Though most oral health conditions are preventable, 3.5 billion people worldwide suffer from cavities, gum diseases, and oral cancer. According to the Centre for Disease Control, 90% of adults 20 years and older have had at least one cavity in their permanent teeth during their lifetime. While some people have chronic and frequent dental cavity issues, other people avoid dental visits for years at a stretch! Could this mean dental cavities are genetic?
What Are Dental Cavities?
Dental cavities or regions of tooth decay are permanently damaged areas of tooth structure that result in cavitation(the formation of a hole) in the tooth’s structure.
Dental cavities occur due to:
- Cavity-causing bacteria in the mouth
- Consumption of sugary foods and beverages
- Frequent snacking
- Poor oral hygiene habits (improper brushing and flossing)
- Genetics
How Do Dental Cavities Occur?
Dental plaque is a thin, colorless, sticky film that covers the surfaces of teeth.
It harbors bacteria, food particles, and saliva when you eat.
If you don’t brush your teeth properly, plaque builds up and can harden.
Hardened plaque is called tartar; this layer is difficult to remove with simple brushing.
Dental plaque is an essential factor in the initiation of tooth decay.
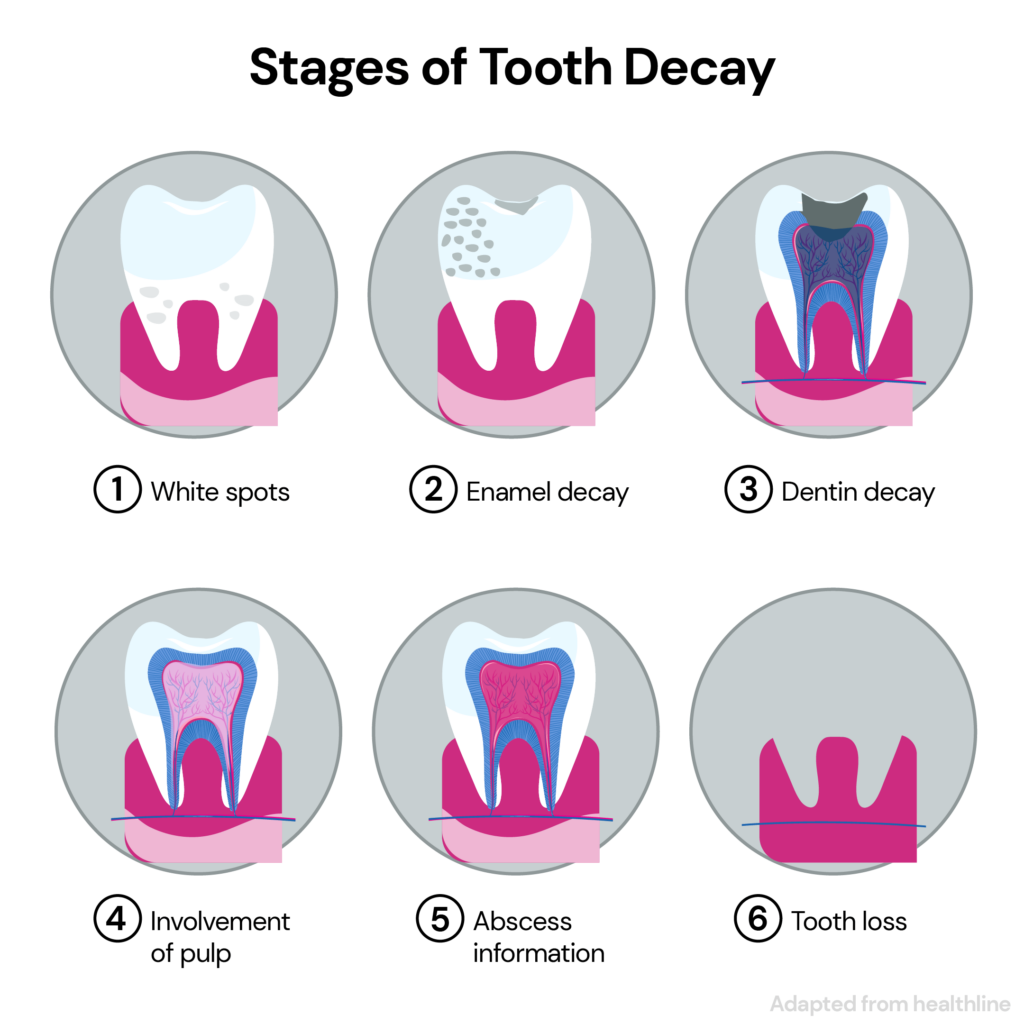
Stages Of Tooth Decay
Tooth cavities occur in five stages:
Early or Initial Demineralization
Bacteria in the plaque begin to produce acids.
These acids start demineralizing (dissolving) the enamel, the outer layer of your tooth.
As enamel begins to lose minerals, it forms a white spot on the teeth.
Enamel Decay
The white spot darkens to a brownish shade as the enamel breaks down further.
It eventually forms a cavity that a dentist can fill up and prevent from worsening.
You may not have any other signs or symptoms at this stage.
Dentine Decay
The decay progresses into the middle tooth layer, called the dentine.
Dentine is softer than enamel and tends to decay faster.
The dentine layer houses the tooth nerves.
That’s why your teeth suddenly become sensitive to hot or cold foods or drinks.
Pulpal Damage
The decay reaches the innermost layer of the tooth, called the pulp.
The pulp contains nerves and blood vessels that nourish the tooth.
When tooth decay irritates the pulp, it starts to swell.
The pulp cannot swell freely since the tooth’s structure is firm.
It begins to apply pressure on the nerves and tissues below.
This pressure triggers the pain commonly associated with cavities.
Abscess Formation
An inflamed pulp causes an abscess (a pocket of pus) to form at the bottom of your tooth.
The infection could spread to nearby tissues if abscesses aren’t immediately addressed and drained.
The treatment for tooth cavities depends upon the stage at which you report to your dentist.
It can range from a simple filling to a tooth removal.
Are Cavities Genetic? 5 Ways Genes Affect Tooth Decay Risk
There is ample research to show that cavities are genetic.
Genes influence various factors that could increase your risk for cavities.
Enamel Structure
Amelogenesis is the process of the formation of the enamel.
This process determines the tooth’s size, shape, color, and likelihood of decay.
Genes could alter the proteins that are a part of this process.
This change, in turn, could affect the likelihood of cavity formation.
Immunological Response
Streptococcus mutans is a bacterium present in a healthy oral cavity.
Your immune response influences the growth of this bacteria in the mouth.
Some gene changes result in weaker immune responses, which can lead to irregular growth of S.mutans.
This bacterial growth can increase your risk of cavities.
Sweet Taste Preference
Some people have a genetic inclination to prefer sweet food more than others.
They seek out higher amounts of sweet foods.
Eating too many sweet foods can increase your risk of tooth cavities.
Nature, Flow, And Composition Of Saliva
Saliva flow and consistency play a role in tooth decay and other oral diseases.
When saliva is thin and free-flowing, it can easily wash away bacteria from your teeth.
Thinner saliva reduces your risk of gum disease or other infections.
On the other hand, having less saliva increases the risk of tooth decay.
Studies have shown that women have less saliva than men, putting them at risk for tooth decay.
Saliva comprises various electrolytes, including sodium, potassium, calcium, magnesium, bicarbonate, and phosphates. They help inhibit caries formation and progression.
Specific gene changes result in inadequate electrolytes in saliva, increasing the risk for cavities.
Oral Microbiome
The oral microbiome is the collection of microbes residing in your mouth.
It can lead to the development of numerous oral infectious diseases, including dental caries, periodontitis, and peri-implant disease.
Genetic factors can contribute to the imbalance in the gut microbiome, resulting in an increased risk for all these conditions.
An imbalanced gut microbiome increases your risk for all these conditions.
Other Factors That Influence Cavity Formation
Besides the causes of tooth cavities mentioned above, other lesser-known factors include:
- Snoring
- Constant snacking
- Missed dental visits
- Improper tooth brushing and flossing
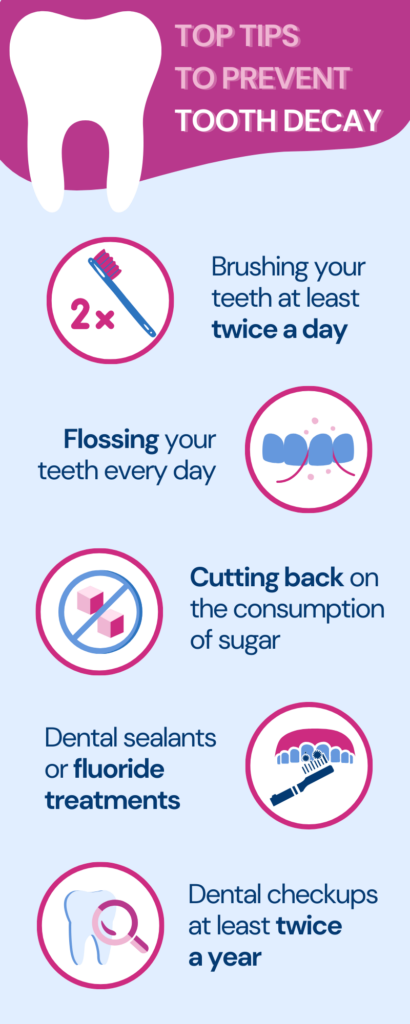
5 Effective Tips To Prevent Genetic Cavities
Tooth cavities are highly preventable, and here are a few practical tips for doing so, regardless of genetics:
- Brushing your teeth at least twice daily with a soft or medium-bristled toothbrush.
- Flossing your teeth every day to help remove food debris between teeth
- Cutting back on the consumption of sugary foods and beverages
- Dental sealants or fluoride treatments in people, especially children, who are more prone to dental caries
- Dental checkups at least twice a year or as recommended by your dentist
Frequently Asked Questions
Can You Reverse Cavities?
Enamel damage can heal over time.
A cavity that has reached the dentine or pulp needs medical attention.
Is A Black Spot On A Tooth A Cavity?
It isn’t always the case.
Certain foods can leave some stains on your teeth, discoloring them.
Can Mouthwash Get Rid Of Cavities?
Mouthwash can significantly reduce the probability of getting a cavity.
However, an existing cavity from tooth decay needs medical attention.
Summary: Are Cavities Genetic?
- Tooth cavities are one of the most common oral health diseases.
- They occur due to sugary food consumption, frequent snacking, poor oral hygiene, and genetics.
- Tooth cavities occur in five stages – early demineralization, enamel decay, dentin decay, pulp decay, and abscess formation.
- Your genes determine factors like saliva consistency and nature, immune response, and enamel structure, which can increase the risk of tooth cavities.
- Brushing and flossing your teeth, regular dental checkups, and controlling your sugar intake can help prevent tooth cavities.
Others Are Also Reading

Bad Teeth Genes: Can Dental Issues Run In Families?

Are UTIs Genetic?

How It Works: Are Freckles Genetic?




