from various other functions, AAT protects the lungs from inflammation caused by exposure to external irritants.
When there is an AAT deficiency, there is a higher risk of developing emphysema and lung damage.
About one in 50 cases of emphysema could be inherited and caused by AAT deficiency.
SERPINA1 is a gene that controls the production of AAT in the body.
There are several mutations (abnormal changes) observed in this gene, and some of them could bring down AAT levels.
M is a normal allele of the gene, while Z is the risk allele that leads to low AAT production.
Studies suggest that there could be about 100,000 people living in the United States with the ZZ genotype, and they have a very high risk of developing severe emphysema.
Emphysema can lead to the below health complications.
Frequent Cold and Flu - People with emphysema develop cold and flu infections frequently, and the severity of the infection is high too.
Chronic Bronchitis - People with severe emphysema may develop chronic bronchitis, another type of COPD.
Both conditions, together, can lead to lung damage and subsequent failure.
Pneumonia - Due to alveoli damage, the person can develop pneumonia, a form of lung infection.
Lung Damage - If multiple alveoli get damaged, the lung’s capacity to function may be affected, leading to lung damage.
Lung Cancer - Emphysema is a risk factor for developing lung cancer.
Emphysema can be diagnosed with chest X-rays, CT scans, lung function tests, and other blood tests.
Emphysema cannot be cured. However, once diagnosed, it can be handled and kept controlled using the below solutions and treatment options.
Lifestyle Changes
Medicines and rehabilitation options
Surgery
About one in 50 cases of emphysema could be inherited and caused by lower production of the AAT protein.
Some people with just one risk allele could be carriers of the condition and pass them on to the next generation without getting affected.
Environmental factors and lifestyle habits may act as triggers for developing the condition early or can worsen the prognosis.
Genetic testing may provide valuable information on whether or not a person is at risk for developing the condition.
Autoimmune disorders are conditions in which the body’s immune system attacks healthy cells.
The immune system is designed to protect the body from infection and disease.
However, in people with autoimmune disorders, the immune system mistakes healthy cells for foreign invaders and attacks them.
This can cause a wide range of symptoms.
Autoimmune disorders can affect any part of the body and are often chronic, meaning they last for a long time.
Gilbert's syndrome is a genetic disorder that affects the liver's ability to process bilirubin.
Bilirubin is a yellow pigment produced when red blood cells are broken down.
Gilbert's syndrome is usually harmless and doesn't require treatment.
People with Gilbert's Syndrome may have yellowing of their skin or eyes, but this is usually not noticeable.
The symptoms of Gilbert's Syndrome are often mistaken for other conditions, such as jaundice.
So far, there’s no solid evidence to confirm that Gilbert’s syndrome is an autoimmune disease.
It occurs due to mutations in the gene called UGT1A1.
In the upcoming section, we'll discuss this gene and its association with Gilbert's.
Gilbert’s can be mistaken for an autoimmune condition that also manifests as high bilirubin levels - autoimmune hepatitis.
Autoimmune hepatitis occurs when the body's immune system incorrectly targets and attacks the liver.
This can lead to chronic inflammation and serious damage to the liver cells.
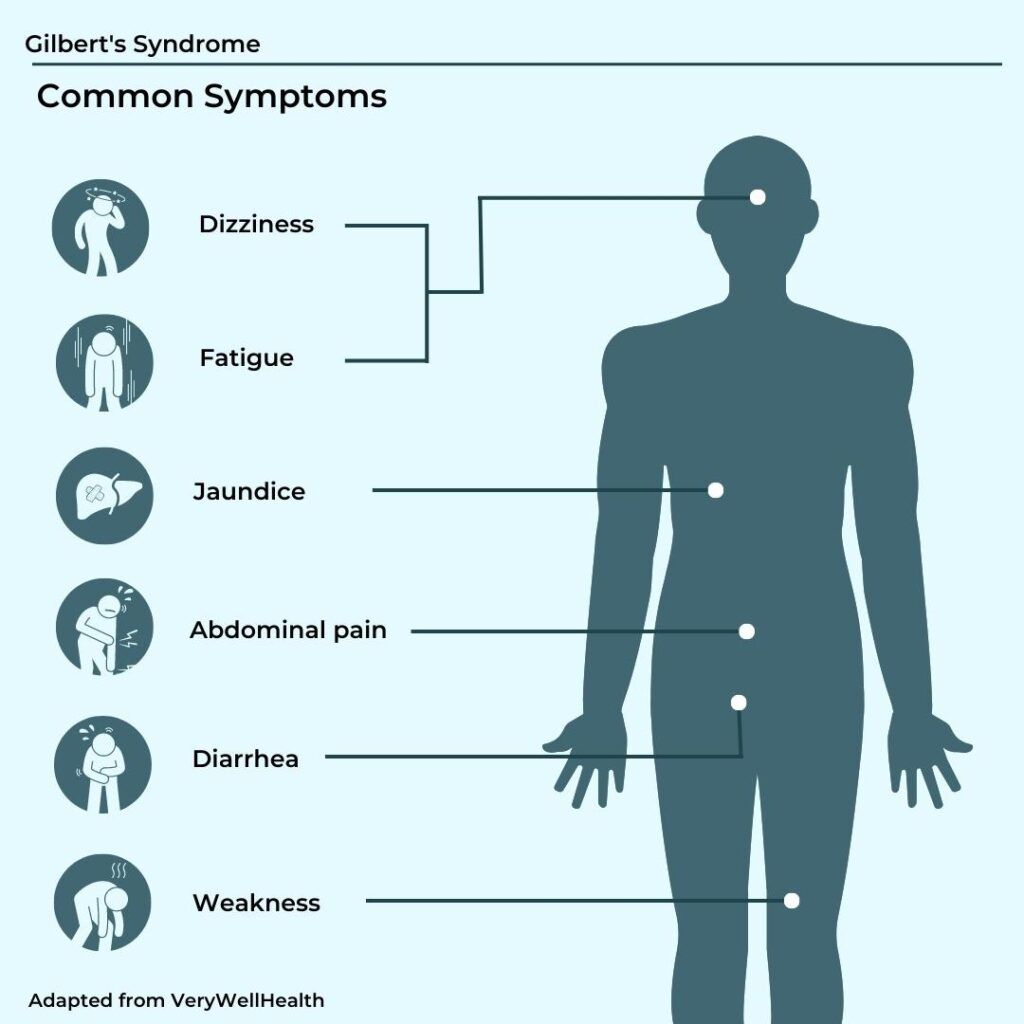
Most people with Gilbert’s syndrome don't have symptoms.
This is because the symptoms are apparent only when bilirubin levels rise beyond a limit.
Most people with Gilbert’s have enough liver enzymes to break down bilirubin.
For those who don’t, bilirubin levels rise in the blood and can cause the following symptoms:
Certain factors trigger the rise of bilirubin levels. They include
Gilbert’s syndrome occurs due to mutations in the UGT1A1 gene.
This gene is located on the long arm (q) of chromosome 2 (2q37).
The UGT1A1 gene contains instructions for producing a liver enzyme known as uridine diphosphate-glucuronosyltransferase-1A1 (UGT1A1).
This enzyme carries out the excretion of bilirubin from the body.
Mutations or changes in this gene can result in reduced levels of the UGT1A1.
People with Gilbert's have only one-third of the normal enzyme activity as others.
Gilbert’s syndrome is inherited in an autosomal recessive manner.
What does this mean?
Humans have 2 copies of every gene - one from each of the biological parents.
If an individual receives one normal gene and one gene with mutations for Gilbert’s, the person will be a carrier for the condition but usually will not show symptoms.
The risk for two carrier biological parents to both pass the mutated gene and, therefore, have an affected child is 25% with each pregnancy.
The chances of 1 parent passing the mutated gene and having a child who is a carrier is 50% with each pregnancy.
The risk is the same for males and females.
People with Gilbert’s syndrome may not get diagnosed in the early stages.
Mostly, diagnoses happen when they are in their 20s or 30s.
Some diagnostic tests for Gilbert’s include:
Most people with Gilbert’s do not need any treatment.
Some tips to prevent bilirubin level rise are:
It is important to note that the UGT1A1 enzyme that breaks down bilirubin also breaks down certain drugs like acetaminophen, cancer and hepatitis drugs, and monoclonal antibodies.
If you have Gilbert’s, it is advisable to consult your doctor before taking medicines.
https://www.webmd.com/children/what-is-gilbert-syndrome
https://medlineplus.gov/genetics/gene/ugt1a1/
https://www.mayoclinic.org/diseases-conditions/autoimmune-hepatitis/symptoms-causes/syc-20352153
https://www.spandidos-publications.com/10.3892/etm.2020.9219
Flu season is just around the corner, and health officials are urging everyone to get their flu shot. According to the Centers for Disease Control and Prevention (CDC), people with diabetes are at high risk of developing serious flu-related complications, such as pneumonia. The CDC recommends that everyone 6 months of age and older get a yearly flu vaccine, but it’s especially important for people with diabetes to get vaccinated.
Your body needs extra energy to fight any infection.
Thus, the body manufactures additional glucose for its fuelling needs.
Further, the infection may stimulate the release of stress hormones like adrenaline and cortisol, both of which can reduce the effectiveness of insulin.
Insulin is responsible for regulating (or lowering) blood sugar levels in the body.
Additional glucose production combined with the lower effectiveness of insulin can make it difficult for the glucose levels to lower back to normal.
This is more profoundly seen in people with diabetes (PWD).
When the glucose levels become too high, the body gets dehydrated, trying to compensate for the levels.
This condition is called hyperosmolar hyperglycemic nonketotic syndrome (HHNS) and can be life-threatening.
The flu wreaks havoc on the body, but it is more so for PWD.
Diabetes weakens the immune system, leaving PWD more susceptible to the flu.
A changed eating pattern combined with dehydration can make it difficult to manage blood sugar levels.
PWD are at an increased risk for complications from the influenza virus, like bronchitis, worsening heart diseases, and pneumonia.
The risk is even higher in those over 65 with diabetes.
Further, the incidences of other chronic conditions like chronic obstructive pulmonary disease (COPD), hypertension, and renal diseases are higher in PWD.
This puts them at higher risk for complications and hospitalizations due to the influenza virus.
Researchers have identified several genes associated with diabetes.
In the sample report below, we've attempted to analyze some important genes that increase the risk of diabetes.
You can identify your genetic risk of diabetes by using your 23andMe DNA data and placing an order for the Gene Health Report.
In the United States, flu viruses are common in fall and winter.
It can begin to peak during October and November and may extend up to early May.
The timing can, however, vary with each season.
According to the CDC, the longest stretch of flu season was from Oct 01, 2018, to May 04, 2019, at that time.
The 2020 and 2021 years saw lower incidences of flu due to increased precautionary methods adopted in light of the COVID pandemic.
However, this year (2022-2023) flu season, many experts suggest, will bring in many more flu cases in the United States than in recent years.
Yearly flu shots are advisable for everyone, including PWD, autoimmune disorders, and mothers with gestational diabetes.
30% of adults hospitalized due to flu in the last few seasons had some type of diabetes.
Further, PWD are three times more likely to have severe COVID than those without diabetes.
So, it is important for all PWD and their families to get their flu shots.
Since the strain of virus emerging every year is different, the CDC recommends yearly flu shots.
According to the CDC, there are several types of flu vaccines:
| Flu Shot | Description |
| Standard dose flu shots | Traditional vaccine |
| Cell-based flu shots | Approved for people 6 months and older |
| Recombinant flu shots | Stronger immune response, shorter shelf life |
| High-dose flu shots | For the elderly (65 years and above) |
| Adjuvant flu shots | For the elderly; contains an adjuvant to boost immune response |
| Nasal spray vaccine | Made with weakened live flu viruses; not recommended for pregnant or immunocompromised people |
According to the CDC, the best vaccine for PWD is injectable dead-virus flu vaccination due to its long-established safety record.
The immune system reacts to the dead/weakened virus in the vaccine, causing the blood sugar levels to spike, just like an infection would.
However, there’s not much research to explain how flu shots can lead to higher blood sugar levels.
According to a report in the Annals of Pharmacotherapy, there has been only one report of an unusual spike in blood glucose levels after vaccination.
However, their healthcare team could not identify a specific reason for the glucose rise, nor did they mention that it was caused directly by the flu shot itself.
This 2022 study included 34 adults with an average age of 75 years with diabetes during the 2018 to 2020 flu seasons.
The researchers examined their blood sugars in the first 24 hours after they got their vaccinations.
They reported higher blood glucose levels on the first day after the flu shot.
The levels returned to baseline by the second day.
The study authors say that they agree with vaccination recommendations for PWD and that the benefits outweigh the risk of transient, acute hyperglycemia.
Diabetes affects immune functioning, and therefore people with diabetes (PWD) are at a higher risk for flu-related complications and hospitalizations.
The CDC recommends everyone, especially PWD get their yearly flu vaccinations.
The best vaccine for PWD is injectable dead-virus flu vaccination due to its long-established safety record.
Spikes in blood sugar levels may be observed a day post-vaccination, but the levels return to baseline the following day.
There may be a small risk for transient acute hyperglycemia following vaccination, but the vaccination benefits for PWD outweigh this risk.
Myopia or nearsightedness is a common eye condition in which individuals cannot clearly see distant or far-away objects.
According to the American Academy of Ophthalmology, nearly half the world’s population will have nearsightedness by 2050.
Nearsightedness among children increases as they grow old, and their glasses prescription usually stabilizes in their 20s.
Myopia is a complex condition that affects the structure of the eye.
When the eyeball is too long, or the cornea (protective outer layer of the eye) is too curved, light that enters the eye is not focussed properly.
As a result, the image is focused in front of the retina rather than on it. This causes blurred vision and is called a refractive error.
Though myopia's exact cause is unclear, it is said to develop due to an interaction between genetic and environmental factors.
In high myopia, the eyeball grows more than normal and becomes long from front to back.
Apart from myopia, people with this eye structure are also at a greater risk for cataracts, glaucoma and detached retina.
Degenerative myopia is a type of nearsightedness that an individual typically inherits from their parents.
In this type of myopia, the eyeball elongates too quickly and causes severe myopia. This condition worsens into adulthood.
People with degenerative myopia are at a higher risk for other visual conditions like a detached retina, glaucoma, and abnormal vessel growth in the eye.
Image: Overview of Myopia
Researchers have found over 200 genes associated with myopia and refractive errors.
In some people who inherit myopia, lifestyle factors like reading a book, using a laptop, or watching the TV from a close distance can result in nearsightedness.
Myopia usually appears in childhood. The condition may settle down or worsen with age.
Researchers at Columbia Medical Center have discovered a gene that may increase the risk of myopia in people who spend a significant amount of time doing near-work like childhood reading.
People with a variant of the APLP2 gene are five times more likely to develop myopia in their teens if they read for at least one hour per day in their childhood.
People with the APLP2 gene but who spent less time reading had no additional risk of developing myopia.
Myopia is a complex condition influenced by many genes and environmental factors, it does not have a clear inheritance pattern.
Some studies show that myopia can be inherited, as you are more likely to develop the condition if one or both of your parents have it.
The risk of myopia is greater when first-degree relatives like parents and siblings of the individual have the condition.
High myopia occurs when an abnormal change (mutation) in a single gene exists.
This form of nearsightedness follows an autosomal dominant (having one copy of the affected gene can cause the condition), autosomal recessive (having two copies of the affected gene causes the condition), or X-linked ( when the affected gene is present on the chromosome and is sufficient to cause the condition in males) inheritance pattern.