Around 25-50% of people with ADHD also have an anxiety disorder, and a significant portion of adults with ADHD also have at least one other psychiatric disorder, such as an anxiety disorder. This means that anxiety can be misdiagnosed as ADHD, and vice versa. Getting the right diagnosis is important because the treatments for ADHD and anxiety are different. What helps with the lack of focus in ADHD may not work for the constant worry associated with anxiety. Understanding their differences & similarities is the first step towards proper care.
Attention-deficit/Hyperactivity Disorder (ADHD) is a long-term mental health condition that typically starts in childhood and may extend into adulthood.
Three main symptoms characterize it:
These symptoms interfere with various aspects of life, including academic performance, professional development, relationships, and daily activities.
When left untreated, ADHD can impact self-confidence and social interactions in children and may lead to lasting emotional challenges in adulthood.
ADHD is more commonly recognized in boys because their symptoms (impulsivity and hyperactivity) are much more noticeable.
Girls have less visible ADHD symptoms, which are easier to overlook or misunderstand.
According to research, approximately 8.4% of children and 2.5% of adults have ADHD.
While the signs may evolve with age, early diagnosis and proper support are essential to managing symptoms effectively and improving long-term outcomes.
Anxiety is an automatic response to stress that helps individuals stay alert, focused, and prepared.
At moderate levels, anxiety can be helpful by signaling danger or enhancing performance.
However, when fear or worry becomes intense and constant, it may point to an anxiety disorder.
These disorders, affecting nearly 30% of adults, differ from everyday nerves thanks to a persistent fear that disrupts daily life.
On a positive note, they are treatable through various psychotherapeutic approaches, allowing most people to lead stable, productive lives.
People with anxiety disorders may stay away from situations that worsen their symptoms, which can impact work, school, and relationships.
For a diagnosis, the symptoms must:
Types of anxiety disorders include:
Timely treatment improves outcomes and can help individuals regain control over their lives.
The 3-3-3 rule for anxiety is a practical method that helps shift focus during stressful moments through three simple actions:
This approach can help refocus your attention and reduce anxious feelings.
Since ADHD and anxiety can be confusing to tell apart due to overlapping signs, the table below breaks down their symptoms for easier comparison.
| Symptom | ADHD presentation | Anxiety presentation | Overlap? |
| Concentration issues | Hard to pay attention because of distractions or boredom. | Hard to focus because of constant worrying or racing thoughts. | ✅ |
| Agitation | Restless, unable to stay still or calm, with a jumpy mind. | Tense muscles, feeling nervous, or unable to relax. | ✅ |
| Procrastination | Delays tasks due to stress or trouble staying. | Delays tasks due to fear of failure or being too worried about doing it right. | ✅ |
| Emotional instability | Quick mood changes like getting upset or excited easily. | Long-lasting negative feelings (e.g., unease, distress). | ❌ |
| Sleep problems | Trouble falling asleep because of too many thoughts or restlessness. | Trouble sleeping due to overthinking or body tension. | ✅ |
| Impulsiveness | Says or does things suddenly, like speaking out of turn or making risky choices. | Rare; tends to think too much and avoid taking risks. | ❌ |
| Physical symptoms | Usually, few, unless there's anxiety too. | Common, like fast heartbeat, sweating, or stomach pain. | ❌ |
| Time management | Often late or misses deadlines (has trouble sensing time). | Spends too much time planning or worrying about tasks. | ❌ |
| Social behavior | Talks a lot, interrupts, or seems overly active. | Stays quiet, avoids people, or worries a lot about what others think. | ❌ |
| Underlying cause | Brain development issues affect attention and activity levels. | Strong reaction to threats, often from stress, genes, or life experiences. | ❌ |
Disclaimer: This comparison is intended for informational purposes only and does not constitute medical advice or a clinical diagnosis. Individual experiences of ADHD and anxiety can vary widely. If you suspect you may have ADHD, an anxiety disorder, or both, please seek evaluation from a qualified healthcare professional.
Both ADHD and anxiety can affect people differently, often starting in similar ways, with their causes and risk factors influencing their development.
ADHD:
Scientists don't fully understand exactly why ADHD occurs, but several key factors are often involved.
Genetics plays a significant role, so if a close family member has ADHD, the chances increase.
It may also be connected to environmental factors or developmental issues in the brain during critical early stages of life.
Anxiety:
The causes of anxiety aren't entirely understood, but it often comes from a mix of things, and it's different for everyone.
It can often stem from stressful or traumatic life events, especially if you're already prone to feeling anxious.
Family history can add to the risk, as anxiety can be passed down through generations.
In some cases, anxiety may have links to underlying medical conditions, such as:
Anxiety linked to a medical issue is more likely when there's no family history, no childhood anxiety, and when symptoms appear suddenly without a clear trigger.
ADHD:
Anxiety:
People frequently mix up ADHD and anxiety since both can impact concentration, but there are clear differences if you know what to look for.
The key is to notice when the focus issues happen and what symptoms accompany them.
| ADHD | Anxiety |
| Trouble focusing even when things are calm | Trouble focusing mostly in anxiety-triggering situations |
| Anxiety often shows up because of problems caused by ADHD | Can cause ongoing, constant worry or nervousness |
| Common signs include forgetfulness, impulsivity, a short attention span, and restlessness. | Common signs include feelings of unease or danger, sweating, shaking, and a fast heartbeat. |
If both ADHD and anxiety are present, a person may struggle to concentrate in many different situations, which can make daily life more difficult.
Anxiety often brings worry that disrupts focus, while ADHD is a developmental condition with ongoing attention and/or hyperactivity-impulsivity issues since childhood.
A professional evaluation is key to a correct diagnosis because the underlying causes differ.
Distinguishing between ADHD and anxiety is essential because both conditions are treated and managed in unique ways.
Correctly diagnosing and treating ADHD vs. anxiety is crucial because their approaches differ.
A healthcare professional may use questionnaires and interviews to diagnose ADHD.
They also use criteria from the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text revision (DSM-5-TR), which includes:
ADHD treatment usually includes:
Anxiety is diagnosed through:
Treatment for anxiety includes:
Since ADHD and anxiety can occur together, diagnosing and treating them carefully is essential.
According to a 2022 research article, stimulant medications for ADHD, like Adderall, may not make anxiety worse and could help with both conditions.
Non-stimulant medications like atomoxetine can also be useful for people with both ADHD and anxiety.
It's important to consult with a healthcare professional for the right treatment.
When deciding whether to address ADHD or anxiety first, the key is to focus on which symptoms are most disruptive.
If anxiety is severe and there's a family history, it's often best to manage anxiety first. Once it's under control, ADHD can be addressed if needed.
However, if inattentiveness is causing more significant issues, it's better to prioritize ADHD, assuming anxiety symptoms are mild.
Ultimately, a healthcare practitioner will decide which condition to address first.
Yes, anxiety can make it harder to distinguish between ADHD and anxiety itself.
Both conditions cause distractibility, restlessness, and difficulty focusing, but the root causes differ.
Overthinking happens in both ADHD and anxiety, but the reasons behind it are different.
ADHD usually occurs due to fast, scattered thoughts and trouble focusing, which can overload the mind.
In anxiety, overthinking is more about constant worry and going over the same fears or negative thoughts again and again.
Sometimes, both conditions can happen together, making diagnosing and treating harder.
Sympyoms like inattention and restlessness make it easy to mistake anxiety for ADHD.
However, if these symptoms come from worry or fear rather than difficulty in focusing, anxiety may be the primary cause.
High-performing anxiety is when a person has anxiety but still functions well in daily life.
They may have a successful career and an active social life and seem in control, but inside, they struggle with constant worry, fear, and self-doubt.
It's not an official diagnosis and is usually considered a form of generalized anxiety disorder.
These individuals hide their stress and keep pushing through instead of avoiding situations.
Doctors first check whether ADHD causes your anxiety or if it’s a separate issue, and then treat the condition that affects you the most.
Before giving any medicine, doctors examine your age, health, and other medical problems.
They also check for side effects and how the medicine might react with others.
So, you may need ADHD or anxiety meds, depending on which condition is more serious and what suits your overall health.

Can L-theanine Help Manage ADHD Symptoms? What Science Says.

Does Magnesium Help With Anxiety? Experts Weigh In
How Does Anxiety Affect Your Brain?
https://www.psychiatry.org/patients-families/adhd/what-is-adhd
https://medlineplus.gov/anxiety.html
https://www.webmd.com/anxiety-panic/anxiety-disorders
https://www.drakeinstitute.com/adhd-vs-anxiety-whats-the-difference
https://www.mayoclinic.org/diseases-conditions/adhd/symptoms-causes/syc-20350889
https://www.mayoclinic.org/diseases-conditions/anxiety/symptoms-causes/syc-20350961
https://add.org/add-vs-anxiety/
https://www.medicalnewstoday.com/articles/adhd-vs-anxiety
https://www.medicalnewstoday.com/articles/best-adhd-medication-for-adults-with-anxiety
Two completely different conditions look the same at first glance. One is harmless and just skin-deep, but one is a silent disease progressing. Despite affecting 11% of women worldwide, lipedema is frequently overlooked or misdiagnosed as harmless cellulite, delaying much-needed medical attention. Lipedema vs. cellulite: which is it? This article unpacks the differences between lipedema and cellulite, helping you understand what your body might be trying to tell you.
Cellulite and lipedema are often discussed together due to their impact on appearance, but they are distinct conditions with unique causes and symptoms:
| Feature | Lipedema | Cellulite |
| Definition | A medical concern where fat builds up in certain areas and affects tissues | A cosmetic condition where fat collects under the skin |
| Appearance | Swollen, uneven, dimpled, or bumpy skin | Dimpled, bumpy, or uneven skin without swelling |
| Causes | Unclear, may involve hormones or genetics | Involves weight, diet, hormones, genetics, or pregnancy |
| Symptoms | Pain, swelling, bruising, and limited flexibility in affected areas | Usually harmless and does not cause physical discomfort |
| Treatment | Decongestive therapy, compression, a healthy lifestyle, or liposuction | Creams, laser treatments, radiofrequency, and lifestyle changes |
Lipedema often goes unnoticed early on, but knowing its signs can help you get the proper care.
It typically affects the lower half of the body, with symptoms that go beyond ordinary weight gain.
Common symptoms of lipedema include:
Though lipedema fat doesn't typically respond to standard weight loss methods, several treatments can help manage symptoms and make daily activities easier.
Treatment options include:
Since lipedema is different from regular obesity, it requires a personalized treatment plan.
Consider talking to a healthcare provider to find the best approach for you.
The pinch test is a quick and simple method often used to spot early signs of lipedema.
It involves gently pinching the skin and deeper tissue in areas where lipedema usually appears, such as the thighs or lower legs.
Focus on how the tissue feels between your fingers and whether there’s any pain.
Regions affected by lipedema may feel tender and have a different texture compared to other body parts.
You could feel lumps beneath your skin, like small beans, which could point to fibrotic tissue.
For a confirmed diagnosis, consult a specialist for a complete evaluation.
It’s often hard to get insurance approval for a liposuction procedure to treat lipedema.
Most insurance companies view it as cosmetic unless it’s medically urgent.
You may need to prove that:
Insurance providers often require medical records to corroborate this, including:
Some plans may also include extra conditions, such as requiring:
Despite providing every requested document, the final decision is at the insurance company’s discretion.
Knowing your policy well and working closely with your doctor can help increase your chances of approval.
Cellulite appears in different forms and levels, depending on its severity.
Common signs of cellulite include:
The severity of cellulite is classified into four grades:
Cellulite can't be entirely removed, but its appearance can be reduced.
Mixing healthy lifestyle habits, medical treatments, and traditional methods can help improve skin appearance.
1. Lifestyle changes:
2. Medical treatments:
3. Traditional methods:
Important Note: Everyone’s skin is different. To find out what would work best for you, consult a professional.
It’s hard to discern lipedema from cellulite at first glance, but there are a few key things to pay attention to.
If the area feels tender, bruises easily, or swells in the lower body, it might be lipedema.
Cellulite, on the other hand, neither hurts nor causes swelling.
It affects the skin’s appearance, not its feel.
Lipedema is often mistaken for obesity or lymphoedema because of overlapping signs like swelling and fat buildup.
Both conditions share some visual similarities but differ in origin and progression.
Obesity causes fat to build up all over the body, but lipedema leads to painful fat buildup mainly in the legs and arms, and it doesn’t improve with diet or exercise.
Lymphoedema, meanwhile, is caused by fluid buildup due to lymphatic dysfunction, which can lead to swelling but lacks the symmetrical fat pattern seen in lipedema.
In some advanced cases, lipedema can progress to affect the lymphatic system or blood vessels, making diagnosis more difficult.
Although lipedema and cellulite may seem similar at first glance, their appearance, texture, and patterns on the body are quite different.
If your legs feel unusually heavy, painful, or tender and look much larger than your upper body, it could be lipedema.
Lipedema fat also tends to feel lumpy under the skin.
Normal fat doesn’t usually cause pain or create a clear difference between body areas.

Are Stretch Marks Genetic?

How Genes Influence The Risk Of Cellulite

How It Works: Are Freckles Genetic?
https://pmc.ncbi.nlm.nih.gov/articles/PMC5055019
https://www.healthline.com/health/lipedema-vs-cellulite
https://www.webmd.com/women/lipedema-symptoms-treatment-causes
https://www.medicalnewstoday.com/articles/lipedema-stages
https://legalclarity.org/does-insurance-cover-lipedema-surgery-what-you-need-to-know/
https://my.clevelandclinic.org/health/diseases/17694-cellulite
https://pmc.ncbi.nlm.nih.gov/articles/PMC7949771
Touted as a brain booster, a lung cleanser, and everything in between, N-acetylcysteine (NAC) is gaining popularity in the medical and pharmaceutical community. Some say it supports fertility, others hail it a powerful liver protector, yet others believe it improves mood and mental clarity. With so many claims surrounding this supplement, it’s hard to know whom to believe. As interest in NAC grows, so does the need for answers. What is NAC, and what does science say about its benefits? Let’s take a look at the research behind it, known effects, and the gaps that still remain.
N-acetylcysteine (NAC) is a supplement form of cysteine, a semi-essential amino acid.
The supplement is engineered for better absorption and stability in the body, allowing it to work more effectively than cysteine.
NAC supports the production of glutathione, an antioxidant that stabilizes cellular functions.
Medically, it helps manage paracetamol/acetaminophen overdoses.
Recently, it has been shown to loosen mucus (mucolysis) from airways in respiratory conditions.
NAC is FDA-approved and the WHO has listed it as an essential medicine.
It is available over the counter in countries like the United States, Canada, and Australia.
Though widely studied, its effectiveness can vary across different health conditions in clinical practice.
NAC continues to generate interest for its potential health benefits. While some claims are supported by strong evidence, others are still being studied.
Here’s a quick look at the top 7 benefits of NAC:
NAC’s treatment for acetaminophen overdoses is its only medically proven application.
It helps the body make more glutathione to clear out the harmful effects of acetaminophen.
If given within 8-10 hours of an overdose, it can prevent severe liver and kidney damage.
NAC can be administered intravenously for faster action.
NAC provides the required building blocks for the production of glutathione, one of the body's most beneficial antioxidants.
This increase in glutathione may help:
Since NAC helps boost antioxidant levels, its role in cell health, immune function, and detoxification is vital.
Some research suggests it can reduce the risk of chronic conditions like heart disease, though more studies are needed to understand the complete picture.
NAC supports detoxification by helping the kidneys flush out harmful substances more effectively.
Early findings suggest it may benefit individuals with kidney issues, though further studies are required.
When it comes to lung health, NAC shows potential for reducing inflammation and breaking down mucus, particularly in chronic respiratory conditions like:
In higher doses (1200mg/day) or when inhaled, NAC could potentially reduce coughing, enhance airway function, and minimize oxidative stress.
NAC may help protect brain function by reducing inflammation and oxidative damage.
Along with increasing glutathione, it supports the balance of glutamate, an essential neurotransmitter in the brain.
These actions may support brain cell survival and reduce the progression of damage seen in neurodegenerative disorders such as:
While currently promising, more human studies are needed before NAC becomes a standard part of treatment for these conditions.
NAC has shown benefits for both male and female reproductive health.
In studies, it has been linked to:
These results indicate NAC’s potential as a supportive supplement in specific fertility treatment plans.
Research suggests NAC may improve insulin resistance, particularly in people with PCOS.
Insulin resistance develops when the body doesn’t respond well to insulin, affecting blood sugar processing.
While NAC may help:
Studies haven’t confirmed how well it helps with blood sugar in type 2 diabetes.
NAC is being studied for its impact on mental health and addiction recovery.
It appears to influence brain chemicals linked to mood and repetitive behavior.
Early research shows potential benefits in reducing symptoms related to:
Additionally, NAC shows promise in addressing substance use disorders (SUD), potentially easing withdrawal symptoms and reducing cravings.
The need for NAC usually arises in people dealing with ongoing physical or mental strain.
It’s often considered by:
Taking NAC every day may be safe for a short period, especially when used for a specific health purpose.
However, long-term safety isn't clear yet, as most studies focus on use between 6 weeks and 6 months.
Side effects are rare at low doses, but the effects of prolonged use are still unclear.
Discussing your plans with a healthcare professional can help you decide whether daily NAC fits your health needs.
You can take NAC in the morning or at night, depending on the purpose and dosage.
Since it may interact with other medications or supplements, a healthcare provider will often recommend the best timing as part of your overall health plan.
Specific individuals should avoid NAC to prevent potential health risks and complications.
Here are those who should refrain from using it.
NAC supplements are generally considered safe for adults when prescribed by a healthcare provider.
However, taking high doses can result in side effects, including:
Inhaling NAC solutions can cause symptoms like:
NAC's main purpose is to support the body's antioxidant and anti-inflammatory processes.
It helps maintain cellular balance by reducing oxidative stress, making it beneficial for conditions where oxidative stress contributes to disease development and progression.
NAC supports brain health by helping replenish glutathione levels, which protect the brain against oxidative stress.
This protective effect may contribute to better cognitive function and reduced cognitive decline.
Preclinical studies show that NAC can lower oxidative stress markers and lessen the severity of cognitive dysfunction in animal models.
With more research, we can better understand its impact on human brain health.
NAC may make you feel good because it supports key brain processes linked to mood and mental health.
One of its leading roles is balancing glutamate, a brain chemical linked to emotions and thinking.
This balance can help relieve symptoms related to depression, anxiety, obsessive-compulsive behavior, and even the negative symptoms of schizophrenia.
Some people may notice improvements only after using NAC for several months, as many clinical studies suggest extended treatment periods are more effective.
NAC may help improve brain fog, especially in individuals experiencing ongoing cognitive difficulties after viral infections like COVID-19.
In a small clinical observation, twelve patients with reduced memory, concentration issues, and mental task difficulties received 600 mg of NAC daily with guanfacine.
The results were as follows:
NAC contributed to better brain health by protecting mitochondria and decreasing kynurenic acid levels that interfere with normal brain signaling.

NMNH Supplements: The Good And The Bad
Best BDNF Supplements To Boost Brain Function

Top 7 “Natural” Supplements Associated With Liver Damage
https://www.healthline.com/nutrition/nac-benefits
https://www.webmd.com/diet/health-benefits-nac
https://pmc.ncbi.nlm.nih.gov/articles/PMC8234027
https://www.webmd.com/vitamins/ai/ingredientmono-1018/n-acetyl-cysteine-nac
https://www.sciencedirect.com/science/article/abs/pii/S0149763416303980
https://pmc.ncbi.nlm.nih.gov/articles/PMC9095537
https://www.sciencedirect.com/science/article/pii/S2667257X22001000
Two brothers grow up in the same home with the same parents and even the same blue eyes. Yet, one is taller, the other has a deeper voice, and their personalities couldn’t be more different. How does that happen if their genes come from the same place? The secret lies in the difference between genotype and phenotype. A flamingo isn’t born pink—it turns pink because of what it eats. Identical twins inherit the same blueprint, but their environment and experiences add unique twists. Science is uncovering more about this connection every day, expanding our knowledge of genetics, health, and evolution. Are we defined by our DNA or our surroundings? Let’s break it down and find out.
Genotype and phenotype are closely related terms that represent different aspects of an organism.
One refers to its genetic makeup, while the other describes how those genes manifest.
The table below highlights their key differences.
| Feature | Genotype | Phenotype |
| Definition | Genetic makeup of an organism (alleles inherited from parents). | Observable traits resulting from genotype and environment. |
| Inheritance | Directly inherited from parents. | Not inherited; influenced by genetic and environmental factors. |
| Assessment | Detected via methods like DNA sequencing, PCR, or genotyping assays. | Determined through observation (e.g., eye color) or measurement (e.g., height). |
| Stability | Stable throughout life (except for mutations). | Can change due to environmental influences. |
| Role in evolution | Changes through mutations or recombination, influenced by natural selection. | Direct target of natural selection (e.g., traits affecting survival/reproduction). |
| Variability in twins | Identical in monozygotic twins. | Differ due to the environment. |
A genotype is the complete set of genetic blueprints (a DNA sequence) an organism inherits from its parents.
These blueprints sketch out characteristics, but how they manifest can depend on various factors.
Genotypes come in allele pairs representing a trait's dominant and recessive versions.
For example, when considering height, the dominant allele promotes greater height, while the recessive allele promotes lesser height.
When two of a kind occur together, that version of the trait is selected and expressed, but when both alleles occur together, the dominant trait takes priority and is expressed.
The most common types are:
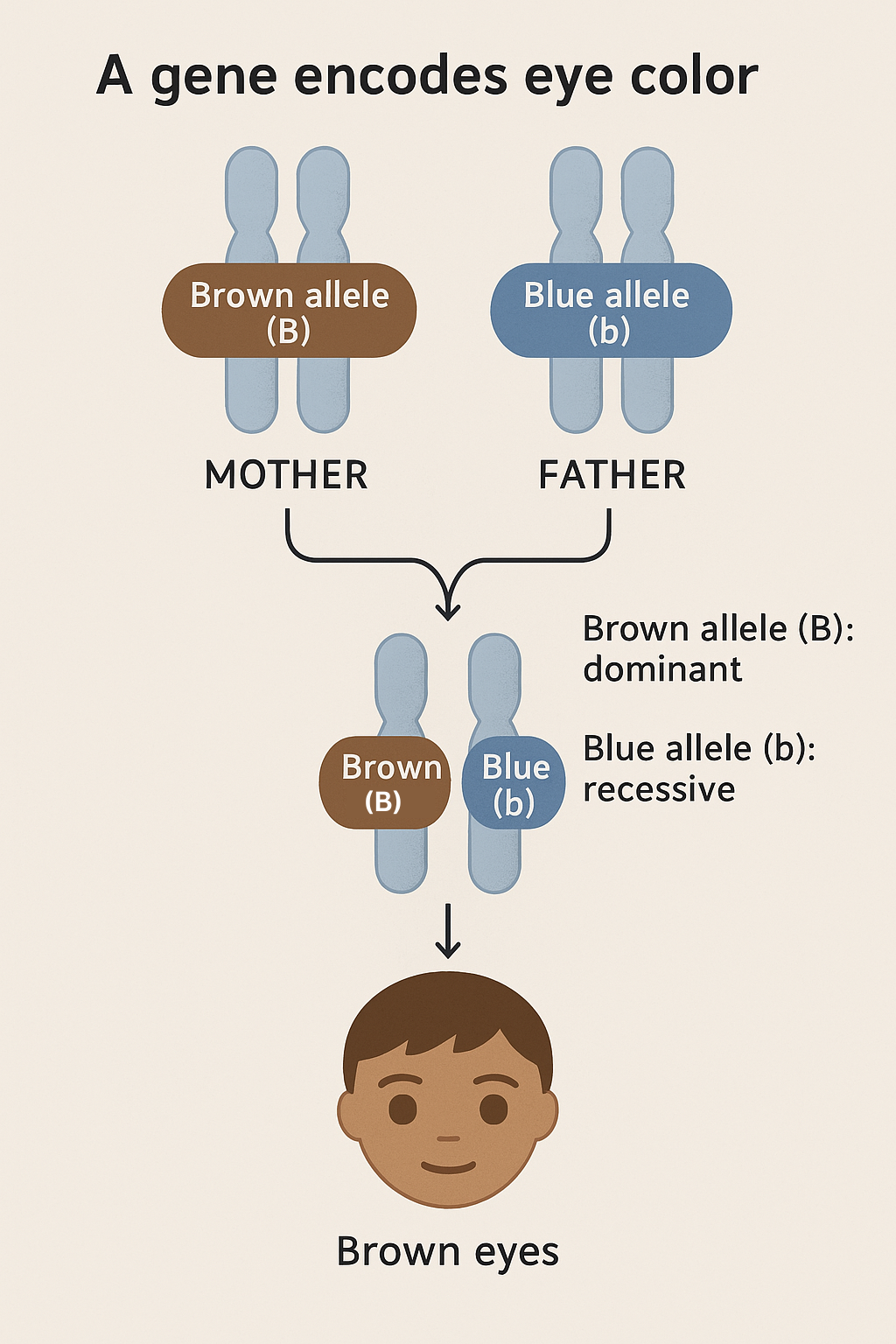
Eye color is a well-known example of how genotypes work.
A person receives one allele from each parent, and how dominant and recessive genes work together influences their eye color.
The mother contributes a brown allele (B), and the father contributes a blue allele (b).
Because brown (B) is dominant and blue (b) is recessive, the child with one of each allele has brown eyes.
The same genetic process plays a role in other traits, like hair color and height.
This process of inheriting alleles and the resulting eye color is illustrated in the image below.
Phenotype consists of all an organism's observable traits, influenced by genetic factors and environmental conditions.
While an individual's genes provide the blueprint, the expression of these traits isn't entirely genetic.
Non-genetic factors such as climate, nutrition, and biological processes can modify the expression of traits.
Flamingoes are genetically wired for certain colors, but pigments in their diet can influence the exact shade we see.
The image below shows that flamingos display different shades depending on their diet, highlighting how the environment shapes phenotype.

Genotype and phenotype don’t always have a clear connection, even though both play key roles.
To strengthen this connection, genome-wide association studies (GWAS) analyze genetic variants and link them to specific traits.
These studies often help understand the mechanisms behind complex traits and diseases.
Through techniques like next-generation sequencing (NGS) and whole-genome transcription profiling, researchers may better understand how genes influence traits.
Additionally, changes in DNA sequences have been linked to differences in traits among individuals and species.
Evolution happens when the genes of living things change over time, influencing how species grow and adapt.
These gene changes, known as genotype changes, play a key role in evolution.
Small changes in DNA, called mutations, introduce new traits, while gene mixing during reproduction creates fresh combinations.
Some traits are more evolutionarily favorable than others for an organism’s survival.
They are retained through an evolutionary process called natural selection.
Over time, nature selects the traits that help organisms survive, a process known as natural selection.
For example, as seen in the image below, a caterpillar’s skin color changes to adapt best to the temperature of its surroundings.
Though it carries genetic blueprints for several colors, it selects the shade most favorable for survival.

Organisms that are better adapted to their environment survive longer and can pass these favourable genes and traits to the next generation.
Yes, phenotypes can change, as they are not fixed and can be influenced by environmental conditions.
Traits such as body structures, behaviors, and even molecular expressions can shift in response to different surroundings.
External factors influence these changes as an organism develops.
Phenotypes can even influence the interactions between organisms and their environment.
Genotype analysis identifies differences in DNA using various techniques.
Large-scale methods examine multiple genetic markers simultaneously, while smaller studies focus on specific variations.
Common techniques for genotype analysis include:
These techniques reveal whether a person carries one or two copies of a gene variant, helping estimate their likelihood of expressing a certain trait.
GWAS and quantitative trait loci (QTL) mapping help link genetic variations to specific traits.
Phenotype analysis studies observable traits influenced by genes and the environment.
Modern tools allow large-scale, non-destructive data collection.
Key techniques in phenotype analysis include:
Unlike genotype analysis, phenotypic traits change over time due to environmental factors.
Combining genotype and phenotype data helps understand inheritance patterns.
GWAS and QTL mapping are key in linking genetic variations to specific traits, helping researchers understand inheritance patterns.
However, challenges like pleiotropy (one gene affecting multiple traits), epistasis (gene interactions), and environmental effects complicate analysis.
Careful study design helps achieve accurate results by minimizing errors.
The AS genotype means a person has one normal hemoglobin gene (A) and one sickle cell gene (S). They carry the sickle cell trait but do not have sickle cell anemia.
If two people with the AS genotype have children, there is a chance the child could inherit:
However, if someone with AS has children with a person who has the AA genotype, their child can inherit either AA or AS with no risk of sickle cell anemia.
Eye color is a phenotype, a visible trait influenced by genetic factors.
GWAS have identified specific SNPs in various genes directly linked to differences in eye color among Europeans.
These findings confirm that eye color is a genetically complex trait shaped by multiple genetic variations rather than a single gene.
Females have an XX genotype, which means they inherit one X chromosome from each parent.
Mothers pass on one X chromosome, while fathers may pass on either an X or a Y chromosome, resulting in either a female(XX) or male(XY) genotype, respectively.
Unlike males, who inherit a Y chromosome from their father, females lack a Y chromosome, and their biological traits develop accordingly.
No, you cannot change your genotype since it remains constant throughout your life.
The only exception is rare cases of spontaneous mutations, which are unexpected changes in DNA that happen naturally.
However, environmental factors can influence how your traits appear, leading to variations in phenotype.
The Future Of Genetic Testing: Emerging Trends And Innovations

Genes vs. Lifestyle: Striking The Right Balance
Genetic Markers Explained
https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/phenotype
https://www.idtdna.com/pages/applications/genotyping
https://www.jbc.org/article/S0021-9258(25)00114-0/fulltext
https://pmc.ncbi.nlm.nih.gov/articles/PMC4530591
https://genomix.ng/category/genotype
https://www.sciencedirect.com/science/article/pii/S0960982209005971
https://www.genome.gov/27557513/the-y-chromosome-beyond-gender-determination
https://pmc.ncbi.nlm.nih.gov/articles/PMC3108095
That sharp, burning sensation shooting down your leg doesn’t just make it tough to get a good night’s sleep. Sciatica also makes sitting for long periods or walking more than a few steps feel difficult. Every day, moments like getting out of bed, enjoying a meal, or completing basic tasks can become a struggle. But what if there were ways to ease that discomfort without complicated treatments? Simple stretches, small posture changes, and lifestyle tweaks can help manage sciatica pain more effectively. We’ve put together some practical tips that target these pain points, allowing you to move through your day with less discomfort and sleep more soundly.
Sciatica is neuropathic pain triggered by compression, irritation, or pressure on the sciatic nerve.
This condition frequently results in inflammation and discomfort traveling along the nerve's path.
Since the sciatic nerve is the longest and thickest in the body, the pain usually starts in the lower back or buttocks and can travel down the leg to the feet and toes.
Sciatica usually affects only one side of the body, and the pain can often worsen with sudden movements such as bending or sneezing, or during prolonged periods of sitting.
Common symptoms of sciatica include:
Various spinal or muscular conditions can trigger the sciatic nerve.
Below are some common causes:
When you have sciatica, getting quality sleep isn’t always easy.
Discomfort from sciatica can interrupt your sleep, but small changes in posture and habits can make a big difference.
Here are 8 simple tips to help you get better sleep with sciatica:
This is one of the most recommended positions to minimize sciatic nerve pressure.
Lying on your back can be effective if you correctly support your lower back and knees.
Bending your body into the fetal position can help relieve pressure from the lower back, particularly if you have a herniated disc.
Prolonged periods spent on a firm surface, like the floor can aid in maintaining correct spinal alignment.
Adding support under your lower back can enhance spinal alignment.
Sleeping on your stomach is one of the least favorable positions for sciatica.
It can cause your spine to curve improperly, putting extra stress on muscles and joints.
This problem can worsen if your mattress is too soft and doesn't support your body properly.
Any position that causes your spine or hips to turn incorrectly should also be avoided, as it can irritate the sciatic nerve and increase pain.
Choosing positions that keep your spine straight and well-supported is best for better sleep and less discomfort.
Stretching before bed can reduce nerve pressure and relax tight muscles, making sleeping easier with sciatica.
Check out these simple stretches below:
It improves lower back flexibility and reduces pressure on the sciatic nerve.
It loosens tight hamstrings that can pull on the lower back.
Tip: Use a towel or band around your foot if you can't reach it comfortably.
It helps relax tight hip muscles pressing on the sciatic nerve.
It opens tight hips and eases pressure on the sciatic nerve.
It relaxes the glute muscles, which are closely connected to the sciatic nerve.
It stretches the front hip muscles that often tighten from sitting too long.
Important notes:
Doctors widely recommend sleeping on one's side during pregnancy, as it supports both maternal health and fetal development.
Sleeping on the left side is often recommended for better blood flow through the inferior vena cava, a vein that flows deoxygenated blood from the lower body to the heart.
A 2019 review confirms that both left and right-sided sleeping positions are safe for you and your baby.
If you're dealing with sciatica, the key is to sleep on the side opposite to the pain.
For extra comfort, you can try incorporating these helpful adjustments:
While stretching techniques are crucial for relief, several other methods can help ease sciatica pain and improve sleep quality, including:
Several factors contribute to sciatica pain intensifying at night:
Doing mild exercises, using heat therapy, and taking OTC anti-inflammatory medicine may help with sciatic nerve pain.
Staying active with gentle movement and avoiding prolonged sitting also provides relief.
For ongoing pain, physical therapy may be recommended.
A combination of strategies, such as hamstring stretches, low-impact activities like walking, hot or cold packs, and proper posture, can quickly heal sciatica.
Short rest periods help, but prolonged inactivity should be avoided to prevent worsening the condition.
For severe sciatica, quick relief may come from a position that reduces nerve pressure, like lying down with knees elevated, along with heat or cold therapy to ease discomfort.
Persistent or unbearable pain should be addressed promptly with a healthcare professional who might recommend targeted treatments like injections for faster relief.
It depends on what feels right for your body, as everyone’s experience with sciatica is different.
Some people find relief lying down, while others feel more comfortable sitting.
What matters most is not staying in one position for too long.
Staying in one position for extended durations can cause stiffness and worsen pain.
Try to move around gently, take short breaks, and find a position that helps you feel at ease.
Sciatica can often be mistaken for several conditions that cause leg pain.
Here are some conditions that mimic sciatica:
The key to distinguishing sciatica is its pain pattern, which travels downward from the lower back to one leg.
Best Sleeping Position For Lower Back Pain: What Research Says

The Stress-Back Pain Connection: How to Break the Cycle

The Top 3 Methods To Fall Asleep Faster
https://my.clevelandclinic.org/health/diseases/12792-sciatica
https://www.healthline.com/health/how-to-sleep-with-sciatica
https://www.nyspine.com/blog/sciatica-stretches-you-can-do-in-bed/
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(19)30054-9/fulltext
https://www.healthline.com/health/chronic-pain/treating-pain-with-heat-and-cold
https://www.ncbi.nlm.nih.gov/books/NBK542299
https://www.webmd.com/drugs/2/drug-5173-1289/naproxen-oral/naproxen-oral/details
https://www.webmd.com/sleep-disorders/benefits-of-cold-vs-hot-shower
https://health.clevelandclinic.org/is-your-leg-pain-sciatica-or-something-else
Did you know that 15%-20% of adults in the USA suffer from restless leg syndrome (RLS)? RLS causes an irresistible urge to move one's legs to relieve unpleasant or uncomfortable sensations. It's most severe at night, often exacerbated by insomnia or poor sleep. But is lack of sleep the only reason? Not really! RLS could be brought on by medications, lifestyle factors, and even some aspects of your diet. Let's learn more about foods that can cause RLS and others that may help manage the condition.
Your diet is a modifiable risk factor in the development of RLS.
A balanced diet with nutrient-laden fruits, vegetables, nuts, and seeds can promote good health and ease the symptoms of RLS.
On the other hand, regular intake of caffeine, alcohol, and sugary foods could trigger RLS or worsen existing symptoms.
The deficiency of specific nutrients like iron could also lead to RLS.
Different foods can trigger RLS symptoms in people.
Here are the Top 4 foods that may cause Restless Leg Syndrome!
Sugary foods are likely one of the most notorious diet elements behind RLS.
While no clinical evidence points to sugar consumption as a direct cause of RLS, here are some indirect ways sugar may contribute to RLS:
Conversely, studies show that eating a diet low in sugars causes fewer symptoms of RLS.
It's always best to avoid sugary foods like sodas, cookies, and other processed desserts.
Caffeine, a nervous system stimulant, is one of the major etiological factors of RLS.
It activates parts of the nervous system, increasing the contractility of voluntary muscles (found in the legs).
It may also cause insomnia (sleeping difficulty), which can further exacerbate RLS.
Tea and coffee are famously caffeine-rich beverages.
Some chocolate bars and snack bars may contain caffeine, too.
Alcohol consumption is known to cause sleep disturbances, which in the long run can cause RLS.
Studies have shown that people develop RLS during detoxification from alcohol.
Celiac disease may be associated with RLS due to its association with iron deficiency.
An immune reaction to gluten, found in grains like wheat, causes this chronic health condition.
For this reason, people with RLS are often screened for Celiac disease.
Researchers recommend cutting down on gluten to help manage RLS symptoms.
While a few foods are known to cause or aggravate restless leg syndrome, some foods are recommended to alleviate symptoms.
Let's examine the list of foods that you can include in your diet to reduce symptoms.
Lack of iron or its incorrect usage may result in the onset of RLS.
Several conditions that can cause iron deficiency include kidney failure, peripheral neuropathy, diabetes, Parkinson's, and rheumatoid arthritis.
Iron-rich foods to add to your diet include:
Folate and magnesium deficiencies may also contribute to RLS.
Both nutrients are required for muscle contraction and nerve impulse conduction.
Folate and magnesium-containing foods to include are:
| Folate-rich foods | Magnesium-rich foods |
| Spinach and dark leafy greens | Nuts like almonds, cashews, peanuts |
| Fortified cereals | Spinach |
| Black-eyed peas | Black-eyed peas |
| Lentils and beans | Soy milk |
| Asparagus | Brown rice |
| Brussels sprouts |
To prevent painful RLS flare-ups, avoid food triggers like caffeine, alcohol, sugary foods, milk, and gluten-containing foods.
All these foods have some links to RLS or RLS flare-ups.
If you have RLS, it's best to consult with a doctor before including or eliminating foods from your diet entirely.
Researchers worldwide suspect a deficiency of vitamins A, C, D, E, and folate to be a causative factor for restless leg syndrome.
However, no conclusive evidence proves that vitamins (in excess or deficiency) cause RLS.
If you are experiencing symptoms of RLS, your magnesium levels will likely be the first thing checked.
This is because RLS is a nervous system disorder, and magnesium deficiency can cause problems with nerve impulse conduction, muscle contractions, and cramps, resulting in RLS.
Research says that magnesium supplementation may relieve RLS symptoms as the mineral makes it easy for muscles to relax.
This may be due to magnesium’s calcium-blocking abilities, which help regulate nerves and muscles.
In addition to appropriate nutritional supplementation, other treatments for RLS include:
A doctor can best evaluate the underlying cause of your case of RLS and recommend the best course of action to eliminate it and ease your symptoms.
1 in every 5 pregnant women experiences RLS, especially in their third trimester.
This may be due to dopamine dysregulation, hormonal imbalance, and other nutritional deficiencies.
Consult your doctor if you are experiencing RLS-like symptoms while.
In people who are allergic to milk or are lactose intolerant, consuming milk may trigger RLS symptoms.
Consuming a substance that the body can’t tolerate leads to inflammation and histamine production, which could further aggravate RLS.
The exact cause of RLS is unknown.
Currently, researchers suspect it developed due to the way the brain cells use dopamine.
Excessive consumption of salt causes fluid retention in the body, which causes discomfort and affects sleep.
Poor sleep quality, in turn, may exacerbate RLS symptoms.
Restoring potassium levels through diet or supplementation may improve RLS symptoms.
However, the exact mechanism of how potassium alleviates symptoms of RLS is unknown.
Bananas are naturally rich in potassium and may help combat RLS symptoms.

Why Core Sleep Matters And How To Get More Of It

Can Lack Of Sleep Cause Nausea? Know How To Prevent It

Could Weight Loss Be The Most Effective Treatment For Sleep Apnea?