Preeclampsia is a pregnancy complication that affects two hundred thousand pregnant people in the U.S. per year. This worrying number has only been on during and post the COVID pandemic. While certain factors can increase the risk of this condition, research also suggests that family history plays a role here. This article discusses in-depth about preeclampsia, touching upon its risk factors and whether it has any genetic roots.
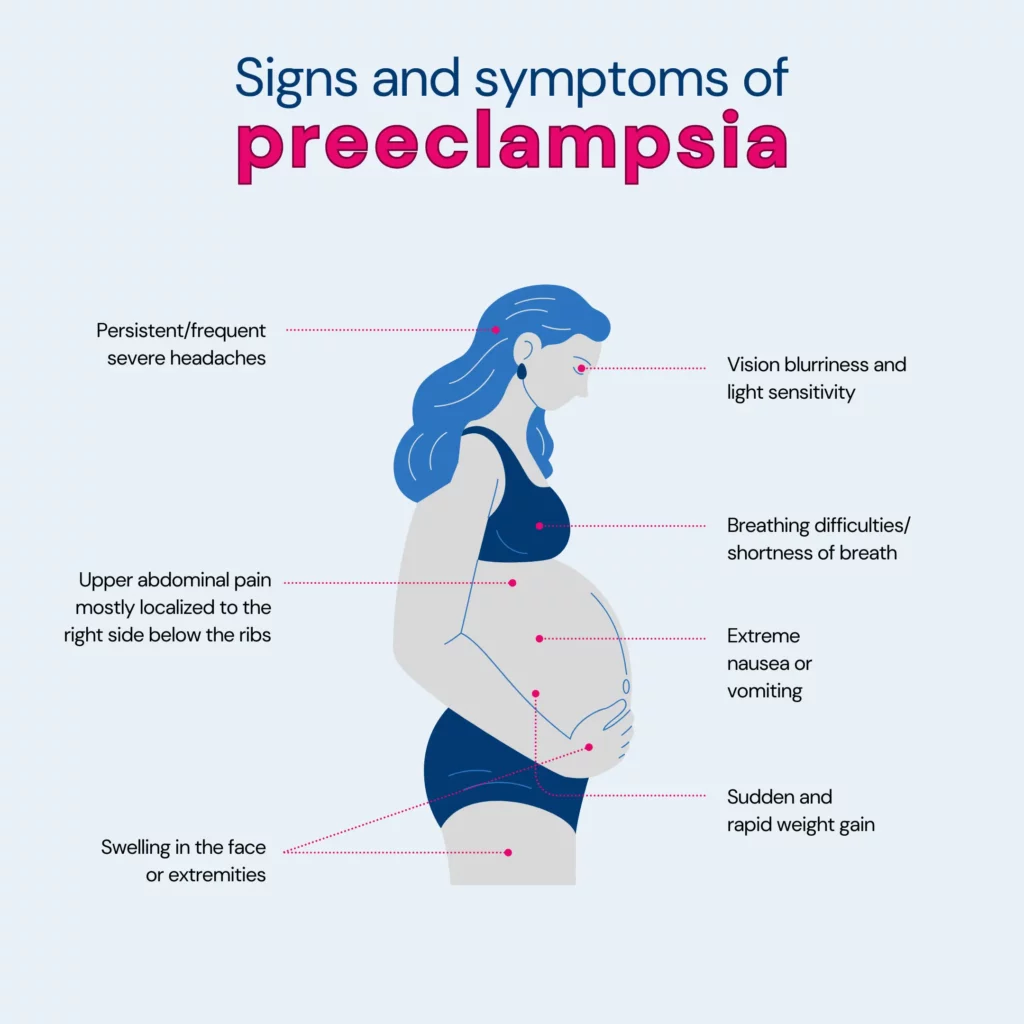
Preeclampsia is a serious condition that may arise during pregnancy, usually occurring after the 20th week.
It results in high blood pressure (hypertension) and is often linked with the presence of protein in the urine (proteinuria), suggesting potential kidney issues.
Preeclampsia can extend its impact to other organs, such as the liver, leading to additional symptoms.
Although it commonly resolves post-childbirth, neglecting treatment can pose significant health risks for both the baby and the mother.
Preeclampsia is usually seen in first pregnancies, but if there is a history of it in the previous pregnancy/ies, then the risk of preeclampsia in future pregnancies is seven times higher!
While it can affect anyone who is pregnant, certain factors increase the risk. Let's take a closer look at them:
Remember, individual risk varies depending on the combination of factors present in each person.
Regular checkups with your healthcare provider throughout the pregnancy are vital steps, ensuring your and your baby's well-being.
Yes, there is substantial evidence suggesting a genetic component in the development of preeclampsia.
Scientists did an extensive study, checking 775 tiny genetic variations in 120 genes of over 350 moms with preeclampsia and 602 without it.
They identified six genes (IGF1, IL4R, IGF2R, GNB3, CSF1, and THBS4) that contribute to preeclampsia development through a combination of maternal and fetal genetic changes.
Yes, there is a familial link to preeclampsia, indicating a genetic influence on the condition, such as:
Yes, if your mom had preeclampsia during her pregnancy, there is an increased risk that you may also develop preeclampsia during your pregnancy.
A cohort study involving 22,768 elder daughters and 2,959 younger daughters revealed a link between a mother's preeclampsia and her daughters' vulnerability to it.
Mothers having preeclampsia during the first pregnancy with an elder daughter increase the elder daughter's risk of developing it in her own first pregnancy by 1.7 times. This risk continues into the second pregnancy.
The study found similarly elevated risks for daughters if the mother had preeclampsia in any other pregnancy or if only mothers with firstborn children were considered.
However, it's important to note that genetic predisposition explained only a minor part of preeclampsia occurrence in the population studied.
Preventing genetic preeclampsia isn't guaranteed because it depends on factors beyond your control. However, there are steps you can take to reduce the risk or manage it:
The best-known method is low-dose aspirin, typically an 81-milligram tablet daily after 12 weeks of pregnancy.
Your primary care provider may recommend this if you have one high-risk factor for preeclampsia or more than one moderate-risk factor.
Being as healthy as possible before pregnancy is advised, especially if you've had preeclampsia before.
Manage any conditions that increase the risk of preeclampsia by discussing them with your healthcare provider.
Note: Before taking any medications, vitamins, or supplements, it's crucial to consult your provider to ensure safety.
Preeclampsia can bring about various health challenges, including:
Understanding these potential impacts is crucial, and early detection and management are essential for the well-being of both the mother and the baby.
Additional factors that might slightly raise the likelihood of developing preeclampsia include:
Preeclampsia is a serious condition during pregnancy with high blood pressure and protein in urine.
It's more likely in first pregnancies, especially if there's a family history or if it happened before.
Genetics is a factor, but it doesn't explain everything. If your mother had it, you're at a higher risk.
Taking low-dose aspirin as prescribed by your doctor and adopting a healthy lifestyle can help lower your risk.
Preeclampsia can cause problems for both mom and baby, so early detection and care are essential.
Age, obesity, and certain conditions can also affect the risk. Regular checkups and healthy choices make a big difference in having a safer pregnancy.
https://www.nhs.uk/conditions/pre-eclampsia/
https://www.news-medical.net/health/The-Genetics-of-Pre-Eclampsia.aspx
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4060423/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3145161/
https://pubmed.ncbi.nlm.nih.gov/10468424/
https://www.mayoclinic.org/diseases-conditions/preeclampsia/symptoms-causes/syc-20355745
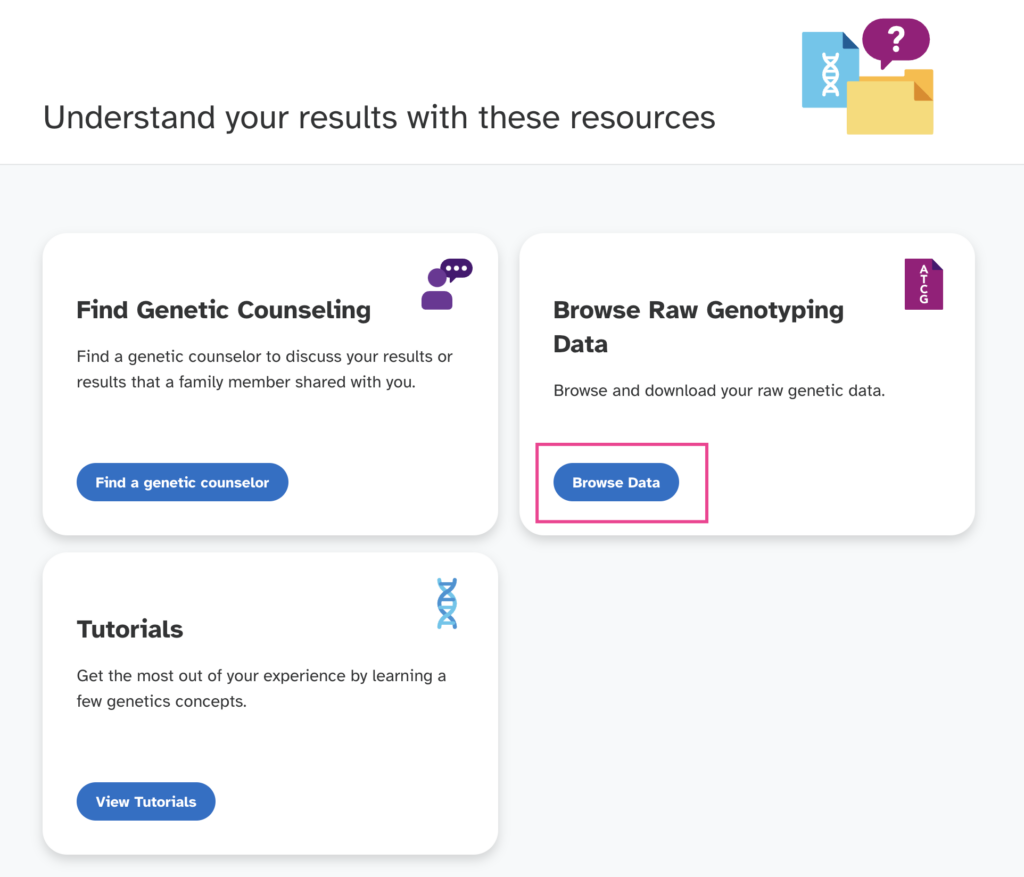
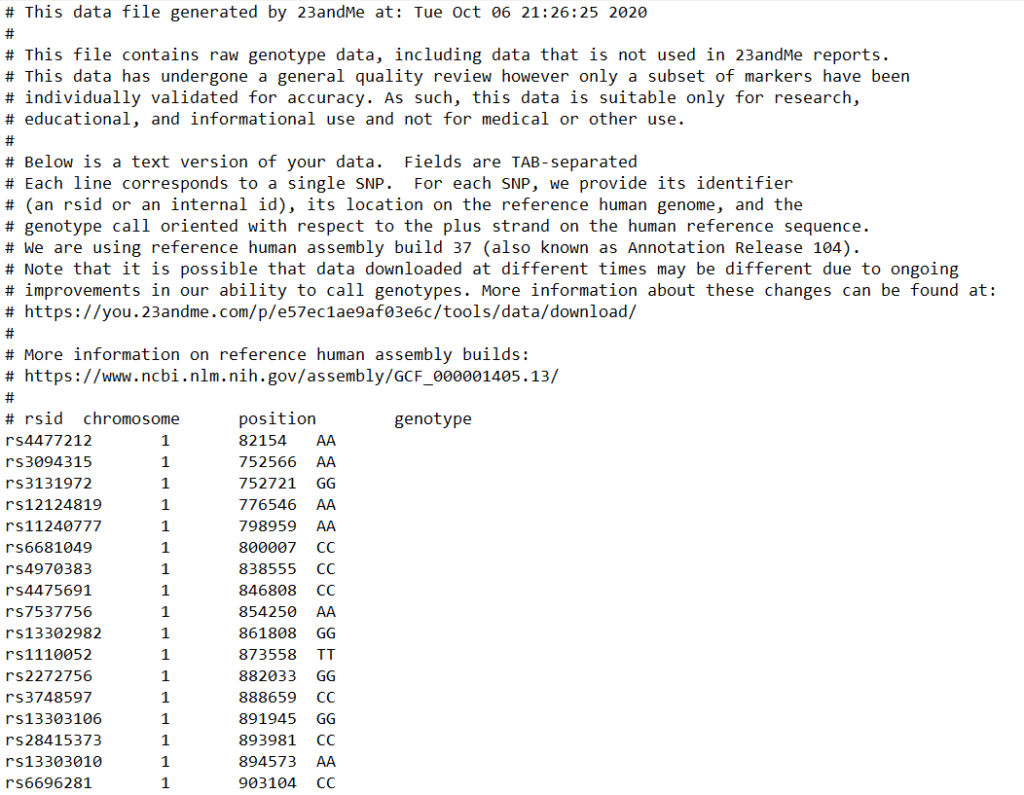
One of the most important parts of your 23andMe results is the DNA raw data, which contains information on more than 700,000 genetic markers. While only a fraction of these markers are utilized to trace your lineage, the remaining data holds invaluable insights into your health and wellness, including potential risks for certain diseases. Unlocking this wealth of information is straightforward. By following seven simple steps, you can swiftly download your DNA raw data file in under a minute. Xcode Life can then analyze this data to provide ten comprehensive reports, offering you a deeper understanding of your health.
Video explainer: How to download 23andMe DNA raw data.
Sign in to your 23andMe account from the 23andMe website
Click on the down arrow near your name from the top navigation bar
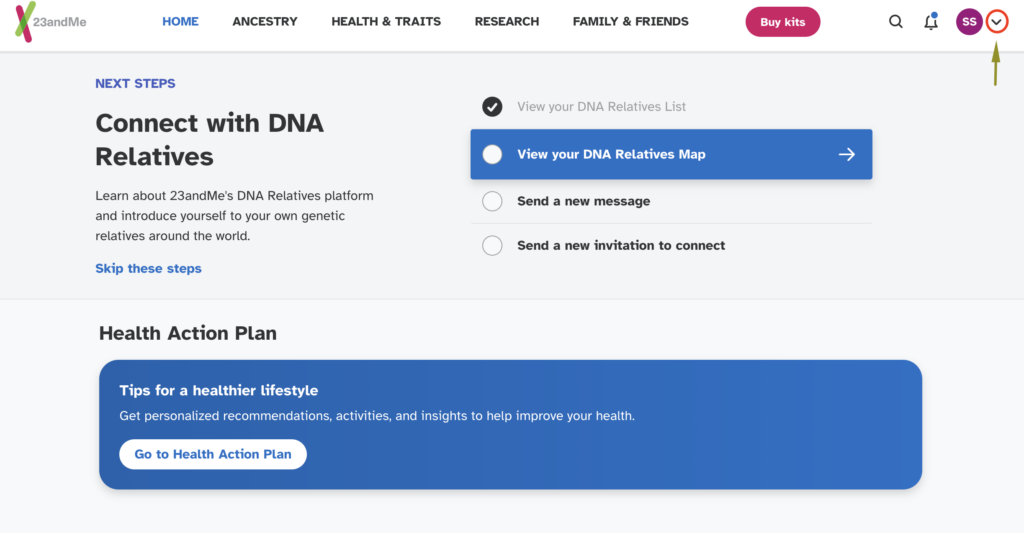
Select "Resources" as shown below
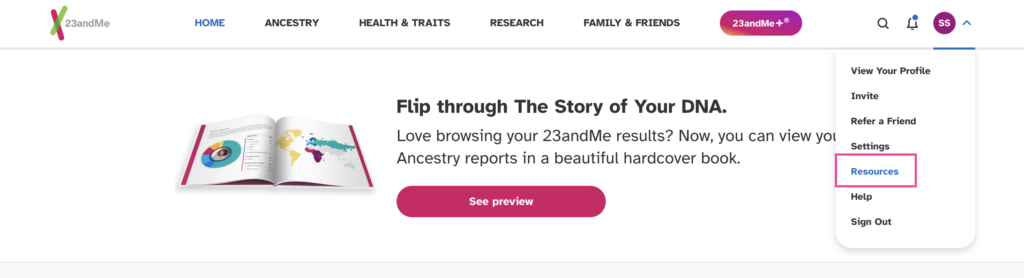
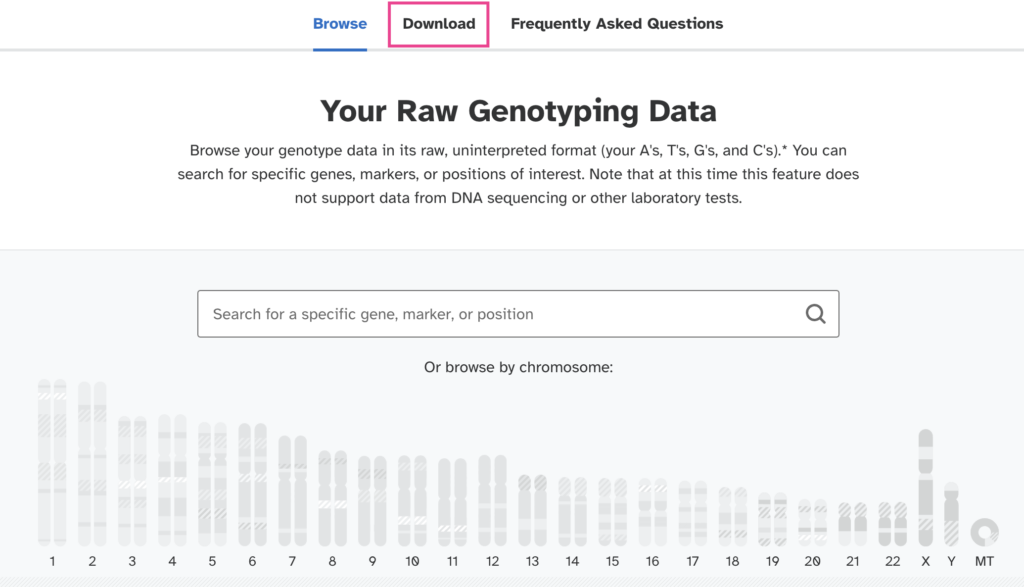
Click on the 'Browse Data' button
Select the "Download" option from the next page.
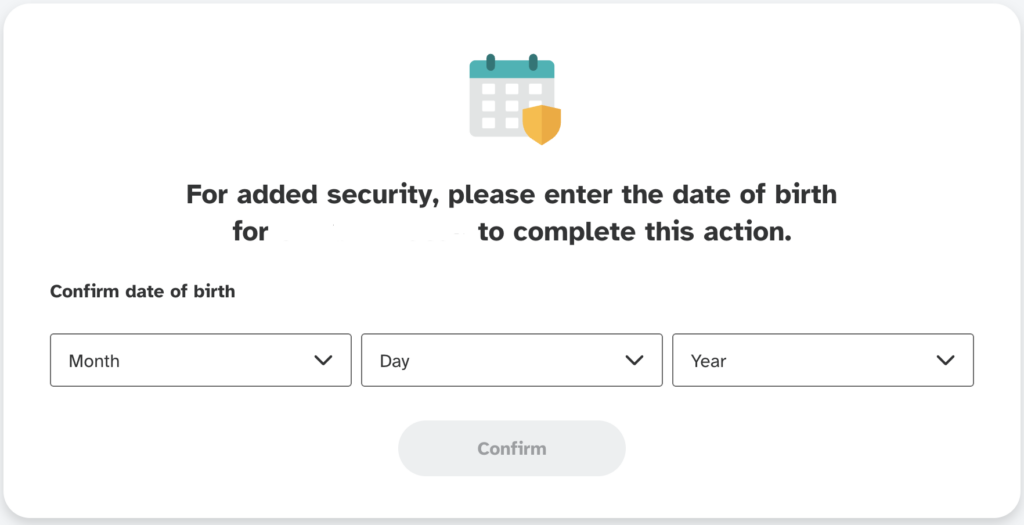
Enter the same date of birth you had given when registering your account.
On the next page scroll down to the bottom of the download page until you see the "Submit request" button.
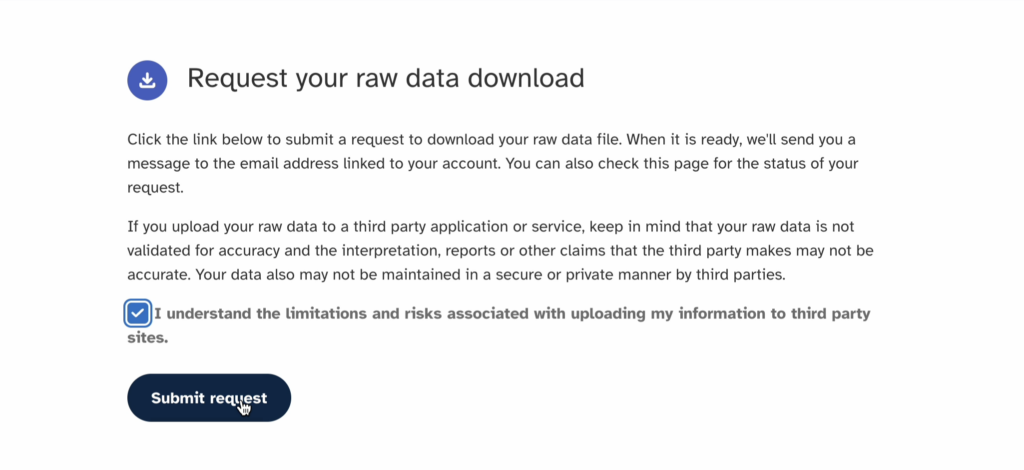
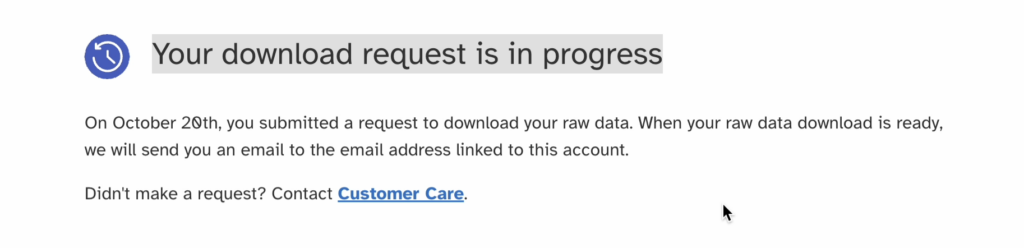
23andMe will send you an email notification once your raw data is ready, or you can just refresh your download page. This may take 2-4 days.
OR, you can directly access the download page here
Also see, Free tools for 23andMe, AncestryDNA, FTDNA raw data analysis
Final notes:
Your DNA raw data is a file of size 5-7 MB in the .zip format or 16-21 MB in the .txt format.
Most of us are not strangers to the occasional scratchy, sore throat, an ailment that often heralds the onset of a common cold or a change in the weather. However, at times, what begins as a minor discomfort in the throat can evolve into symptoms that are more persistent and troubling. While many conditions could cause persistent sore throat, two common ones are tonsil stones and strep throat. Despite their distinct natures, both conditions share similar symptoms, like a sore throat, leading to a common dilemma in self-diagnosis. In this article, we aim to clearly differentiate between tonsil stones vs strep throat. We will explore the unique characteristics, causes, symptoms, and treatment methods for each condition.
About Xcode Life
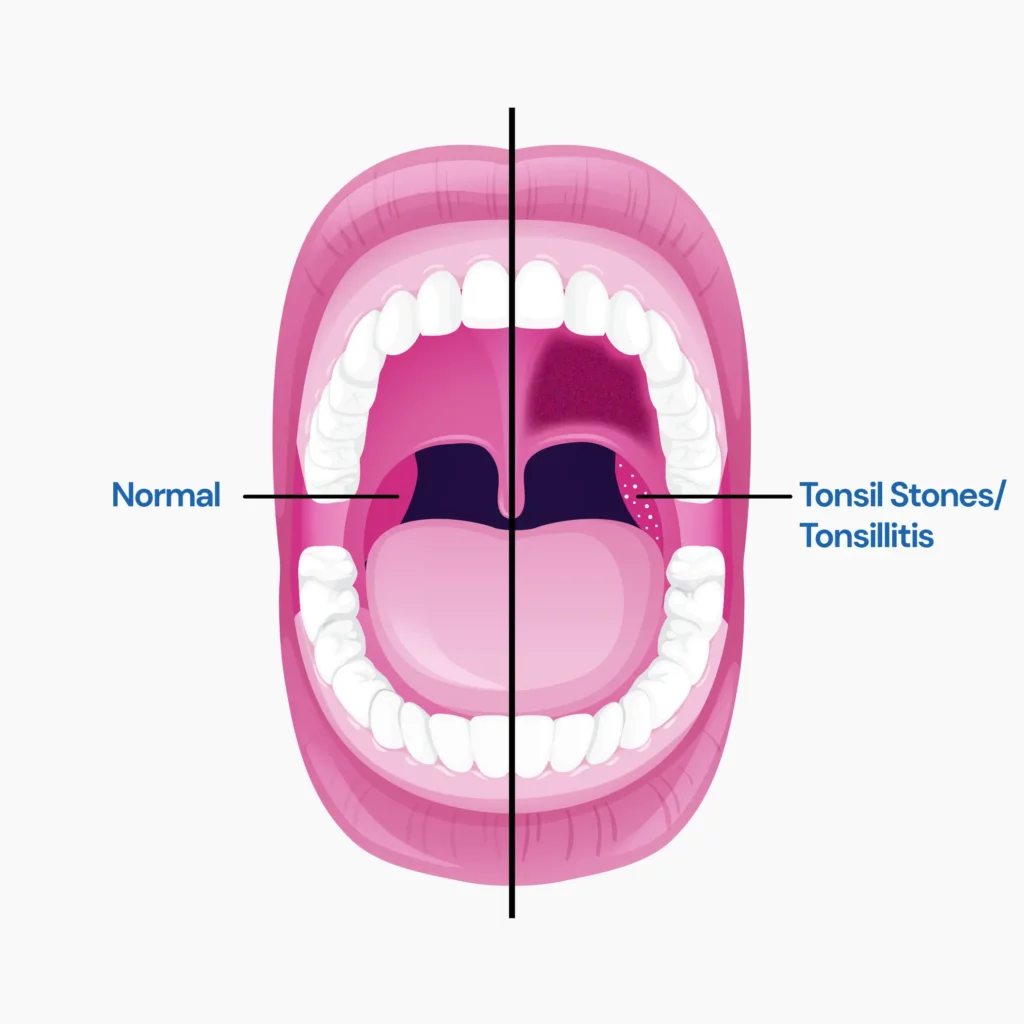
Tonsils are two round, fleshy masses at the back of your throat.
They are lymph nodes that filter germs that enter the nose and mouth.
Tonsil stones are small white-colored pebble-like stones that form in the tonsils.
They are composed of minerals like calcium, food debris, and germs
Symptoms of tonsil stones and Strep throat infection can be very similar.
Most people may experience the following symptoms:
Tonsil stones are formed when food debris gets stuck in the folds of the tonsils.
These folds are usually small, but when debris is trapped, it enlarges them.
This results in minerals like calcium getting deposited and hardening into stones.
Strep throat is a contagious condition caused by a bacterial infection in the throat and tonsils. Strep throat is more common in children but affects people of all ages.
Common symptoms of strep throat are:
Some people may also experience nausea, vomiting, fatigue, and body aches.
Group A Streptococcus bacteria cause strep throat.
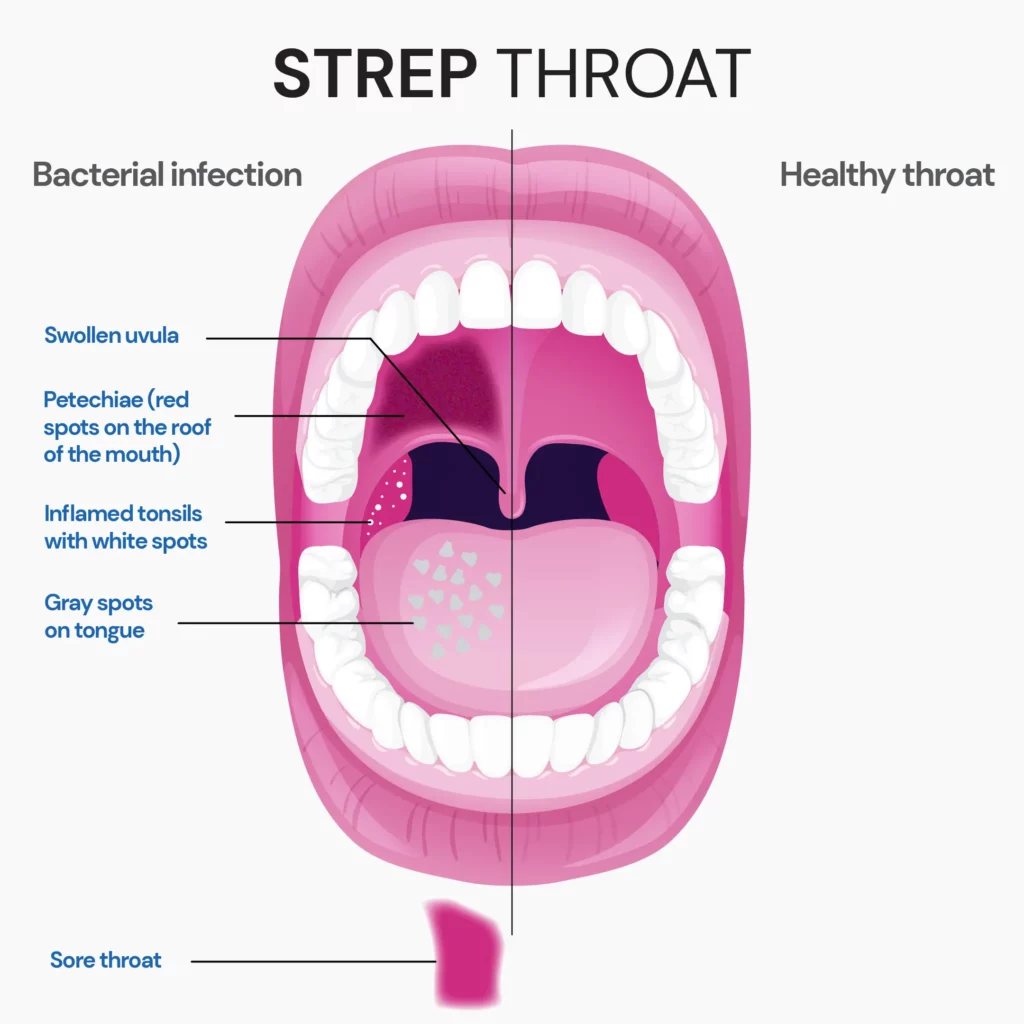
Since tonsil stones and Strep throat show similar symptoms, it is often difficult to tell one from the other.
But, here’s how their symptoms are different, making diagnosis easy:
| Symptom | Tonsil stones | Strep throat |
| Runny nose | Absent | Present |
| Sore throat | Present | Present but has a sudden onset |
| Bad breath | Present | Absent |
| Cough | Present | May not be present |
| Postnasal drip | Present | Absent |
| Stiff neck | Present | Absent |
| State of tonsil | White or yellow small stones on tonsils | Swollen or red tonsil with streaks of white pus |
| Nausea and vomiting | Absent | Present |
Recurring strep infection or tonsilitis can increase the risk of tonsil stones; but tonsil stones need not always mean that there's an underlying strep infection.
No, not always. The white streaks or spots in strep are usually pus formations due to the infection, unlike the white ones in tonsil stones, which are hardened and calcified stones.
Your doctor will perform a physical examination and check your nose, throat, and ear for signs of infection.
If your doctor suspects strep throat, they will collect a swab from the back of your throat.
If you test negative for Streptococcus bacteria, a throat culture is performed to determine the causative organism of your tonsil stones.
The treatment for tonsil stones and strep throat varies.
In many cases, tonsil stones are treated at home. Some common home remedies include:
*do not try these at home before consulting a qualified practitioner.
Medications
Your doctor may prescribe antibiotics if required. Some OTC painkillers may also be helpful.**
**do not try these at home before consulting a qualified practitioner.
Surgery
If tonsil stones keep recurring, your doctor may recommend tonsillectomy (a surgery to remove tonsils).
Treating Strep throat usually involves a prescription of antibiotics.
Usually, amoxicillin or penicillin is prescribed to treat strep throat.
A single benzathine penicillin G shot is also used to treat strep throat.
Other antibiotics like erythromycin or cephalosporins like cephalexin may be prescribed to those who are allergic to penicillin.
It is important to treat strep throat at the earliest to prevent complications, which include:
Home remedies like gargling with salt water, getting plenty of rest, drinking warm fluids, and lozenges can help relieve sore throat associated with tonsil stones and strep throat.
Tonsil stones and Strep throat are contagious and can spread quickly.
You can prevent both conditions by practicing good hygiene, such as:
Alex, a seasoned construction worker, spends his days lifting and moving heavy materials. However, on a particularly strenuous day, while carrying a hefty piece of surveying equipment, Alex felt an unusual and disconcerting "popping" sensation in his lower abdomen. Concerned, he sought medical advice, and his fears were confirmed: Alex had developed a hernia. This diagnosis stirred a deeper anxiety within him. He recalled a pattern in his family—his father, uncle, and grandfather had all suffered from hernias. This familial recurrence led Alex to ponder a crucial question: Are hernias genetic? More importantly, Alex grappled with the concern that he might pass on the “hernia genes” to his own children.
In this article, we delve into the intricate relationship between hernias and genetics. We also aim to answer the pressing questions that linger in the minds of those who, like Alex, find themselves caught in a web of familial medical history.
About Xcode Life
A hernia is a condition that occurs when organs or fatty tissue protrude through fragile areas in the surrounding muscle or fascia, similar to a bubble in a balloon.
These weak spots are common in areas like the abdomen or groin, and several factors can lead to their development.
Not all hernias are the same. These bulges of organs happen in different places and have unique causes. Let's take a clear look at some common types of hernias:
Hernias happen when muscles get weak or strained. This can happen quickly or slowly.
Common causes:
No, there is no single root cause for hernias. Their development is often a multifactorial process, meaning multiple factors contribute to their formation, with the two main contributors being:
Based on the reviewed studies, evidence suggests that groin hernias have a genetic component.
The research, which analyzed family histories and inheritance patterns, found that having a family history of inguinal hernia notably raises the risk of developing a primary hernia.
The studies also indicated a tendency for increased hernia recurrence rates and earlier recurrence when there is a family history of inguinal hernia.
The current evidence focuses on groin hernias, but other types, like umbilical or hiatal hernias, might have different genetic influences.
More research is needed to understand the potential genetic link in other hernia types.
According to a recent systematic review, the inheritance of groin hernias appears to have a notable familial component. However, there’s no clear inheritance pattern for hernias.
Studies on twins in children didn't always confirm a clear genetic link. Still, research on family histories and reliable databases revealed a higher risk of inguinal hernias in children with a family history.
Notably, there's a significant connection between mothers and daughters and between sisters, suggesting that the tendency to inherit hernias is stronger among females.
In adults, people with inguinal hernias were more likely to have a family history of the condition compared to those without hernias.
A nationwide study pointed out that the risk of getting surgery for an inguinal hernia was highest when a sister had already undergone the same surgery compared to a brother.
Also, having a sibling who had hernia surgery increased the chances of needing surgery for a femoral hernia.
However, the research indicates that having a family history is a significant factor in developing inguinal hernias, with a stronger inheritance pattern among females.
Congenital diaphragmatic hernia (CDH) is an unusual condition that occurs in babies before birth.
It happens when the diaphragm, the muscle separating the chest and abdomen, doesn't close properly, creating a hole known as a hernia.
This opening allows abdominal organs like the intestines, stomach, and liver to move into the chest, affecting normal development.
The presence of intestines in the chest can lead to complications like malrotation, where the typical connections holding the intestines in place are disrupted.
This may cause twisting and cutting off of the blood supply (volvulus).
Additionally, the affected side's lung is smaller, and the development of both lungs is impacted.
The air sacs inside the lungs may not form correctly, leading to blood flow issues and increased pressure in lung blood vessels.
This higher pressure makes breathing challenging for the baby after birth, and some infants may also experience heart development problems.
Treatment for CDH depends on factors like when the condition is discovered, its severity, and whether there are associated heart issues.
While hernias are often associated with increased physical strain or pressure, a subset can have a genetic component.
These "genetic hernias" are caused by mutations in specific genes that affect the proteins responsible for building and maintaining strong connective tissues, particularly collagen.
Beyond genes: Additional risk factors
Hernias are usually fixed through surgery, especially if they're big or causing a lot of trouble. Here's what can be done:
Diagnosing and checking hernias:
Note: Remember, it's crucial to consult your doctor for personalized advice, whether considering surgery, using a supportive belt, or undergoing diagnostic tests.
Hernias, when organs bulge through weak spots in muscles, might have a family link, especially for groin hernias.
If someone in your family had it, you might be at a higher risk. This connection is stronger among females.
While groin hernias seem connected to genes, we're still figuring out if other types, like belly button or upper stomach hernias, have the same link.
Some gene mutations and family history can make you more prone to hernias.
Treatment involves surgery, lifestyle changes, and sometimes using a supportive belt.
Regular check-ups and tests help keep an eye on things. Remember, talking to your doctor about your situation is crucial.
https://www.webmd.com/digestive-disorders/understanding-hernia-basics
https://my.clevelandclinic.org/health/diseases/15757-hernia
https://www.healthline.com/health/hernia
https://www.cdc.gov/copd/index.html
https://www.medicalnewstoday.com/articles/142334
https://pubmed.ncbi.nlm.nih.gov/23423330/
https://pubmed.ncbi.nlm.nih.gov/36443569/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6061067/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4131122/
If there’s any food that can break the myth that plant sources don’t provide enough protein, it is definitely pumpkin seeds! They are also a great testament to the saying, “Good things come in small packages.” A small amount of pumpkin seeds eaten every day can enrich your body with magnesium, potassium, calcium, and zinc. Pumpkin seed powder is made by roasting pumpkin seeds, which increases its antioxidants due to heat exposure. It’s also touted to be one of the best plant protein alternatives for those who avoid animal or dairy-based proteins.
Did You Know?
Protein is one of the most important macronutrients for weight loss. It not only supports muscle mass building but also keeps you fuller for longer resulting in lesser calorie intake. However, not everyone may experience the same kind of weight loss with protein intake, with one of the most significant reasons being genetic makeup. Some genes interact with protein to influence its effect on the body.
At Xcode Life, you can upload your existing DNA raw data from ancestry genetic tests to understand how your body interacts with nutrients so that you can modify your diet to achieve your nutritional goals. Learn more.
As the name suggests, pumpkin seed powder is obtained by grinding raw or roasted pumpkin seeds.
It has been found that pumpkin seed powder prepared from roasted pumpkin seeds has greater health benefits as roasting them increases the antioxidant content.
Roasting pumpkin seeds also improves their flavor and taste.
However, roasted pumpkin seeds may result in the loss of micronutrients.
Regardless of how you consume pumpkin seed powder, it is an excellent source of plant protein for vegetarians and vegans.
Pumpkin seed powder is prepared from 100% pure roasted or raw ground pumpkin seeds.
Pumpkin protein powder, on the contrary, contains pumpkin seed powder along with other plant proteins obtained from flaxseeds or quinoa. Therefore it is pumpkin flavored but does not contain 100% of pumpkin powder.
Always check the ingredient list to know if you are consuming pure pumpkin powder.
Sometimes, pumpkin protein powders contain whey or casein as the main protein source with pumpkin flavor.
Pumpkin seed powder and pumpkin seed protein are often the same product, provided the ingredient in both of them is pumpkin seeds.
One ounce of 28 g of pumpkin seed powder can give you 18 g of protein. Other nutrients you get from it are:
| Nutrient | Value |
| Calories | 80 |
| Carbohydrates | 1 g |
| Fat | 0 g |
| Sugar | 0 g |
| Calcium | 33 mg |
| Iron | 6 mg |
| Potassium | 462 mg |
| Zinc | 7 mg |
| Magnesium | 319 mg |
It also contains antioxidants like flavonoids and phenolic acid, and small amounts of vitamin E and carotenoids.
There is ongoing research about the benefits of pumpkin seed protein.
Some of these include:
Researchers have found that pumpkin seed extract has anti-cancer effects on several cancers, including prostate, breast, lung, liver, and colon.
This is attributed to the antioxidant properties of various phytochemicals present in it.
Pumpkin seeds contain oils that have been found to improve urinary symptoms.
Some studies show that pumpkin seed extract improves prostate health.
However, more studies are required to prove this conclusively.
Many studies have stated that eating pumpkin seeds may help prevent depression. This is attributed to the amino acid tryptophan present in them.
Tryptophan is the precursor of serotonin.
Serotonin is the ‘feel good hormone’ and may have anti-depressant effects.
Several animal studies have found that pumpkin seed powder and extract have improved blood sugar levels.
This has been attributed to the protein, fiber, and fat content in the pumpkin powder.
Pea protein and pumpkin seed protein are both protein-rich.
The question of ‘which is better’ depends upon your needs.
Pea protein is rich in proteins, whereas pumpkin seed powder is rich in fiber.
Pumpkin seed protein is also rich in iron.
Pea protein and pumpkin seed powder have similar amino acid profiles, helping build muscle mass.
Pumpkin seed powder is versatile and can be used in multiple ways.
The American Heart Association (AHA) recommends you consume a quarter cup of pumpkin seeds (30 g) daily as part of a healthy diet.
This comprises protein, healthy fats, fiber, zinc, selenium, and magnesium.
While you can eat up to 30 g of pumpkin seeds daily as part of a healthy diet, it is always best to consult your dietician to determine the right quantity for you.
Pumpkin seed protein contains all nine essential amino acids, similar to pea protein.
However, it is low in threonine and lysine, making it an incomplete protein.
Side effects due to pumpkin and pumpkin seed powder are rare.
However, some side effects may include:
Pumpkin seed powder can be added to a variety of recipes.
Here are a few ways to do so:
Losing weight is a personal choice. It might be either because of serious health concerns or because one wants to look and feel good about themselves. Social media pages are full of fad diets and supplements that claim to reduce your weight miraculously. Some people claim that taking DHEA supplements has helped them reduce weight.
But is this true?
Are there any side effects of taking DHEA supplements? Read on to find out.
Your adrenal glands located in your kidney produce a hormone called DHEA (dehydroepiandrosterone).
Scientists are not entirely sure what role DHEA plays in the body, but this hormone is a precursor to male and female sex hormones.
DHEA supplements are made from wild yam or soy.
Proponents claim that this supplement:
This supplement can be availed without a prescription.
DHEA is known to block an enzyme named glucose-6-phosphate dehydrogenase, which is essential for fat synthesis.
DHEA can also inactivate some enzymes related to fat synthesis.
Over time, this means that more fat is burned than produced.
A study was conducted on older men and women to find if DHEA reduced abdominal fat.
The subjects were divided into two groups.
One group was given DHEA supplements for six months, while the other did not.
After six months, the group that received DHEA showed a significant reduction in abdominal fat.
But the results of this study do not automatically mean that you should buy DHEA supplements over the counter.
Insulin is a metabolic hormone that plays a crucial role in the body.
Insulin regulates blood glucose levels in the body.
The same study also showed that DHEA supplements could make people more sensitive to insulin and reduce resistance.
Understanding how genes interact with nutrition is crucial for healthy and long-lasting weight loss.
Each person's genetic makeup is unique, and how our body responds to different nutrients in our diet can vary based on this genetic composition.
Expanding on the genetic response to specific nutrients and its influence on weight loss:
The interaction between genetics and dietary fats, particularly saturated fats, is a prime example of how our genetic makeup can influence weight management.
Saturated fats are found in foods like red meat, dairy products, and certain oils. The APOA2 gene is particularly noteworthy in this context. It plays a role in the body's handling of these fats.
People with specific variants of the APOA2 gene have been found to be more sensitive to saturated fats.
For these individuals, consuming a diet high in saturated fats can lead to a greater propensity for weight gain and accumulation of body fat, compared to those without this variant.
Essentially, their bodies respond to saturated fats in a way that promotes fat storage more than fat burning.
Another example of how genetics can influence the body's response to specific nutrients, thereby affecting weight loss, involves the gene AMY1, which is responsible for the production of salivary amylase.
This enzyme is crucial for the breakdown of starches in our diet.
Individuals with more copies of the AMY1 gene produce more salivary amylase and are generally better equipped to break down starches efficiently.
On the other hand, those with fewer copies may find it harder to process these carbohydrates. This difference can significantly impact weight management.
For someone with fewer AMY1 copies, a diet high in starchy foods like bread, pasta, and potatoes might lead to more pronounced weight gain compared to someone with more copies of this gene.
Understanding these genetic predispositions allows for a more nuanced approach to nutrition and diet planning.
It's not just about the type of food consumed, but also how an individual's body processes these foods based on their genetic makeup.
This knowledge paves the way for personalized nutrition, offering tailored dietary recommendations that align with each person's unique genetic profile.
Some proponents of DHEA supplements claim that they can reduce cervical cancer and heart disease risk.
It can also reportedly treat sexual dysfunction.
However, these claims are yet to be proven.
DHEA is a hormone whose secretion reduces with age.
Therefore, many scientists speculate that supplementing your body’s reduced DHEA levels can slow aging.
Some studies have shown that it has some effect on aging, while others have reported no effect.
There are also other health concerns to long-term DHEA usage.
DHEA has shown some promise in reducing mild depression in middle-aged and older adults.
The National Institute of Mental Health conducted a study that showed a reduction in mild to moderate depression in the elderly.
However, more research is required to back this claim.
Some scientists even claim that DHEA supplements can treat Alzheimer’s disease, Schizophrenia, and infertility.
However, there is little evidence to support this claim.
DHEA and weight loss might be linked.
Some preliminary research has shown that DHEA does help in weight loss.
However, taking it might result in side effects.
Moreover, a proper diet and regular exercise are much more holistic approaches toward weight loss than consuming supplements.
If you still want to check it out, consult your doctor before buying it over the counter.
DHEA is a hormone that is produced by your adrenal glands.
It is a precursor to male and female sex hormones.
This hormone decreases in the body with age.
Some people claim that DHEA supplements can contribute to weight loss and strengthen the immune system.
However, scientists still need to learn about the benefits of DHEA supplements, although some research shows that it is beneficial.
DHEA supplements might only be for some, as they may have side effects.
It is always advisable to consult your doctor before starting any supplements.