Have you ever considered that the power of your breakfast might not just lie in the nutrients it offers but also in the precise clock hour you consume it? We live in a world where every bite can be an informed choice driven by the latest in nutritional science. In recent years, researchers have become increasingly interested in investigating the relationship between breakfast timing and diabetes risk. So, today, we won't just discuss what you should eat for breakfast but will delve into how breakfast timing might just be the hidden secret to supercharging your health goals.
Did You Know? Your ancestry test DNA data includes 700,000 markers, which can be used to learn everything about your nutritional profile and eating behavior. The video below outlines one such example where genes control your tendency to snack frequently. Want to learn about your personalized nutritional insights without repeating your DNA test? Learn more.
The link between meal timings and health is closely tied to our body's natural circadian rhythm.
This rhythm acts like an internal clock regulating our sleep-wake patterns over 24 hours.
It affects how tired or awake we feel and influences other essential processes, including eating and digestion.
Irregular meal patterns caused by working night shifts or traveling across time zones can disrupt our body's natural rhythm and adversely affect our health.
Studies have shown that night shift workers consume more calories during their night hours and have poorer diet quality.
Therefore, it can increase the risk of metabolic conditions like insulin resistance, obesity, and diabetes.
To maintain better health outcomes, paying attention to when we eat and aligning our meals with our body's natural rhythm is essential.
Research published in The Journal of Nutrition in 2019 indicates a connection between skipping breakfast and an increased risk of type 2 diabetes.
A systematic review and meta-analysis evaluated this connection while considering body mass index (BMI).
The analysis included 6 separate studies with 96,175 participants and 4935 cases of type 2 diabetes.
Without adjusting BMI, participants who regularly skipped breakfast had 33% higher chances of developing the risk of type 2 diabetes than those who did not.
Even after adjusting it, the connection remained significant. Breakfast skippers faced a considerable 22% higher risk.
Additionally, the researchers conducted a dose-response analysis, demonstrating each additional day of skipping breakfast.
When breakfast was skipped 4 to 5 days a week, type 2 diabetes risk spiked by an alarming 55%.
The Only Checklist You Need For Lifelong Good Health
The most recent study published in the International Journal of Epidemiology examined the possible effect of breakfast timing on type 2 diabetes.
103,312 adults from the NutriNet-Santé cohort were enrolled to provide valuable dietary habits and overall health data.
A significant majority (79%) were women.
The mean age of the cohort was 42 years.
Over 2 years, researchers meticulously tracked the participants' eating patterns, recording the breakfast timing and the frequency of meals throughout the day.
Subsequently, they observed the participants for an average of 7.3 years, keenly noting the chances of rising type 2 diabetes.
Throughout the study, the researchers recorded 963 fresh cases of type 2 diabetes.
Individuals who consistently had their first meal after 9 AM faced a 59% higher risk of developing type 2 diabetes than those who enjoyed breakfast early before 8 AM.
However, the study yielded a favorable outcome for individuals who frequently ate throughout the day - they had a lower risk for type 2 diabetes.
Furthermore, researchers found no significant correlation between overnight fasting and type 2 diabetes, except for those who ate breakfast before 8 AM and fasted over 13 hours at night.
While the study provided valuable insights, it did encounter certain limitations.
One potential concern lies in the reliance on self-reported dietary records by participants, which may only sometimes be entirely accurate.
Additionally, other unexplored factors might increase the risk of type 2 diabetes, which were not within the scope of this study.
To address the limitations, they should investigate whether similar results appear across diverse populations in the future.
Recent research has revealed the benefits of having breakfast before 8 AM.
Those who opt for an early morning meal enjoy a remarkable 59% reduction in their risk of developing diabetes.
If you're a late breakfast eater, consider shifting your mealtime earlier to reap these potential health rewards.
Note: If you have any medical conditions, it's crucial to seek your doctor's advice before making any significant changes to your diet.
The Gene Nutrition panel of Xcode Life includes 48 important nutrition aspects, covering everything from ideal macro breakup and eating patterns to vitamin needs and food intolerances.
If you have done an ancestry genetic test with companies like 23andMe, AncestryDNA, MyHeritage, etc., you can learn your nutritional gene status in just 3 steps.
Not yet tested?
If you're new to the world of genetic testing, we've got you covered!
You can now get your ancestry DNA kits at an additional discount!
By following the link provided in this article, you can purchase a DNA kit at 10% OFF (the discount will be reflected when you add the product).
This will ensure that you have everything you need to embark on your genetic journey.
Once you receive your kits, you can follow the instructions given by the respective service providers to collect your sample and ship it.
After you receive your DNA test results from the kit, you can upload your DNA data to our secure platform.
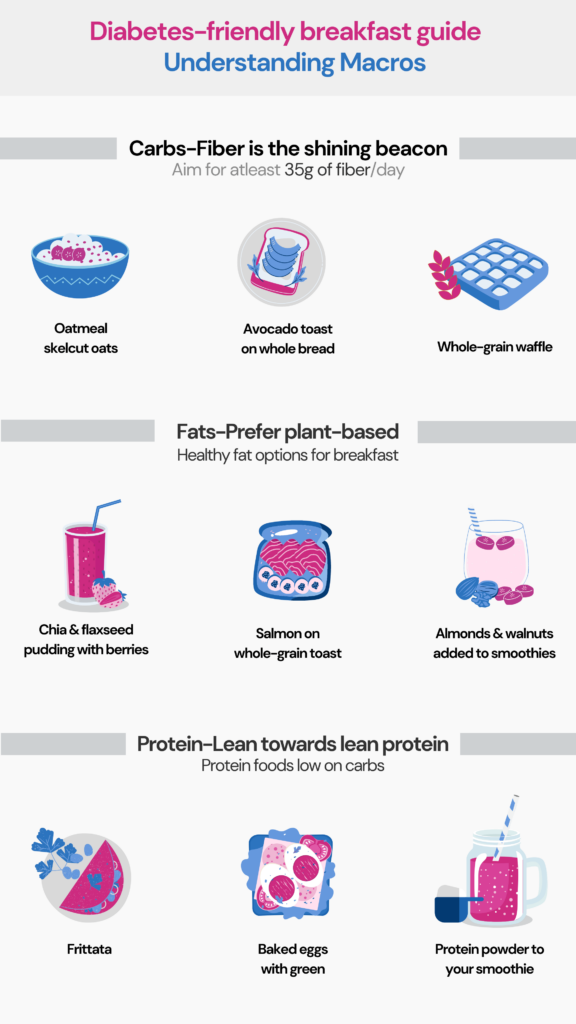
While early breakfast timing has demonstrated promising health benefits, it may only suit some people's lifestyles or individual needs.
An early morning meal can jumpstart metabolism, provide sustained energy, and promote better insulin sensitivity for some individuals.
However, others may struggle to stick to an early breakfast routine due to various commitments or natural hunger patterns. Forcing a specific breakfast time might lead to discomfort or disrupted eating habits.
Ultimately, the focus should be on adopting a balanced and nutritious diet that aligns with individual preferences and supports overall well-being.
Breakfast timing matters to our health.
Research suggests skipping breakfast raises the risk of type 2 diabetes, even with BMI adjustment.
Recent research found that individuals who had their breakfast after 9 AM had a 59% higher risk of type 2 diabetes than those who had it before 8 AM.
Further, those who had frequent small meals throughout the day had a lowered risk for type 2 diabetes.
Early breakfast timing may offer substantial health benefits but only suit some people's lifestyles or preferences.
For those who can accommodate an early morning meal, it could be a beneficial practice to adopt.
However, it's important to maintain a balanced and nutritious diet that aligns with individual needs and overall well-being.
https://www.healthline.com/nutrition/when-to-eat
https://pubmed.ncbi.nlm.nih.gov/32260404/
https://jn.nutrition.org/article/S0022-3166(22)16427-8/
https://academic.oup.com/ije/advance-article-abstract/doi/10.1093/ije/dyad081/7199760
https://www.sciencedaily.com/releases/2023/07/230718105633.htm
Are some people born with a predisposition to cancer? Cancer, the cause of death in 1 in every 6 people, is caused due to a combination of genetic, lifestyle, and environmental factors. While the latter two can be controlled to an extent, we can’t change the genes we are born with. But learning about your genetic profile can help in significantly reducing cancer risk and even preventing it. MUTYH is one such gene associated with cancer risk. It produces an enzyme that repairs DNA damage. Mutation in this gene causes MUTYH associated polyposis, a condition that increases your risk for colon cancer.
Did You Know? Your 23andMe or any ancestry test DNA data includes 700,000 markers, which can be used to learn everything from disease risk and drug sensitivities to nutritional requirements and fitness parameters. Learn more.
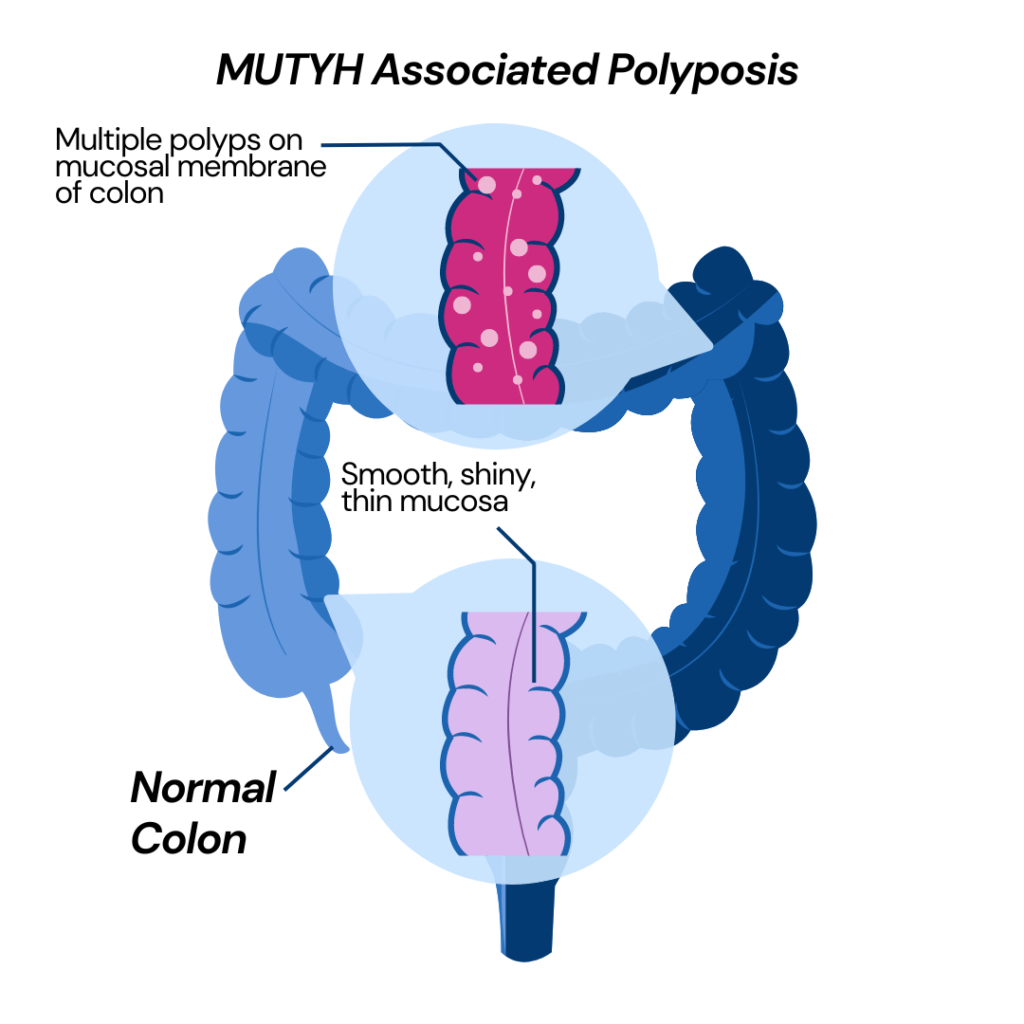
MUTYH-associated polyposis (MAP) is a rare genetic condition where a person has numerous tissue growths in their colon and rectum.
These growths are called adenomatous polyps.
People with MAP can develop between 10 to 100 polyps.
Some people with MAP can develop colorectal cancer with or without polyps.
Mutations in the MUTYH gene cause MAP.
This gene normally plays a kind of 'quality control' role in our cells, helping to fix any mistakes that may occur when our DNA is copied during cell division.
However, when there are errors in the MUTYH gene itself, this repair process can falter, allowing damaged DNA to accumulate.
As a result, other genes responsible for regulating cellular growth, such as APC and KRAS genes, are affected.
MAP typically does not show a lot of symptoms.
Patients can sometimes have the following:
Patients can show other types of growth apart from colorectal growth.
They can have lumps on the thyroid and adrenal glands.
Dental abnormalities such as jawbone cysts are also common for patients having MAP.
Growths inside the eyes called congenital hypertrophy of the retinal pigment epithelium might be present.
Mutations in the MUTYH gene cause MAP.
The two most common mutations are Y165C and G382D.
Additional alterations can be found in complete gene sequencing tests.
To have MAP, a person must have two copies of the mutated MUTYH gene.
MUTYH-associated polyposis is inherited in an autosomal recessive pattern.
It means both parents must be carriers of the disease for it to appear in their children.
The children of two mutation carriers can have three different scenarios:
Studies show that 1 in every 100 people carries a mutation in the MUTYH gene.
You run the risk of being a carrier if either of your parents had the MUTYH gene mutation.
It indicates that you will not suffer from MAP but can pass on the disease to your children.
You will likely suffer from this disease if your parents have a MUTYH gene mutation.
People with MAP are at an increased risk of developing colon and rectal cancer.
Almost half of all people with MAP will have colorectal cancer at diagnosis.
Those with a single MUTYH gene mutation have a higher chance of developing cancer.
Most colorectal cancers occur between 40 to 60 years of age.
MAP increases the chances of thyroid and duodenal cancer.
The gene mutation associated with MAP affects all the cells of the body.
Patients with MAP run the risk of developing stomach polyps and duodenal adenoma.
Chances of breast and ovarian cancer are also increased in women suffering from MAP.
Genetic testing is required to diagnose MAP.
Your symptoms and family history will also help determine whether you suffer from MAP.
You have an increased risk of MAP if
Patients diagnosed with MAP should undergo screenings to monitor their condition and rule out possible cancer.
The screenings suggested by doctors are:
MAP genetic testing helps doctors see if you have changes or mutations in your MUTYH gene.
Anyone can do this test, but it's especially useful if you or your family have had many colon polyps or colon cancer.
A doctor or genetic counselor will guide you on how to do this, often through a simple blood test.
If you test positive, it means you have a mutation.
It doesn't mean you have or will get cancer, but you're at higher risk. Doctors will guide you on what to do, like getting more regular colon checks.
If you test negative, it means you don't have the mutation.
But it doesn't mean you won't ever get colon polyps or cancer, so you should still follow your doctor's advice for routine checkups.
Remember, this test is just a tool. It's a way to understand your risk so you and your doctors can make the best health decisions.
MAP cannot be cured.
Treatment focuses on preventing cancer and maintaining a healthy lifestyle for patients.
Patients are advised to undergo regular colonoscopy to monitor their condition.
If there are less than 20 polyps, they can be removed by a polypectomy procedure during colonoscopy.
If the polyps are numerous and growing fast, then surgical removal of the colon or rectum may be necessary.
This procedure is called colectomy.
Laparoscopic surgery has made colectomy a less painful and disabling procedure.
Surgical intervention might be the last resort to prevent cancer.
Some non-steroidal, anti-inflammatory drugs, such as sulindac, can reduce and prevent the growth of polyps.
Thyroid ultrasound and genetic testing are also recommended for MAP patients.
MUTYH Associated Polyposis (MAP) is a rare genetic condition with abnormal growths on the colon and rectum, called polyps.
This condition makes the patient prone to develop colorectal cancer.
It also increases the chances of thyroid, breast, and ovarian cancers.
MAP can be diagnosed by genetic testing.
This condition does not have a cure.
Treatment includes surgically removing the polyps or laparoscopic surgery to remove the colon or rectum.
Patients should be regularly monitored to rule out possible signs of cancer.
https://my.clevelandclinic.org/health/diseases/17254-myh-associated-polyposis
https://rarediseases.info.nih.gov/diseases/10805/myh-associated-polyposis
https://www.ncbi.nlm.nih.gov/books/NBK107219/
https://www.nature.com/articles/s41467-022-30916-1
https://www.cancer.org/cancer/types/colon-rectal-cancer/about/what-is-colorectal-cancer.html
https://www.who.int/news-room/fact-sheets/detail/cancer
Do you struggle to concentrate or feel mentally tired, even after a good night's sleep? If you're constantly feeling that your brain's "hazy," you may be experiencing what is known as "brain fog."
While not a medical term, brain fog is commonly used to describe symptoms caused by underlying health issues or lifestyle factors. It can make it hard to think and feel productive and even affect your mood.
Identifying the root cause of your brain fog can help you find ways to improve your cognitive function and feel more like yourself again.
In this article, we'll explore common signs and symptoms that may indicate you're experiencing brain fog, a self-assessment test for brain fog, and tips for alleviating it.
Brain fog is a commonly reported symptom that affects many people.
It can be described as a feeling of mental confusion or haziness that makes it difficult to think clearly and remember things.
Some people describe it as feeling like their brain is in a fog or cloud, while others may describe it as mentally tired or as if operating on autopilot.
The experience of brain fog can vary from person to person, but it can make it challenging to concentrate, make decisions, and carry out daily tasks.
Brain fog can be a symptom of many conditions, including chronic fatigue syndrome, depression, anxiety, and autoimmune disorders.
Brain fog has many potential causes and can be a symptom of several different medical conditions. Here are some of the most common causes of brain fog:
It's important to note that brain fog can have many potential causes, and it's essential to speak with a healthcare provider to determine the underlying cause and receive appropriate treatment.
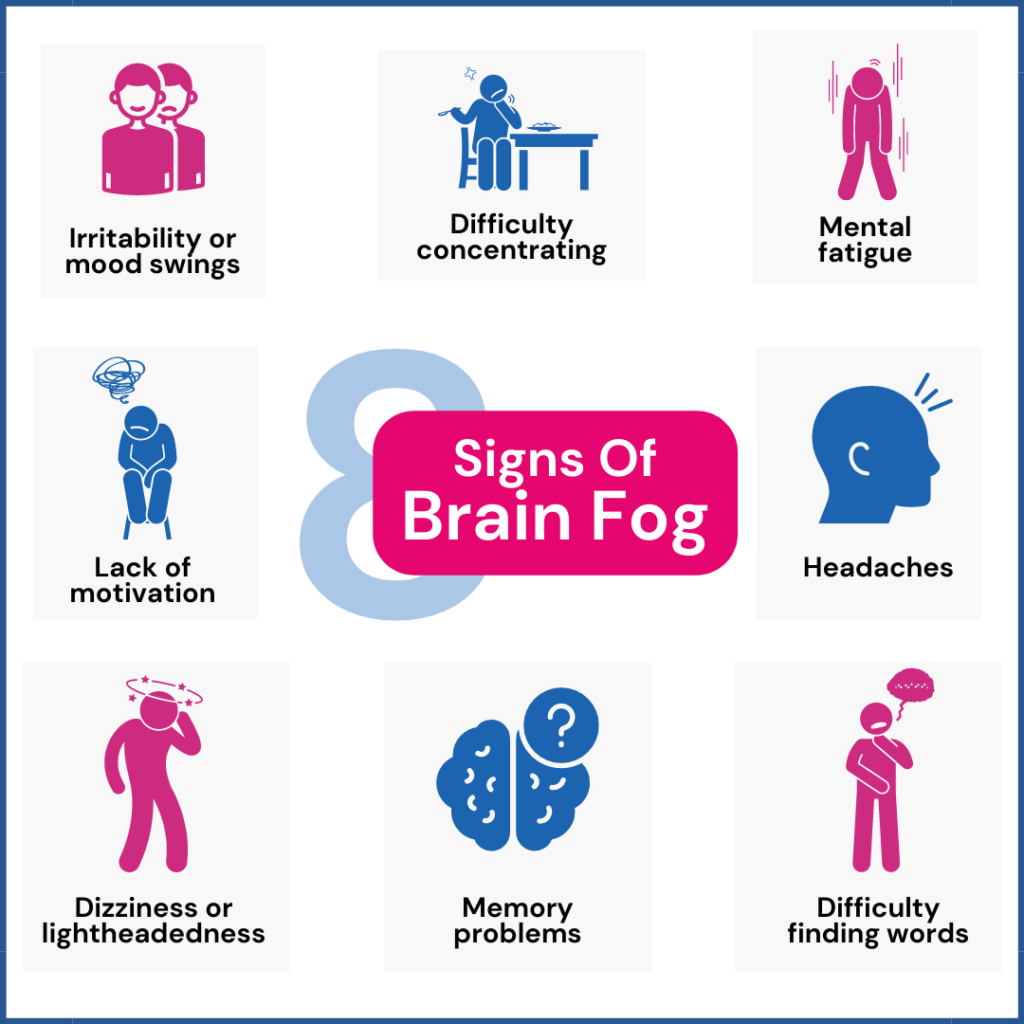
The symptoms of brain fog can vary from person to person, but some common symptoms include the following:
It's important to note that brain fog can be a symptom of several different medical conditions.
So, speaking with a healthcare provider is essential if you're experiencing symptoms of brain fog affecting your daily life.
Scoring
Add up your scores and see where you fall on the scale
Note: This questionnaire is not intended to provide a clinical diagnosis. If you are concerned about your symptoms or if they are affecting your daily life, please consult a medical professional.
If you're experiencing brain fog, there are several things you can do to help alleviate the symptoms. Here are five effective tips to alleviate brain fog:
These tips can help alleviate brain fog, but speaking with a healthcare provider is essential if you're experiencing persistent or severe symptoms.
Brain fog can be a symptom of several medical conditions, and getting an accurate diagnosis and appropriate treatment is essential.
Brain fog is a term used to describe a set of cognitive symptoms. It can be due to various factors, from chronic stress to an underlying health condition.
It often presents itself as difficulty in concentration, memory issues, lack of motivation, and frequent headaches.
Some strategies to manage brain fog include getting adequate rest, regular exercise, and eating a nutritious diet.
It is important to consult a qualified healthcare professional if you are experiencing persistent and severe brain fog.
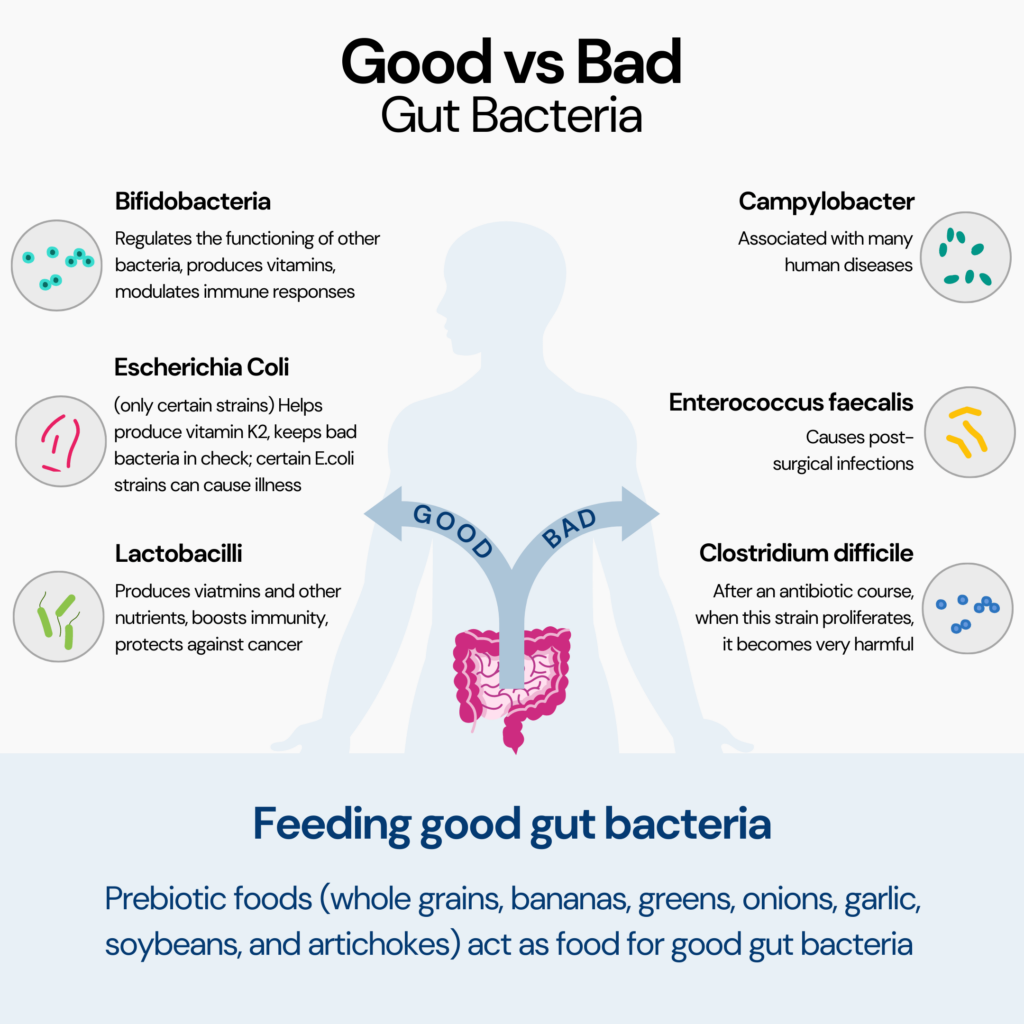
Our gut is a host to a big microbial community that includes both the bad bacteria and the good bacteria. When good bacteria overpowers bad bacteria, our gut is happy, and all’s well. However, do you know what happens when the abundance of bad bacteria increases? Yes, our gut goes kaput, but the imbalance in this microbial community also leads to a higher risk for mental conditions like depression. Keeping this important gut-brain connection in mind, researchers are exploring the idea of “probiotics for depression,” and the results seem very promising.
Did You Know? Your ancestry tests DNA data includes 700,000 markers, which can be used to learn everything from disease risk and drug sensitivities to nutritional requirements and fitness parameters, including your risk for various mental health conditions like depression and anxiety. Learn more.
Probiotics are live microorganisms, typically good bacteria or yeasts, that provide health benefits when consumed adequately.
These beneficial bacteria are commonly found in certain foods and supplements and are known for their positive impact on gut health.
Some help us digest our food better, while others are like little soldiers fighting the bad germs that can make us sick. They even make vitamins that our bodies love!
Many of these probiotics are the same or very similar to the microorganisms naturally living inside us.
So when we take probiotics, we give our body some extra backup to stay strong and keep us feeling great!
Probiotics can be obtained from various sources, making them easily accessible in our daily diet. Some familiar food sources rich in probiotics include:
While probiotics share the common characteristic of being beneficial bacteria, not all probiotics are equal in terms of their effects on health.
Different strains of probiotics have specific functions and benefits.
Think of probiotics like a diverse team of tiny helpers.
Some strains may be superstars at promoting good gut health, while others might have special talents in supporting our immune system.
They all work together, but their specific roles can vary.
Each species and strain might impact our bodies differently, so learning more about their unique characteristics is essential.
Probiotics offer many health benefits that can make a real difference in our feelings.
Probiotics are usually well-behaved, causing little to no trouble for most people.
However, some people might initially experience mild issues, like bloating, gas, or diarrhea, after taking the supplements.
But, if you notice any following side effects such as:
Then consult with your doctor before giving probiotics supplements another try.
They'll help determine what's causing the disturbances and suggest a different blend of probiotics or adjust the dosage.
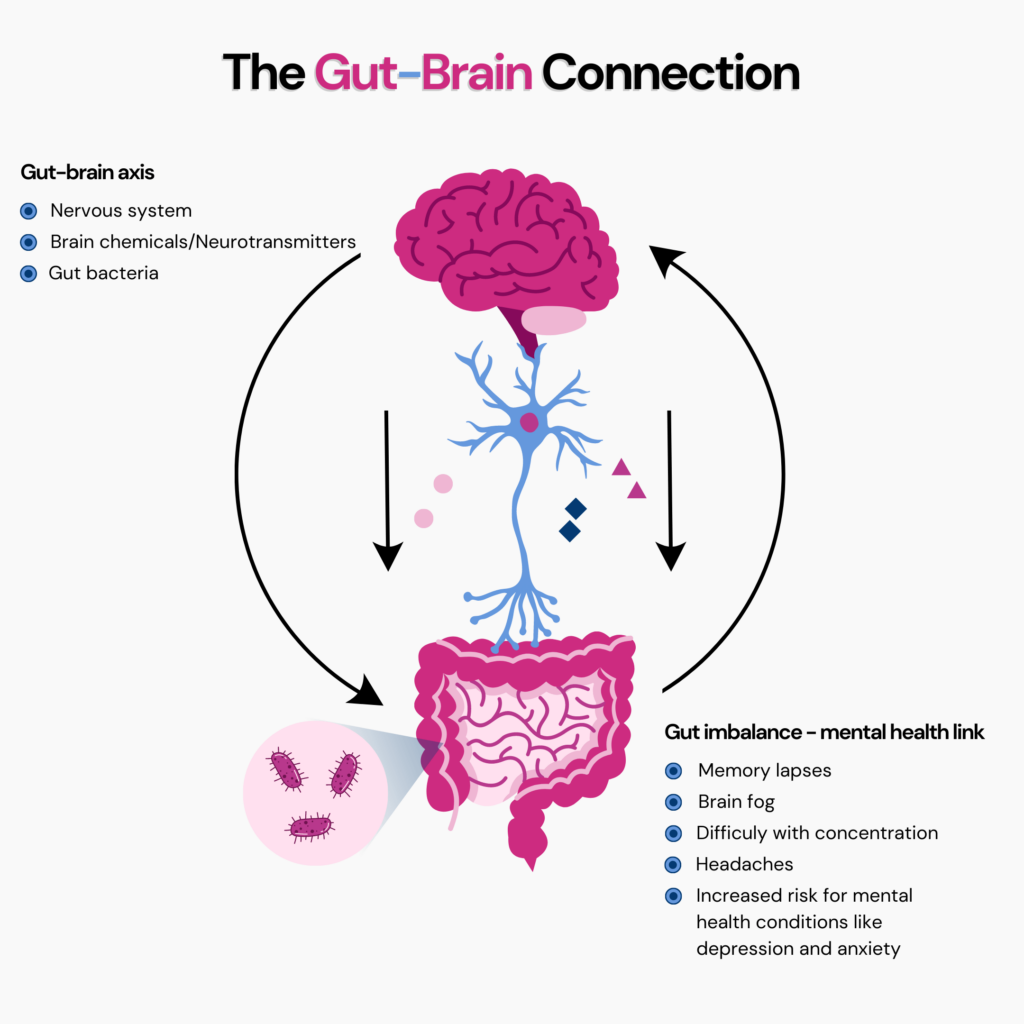
You know that feeling when something big happens, and your gut starts doing flip-flops? Or when stress makes your stomach feel queasy? The real reason behind those sensations is the gut-brain connection at work.
Our gut and brain are like best buddies, always chatting. When we're anxious, depressed, or excited, our gut can feel it too.
It's like our emotions have a direct line to our stomach.
This connection goes both ways.
When our gut is troubled, it can send signals to our brain, affecting our feelings.
When our brain is stressed, it can mess with our stomach, causing gut troubles.
So, neglecting our gut health can also impact our mental health.
Genetic Testing For Mental Health: How To Go About It
Our gut and brain have this incredible connection called the gut-brain axis (GBA).
The GBA links our brain and spinal cord to our gut, where probiotics do their magic. They create neurotransmitters that affect our mood and feeling.
In clinical trials, probiotics like Lactobacillus and Bifidobacterium have shown promise in supporting mental health.
But we're all unique, and so are our gut buddies. How we experience mental health symptoms and how probiotics work for us can differ.
Various factors, such as our genes, life experiences, and the specific combination of gut bacteria, influence our overall mental well-being.
Even though we're still on this exciting journey of discovery, scientists are digging for the right probiotics and dosages to improve mental health.
To comprehend the mechanism behind probiotics for depression, let's split some valuable information to acquire a better grasp.
The effect of probiotics on depressive symptoms: A 2017 systematic review
The researchers looked at 5 databases to see whether probiotics for depression can actually work.
They examined the ten studies that met the criteria, focusing on mood, anxiety, and thinking skills.
Many studies have shown promising results that suggest probiotics can help alleviate depression.
The challenging aspect lies in the fact that each study had a significant variation in the types of probiotics used, the amount consumed, and the duration of consumption.
Interestingly, none of the studies checked how probiotics affected sleep, which is a big deal for people with depression.
Overall, the results look hopeful for using probiotics to help with depression.
However, further studies with larger groups of people are necessary to obtain more definitive conclusions.
The efficacy, safety, and tolerability of probiotics on depression: A 2021 pilot study
The researchers investigated the potential of probiotics to alleviate depression in patients who had not previously received treatment.
The study involved 10 patients with Major Depressive Disorder (MDD) from Kingston, Ontario, Canada.
The participants consumed a probiotic supplement containing a specific strain of bacteria once daily for 8 weeks.
The researchers measured the patient's depressive symptoms at the beginning of weeks 4 and 8.
The results were promising. By week 4, significant improvements in mood-related symptoms were observed, and these improvements continued through week 8.
By week 8, the patients reported improved subjective sleep quality.
The supplement was well-tolerated by all the participants without any side effects.
In a research article published by PubMed in 2016, the most used probiotics with promising benefits for brain health and depression were identified as follows:
The studies included human and animal research with these probiotic doses ranging from 108 to 1010 CFU for 2 weeks in animals and 4 weeks in humans.
The results indicated that these probiotics may positively impact central nervous system function and mental health, showing potential improvements in anxiety, depression, and memory abilities.
However, it is crucial to acknowledge that scientific research is ongoing, and staying updated with the latest results is essential.
Individuals with depression or other mental health concerns should seek guidance from healthcare professionals before considering new medications.
Probiotics, the beneficial bacteria in our gut, can improve mental well-being.
They enhance mood, and memory abilities, boost serotonin production, and improve cognitive function. In addition, probiotics to alleviate depression and anxiety may do so by reducing inflammation.
Different strains of probiotics have specific functions and benefits.
The gut-brain axis plays a significant role in this process.
Probiotics are found in yogurt, kefir, kimchi, sauerkraut, miso, and pickles.
Scientific research suggests probiotics may alleviate depression symptoms.
Further studies with larger groups are needed for more conclusive results.
Consulting healthcare professionals is essential before considering probiotics for mental health.
https://my.clevelandclinic.org/health/articles/14598-probiotics
https://www.healthline.com/nutrition/11-super-healthy-probiotic-foods
https://www.medicalnewstoday.com/articles/probiotic-supplements-may-help-with-depression
https://www.healthline.com/nutrition/8-health-benefits-of-probiotics
https://www.healthline.com/health/probiotics-depression
https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6971226/
https://www.frontiersin.org/articles/10.3389/fpsyt.2021.618279/full
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5319175/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/
https://pubmed.ncbi.nlm.nih.gov/27413138/
Too much cholesterol and heart disease risk is a well-established connection. However, a lesser-known link would be that between cholesterol levels and ApoE Alzheimer's risk. Intrigued yet? Turns out, the same genes implicated in Alzheimer’s also have a role to play in cholesterol clearance from the body. A new study has revealed surprising insights into how fluctuating cholesterol levels can increase Alzheimer’s risk.
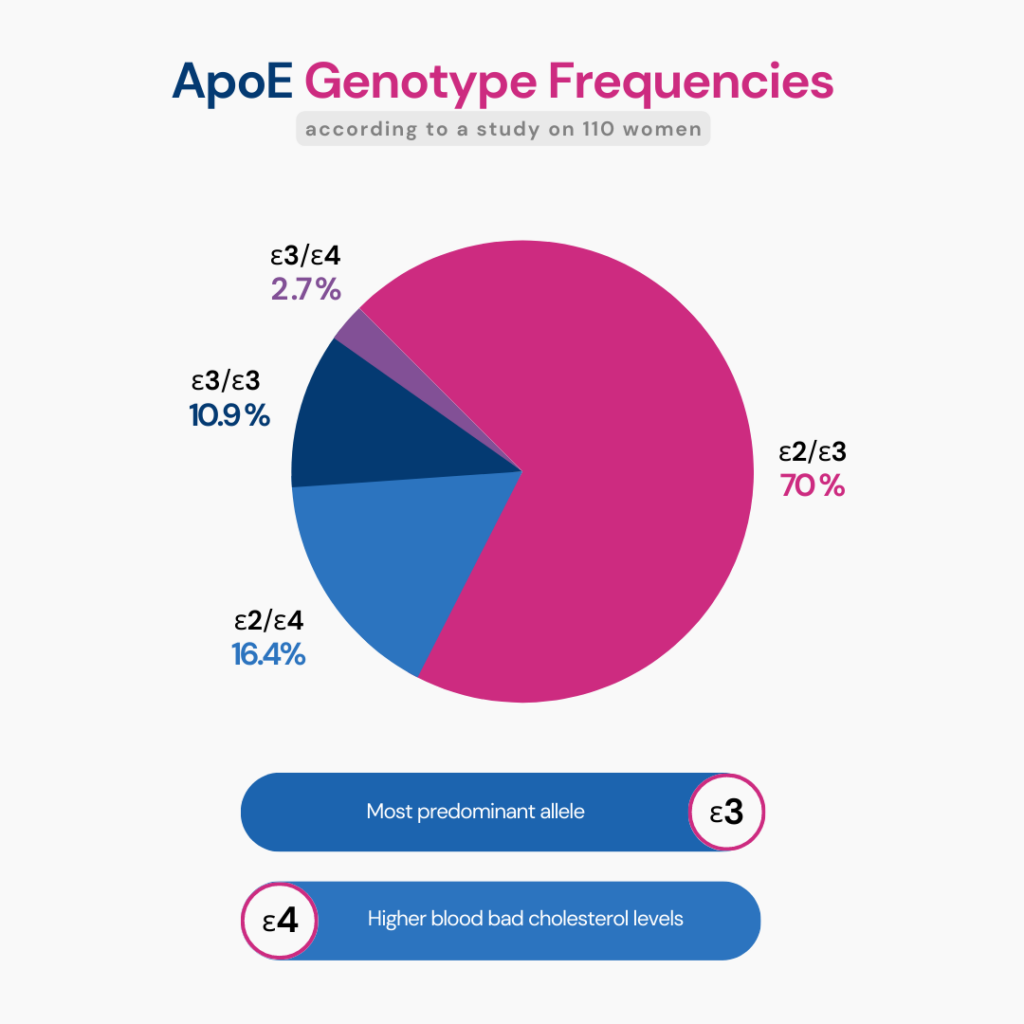
Did You Know? ApoE gene comes in 3 forms, E2, E3, and E4, each of which affects cholesterol metabolism. One particular form is associated with poor cholesterol removal and a resultant increased risk for heart disease. Watch this video to learn more:
Alzheimer’s is a common type of dementia affecting 5.8 million American adults.
This condition is characterized by memory loss, poor judgment, inability to participate in a conversation, and mood and behavioral changes.
As the condition progresses, it can lead to complete memory loss and the inability to speak, walk, or even swallow.
Beyond 65, the risk of developing the condition doubles every five years.
Currently, Alzheimer’s disease doesn’t have a cure. It can only be managed with medications and intervention strategies.
Cholesterol is a waxy, fat-like substance produced by the liver and found in many food sources.
Cholesterol is an integral component of cell membranes to maintain their fluidity and integrity.
The body also needs cholesterol to make vitamin D, bile acid, and steroid hormones.
Excess cholesterol in the blood can combine with other substances and form plaque.
Plaques are deposits that stick to the inner walls of blood vessels and cause blocks.
Plaque buildup is a common cause of coronary artery disease.
High cholesterol levels are also associated with increased risk of peripheral artery diseases, hypertension, stroke, and high blood pressure.
Genetic Testing For Familial Hypercholesterolemia
The Central Nervous System (CNS) stores up to 25% of the cholesterol levels in the body.
Cholesterol levels play a role in the physiological functioning of the brain.
According to experts, very little dietary cholesterol enters the brain because of the Blood Brain Barrier.
The brain cells synthesize most of the cholesterol that the brain needs internally.
The brain needs cholesterol for the following functions.
Membrane cholesterol plays a vital role in the formation of amyloid-β.
Amyloid-β is a type of amino acid that is associated with the pathology of Alzheimer’s disease.
In adults, cholesterol is biosynthesized in the astrocyte cells (types of cells in the CNS).
The cholesterol is transported to the neurons via Apolipoprotein E lipoproteins (ApoE lipoproteins).
Synapse formation requires cholesterol transfer from the astrocytes to the neurons. This process is ApoE-dependent.
The ApoE gene helps produce the ApoE lipoprotein.
Mutations in the ApoE gene cause issues in ApoE lipoprotein production.
ApoE Gene & its Genotypes
This can affect cholesterol transfer and may contribute to the development of Alzheimer’s disease.
There are three common isoforms of this gene identified.
In July 2023, research published in the American Academy of Neurology analyzed the relationship between fluctuating cholesterol levels and Alzheimer’s risk.
The researchers picked 11,571 individual healthcare data of people over 60 for the study.
These individuals did not have a previous diagnosis of dementia or Alzheimer’s.
They were followed up for thirteen years to keep track of their fluctuating cholesterol levels and Alzheimer’s risk.
The participants were divided into five groups based on how much or how little their cholesterol and triglyceride variations were.
In the thirteen years of follow-up, 2,473 subjects were diagnosed with Alzheimer’s or other forms of dementia.
The following variables that could affect the risk of developing dementia were adjusted while calculating the results.
The researchers observed that people in the high-fluctuating cholesterol category had a 19% increased risk of developing some form of dementia compared to the low-fluctuation group.
Similarly, individuals with the highest triglyceride fluctuations had a 23% increased risk of developing some form of dementia compared to the group with lower fluctuations.
Did You Know? Your ancestry test DNA data includes 700,000 markers, which can be used to learn everything from disease risk and drug sensitivities to nutritional requirements and fitness parameters, including your risk for Alzheimer's. Learn more.
The following dietary changes can help bring down overall cholesterol and triglyceride levels.
When practiced regularly, low or moderate forms of aerobic exercises can help reduce overall cholesterol levels.
Excess body fat is one of the common reasons for developing high cholesterol and triglyceride levels.
A 2004 systematic review reports that for every 10 kilograms of weight lost in obese and grossly overweight individuals, a drop of 0.23 mmol of cholesterol could be noticed.
Smoking can increase overall cholesterol and triglyceride levels in the body.
Quitting smoking is critical for individuals with high cholesterol levels.
When lifestyle changes aren’t showing effects, or in the case of severely high cholesterol and triglyceride levels, medications to lower cholesterol levels may help.
Some of the common types of cholesterol-lowering medications include the following:
Many research studies report that increased High-Density Lipoprotein (HDL) levels may reduce the risk of Alzheimer’s disease.
HDL, also called good cholesterol, helps carry bad cholesterol from the bloodstream to the liver to help flush them out.
Animal-based studies report that higher levels of HDL may help protect against neuroinflammation and memory deficits.
Other studies report that HDL prevents the vascular accumulation of amyloid-β, a risk factor for developing Alzheimer’s disease.
Increasing HDL cholesterol levels and avoiding overall fluctuating cholesterol levels can reduce Alzheimer’s risk in older adults.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8264368/
https://pubmed.ncbi.nlm.nih.gov/12648780/
https://www.sciencedaily.com/releases/2023/07/230705171104.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6682969/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6844833/
https://pubmed.ncbi.nlm.nih.gov/22269162/
https://www.ncbi.nlm.nih.gov/books/NBK459119/
https://www.nia.nih.gov/health/alzheimers-disease-genetics-fact-sheet
https://pubmed.ncbi.nlm.nih.gov/14969506/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6236809/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6530968/
https://www.sciencedaily.com/releases/2023/07/230705171104.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8264368/
Navigating the intricate pathways of genetics has never been more approachable, thanks to advances in technology like those offered by Invitae Genetic Testing. As one of the industry leaders, Invitae presents an enticing opportunity to dig deeper into your DNA. However, before diving headfirst into the realm of personal genomics, it's essential to be fully aware of the comprehensive services Invitae provides, their implications, and the considerations you need to make. This blog post will offer an in-depth review of Invitae Genetic Testing, ensuring you have all the information necessary to make an informed decision.
Invitae, with its headquarters set in San Francisco, California, is a medical genetics company founded by Randal W. Scott and Sean E. George in 2010. Invitae is a College of American Pathologists (CAP)-accredited and Clinical Laboratory Improvement Amendments (CLIA)-certified clinical diagnostic laboratory.
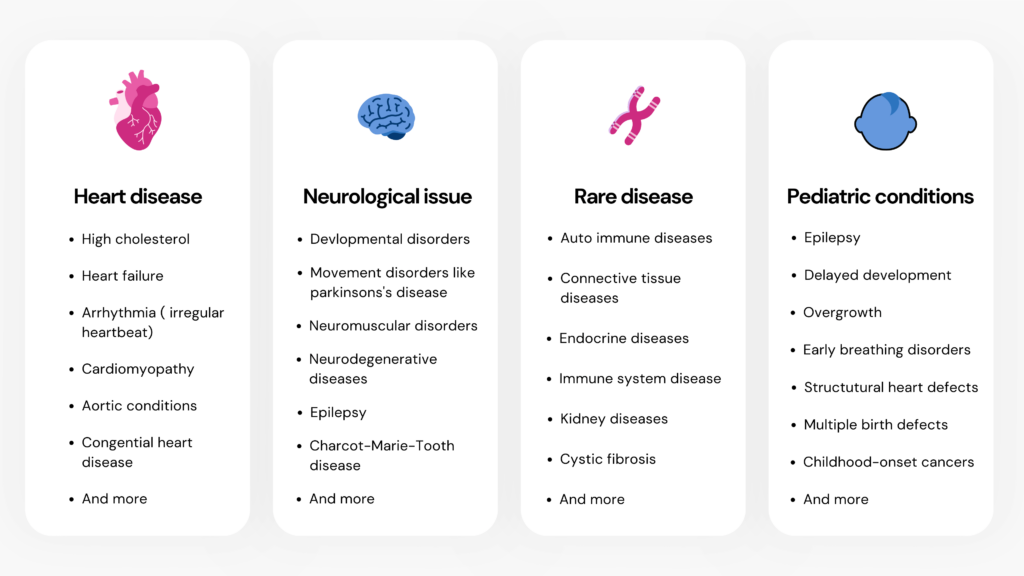
The company offers gene panels and single-gene testing for a broad range of clinical areas, including hereditary cancer, cardiology, neurology, pediatric genetics, metabolic disorders, immunology, and hematology.
Invitae has special tools for medical professionals that help them record family history and provide appropriate genetic testing recommendations.
Invitae offers 4 categories of tests for its users:
Provides information relevant to pre-pregnancy and pregnancy-related decision-making.
It includes the following tests:
Provides information to develop a personalized health plan for cancer and heart disease.
It includes the following tests:
You can order any or all of these tests.
Provides information to help your physician plan an effective treatment.
Looks at 65 genes associated with common cancers
Provides information that helps diagnose and understand the inheritance of various health conditions.
It includes a variety of health conditions grouped under:
Invitae offers a bunch of tests for medical professionals, grouped under the following categories:
Provides genetic information to help professionals tailor chemotherapy and other treatment plans for their patients.
It covers multiple panels, including:
You can view the entire list here.
Provides information that helps medical professionals give insights regarding pre-pregnancy, infertility, and other pregnancy issues.
The tests are grouped under 2 packages:
Provides information to enable medical professionals to inform prognosis, treatment, and next steps for those with rare diseases.
Available panels:
Invitae also offers an RNA-testing feature, which incorporates testing into the variant classification process for variants of uncertain significance (VUS). A VUS is a genetic change in a sequence whose association with disease risk is unclear.
Invitae also offers exome testing options that provide more accurate and reliable results. Exons are a segment of a DNA or RNA molecule containing information coding for the protein. The exome is the part of the genome that consists of exons. It is estimated that the vast majority of disease-causing DNA changes are found in exons.
It includes the following testing options:
Users can choose any test from the options provided and place an order. Once you order, an independent physician will review your health history and approve the test if appropriate.
Once your doctor approves the test, you can sign up with/sign in to your account.
Once your email is verified, you can register a kit using the confirmation code.
Invitae Kit Registration
You can learn about specimen collection and shipping here.
The diagnostic tests under this category may be covered by insurance.
The report begins with a section with patient information and sample collection details (same for all reports).
If it is a "positive result," the next section contains information about the pathogenic variant identified.
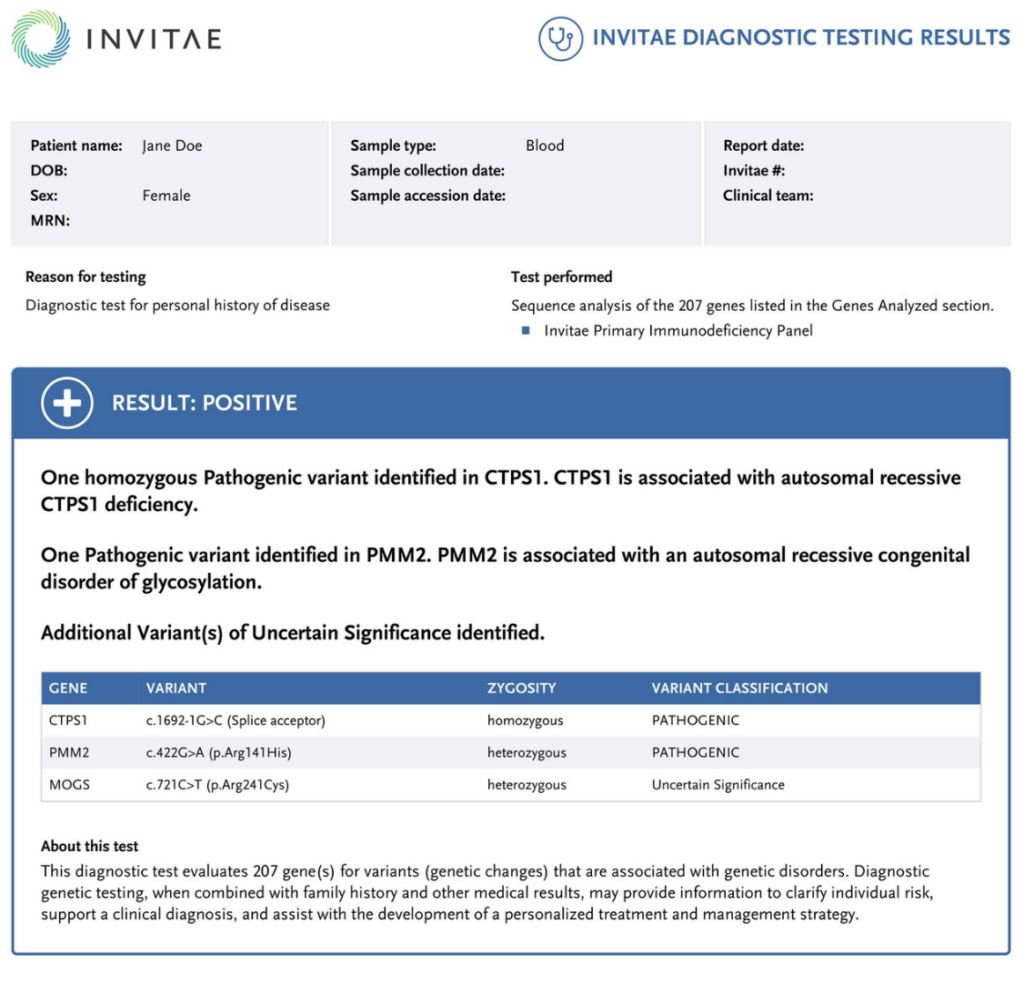
The next section of the report helps users with the next steps after encountering a positive result.
The website also has a "Positive Result FAQ" guide.
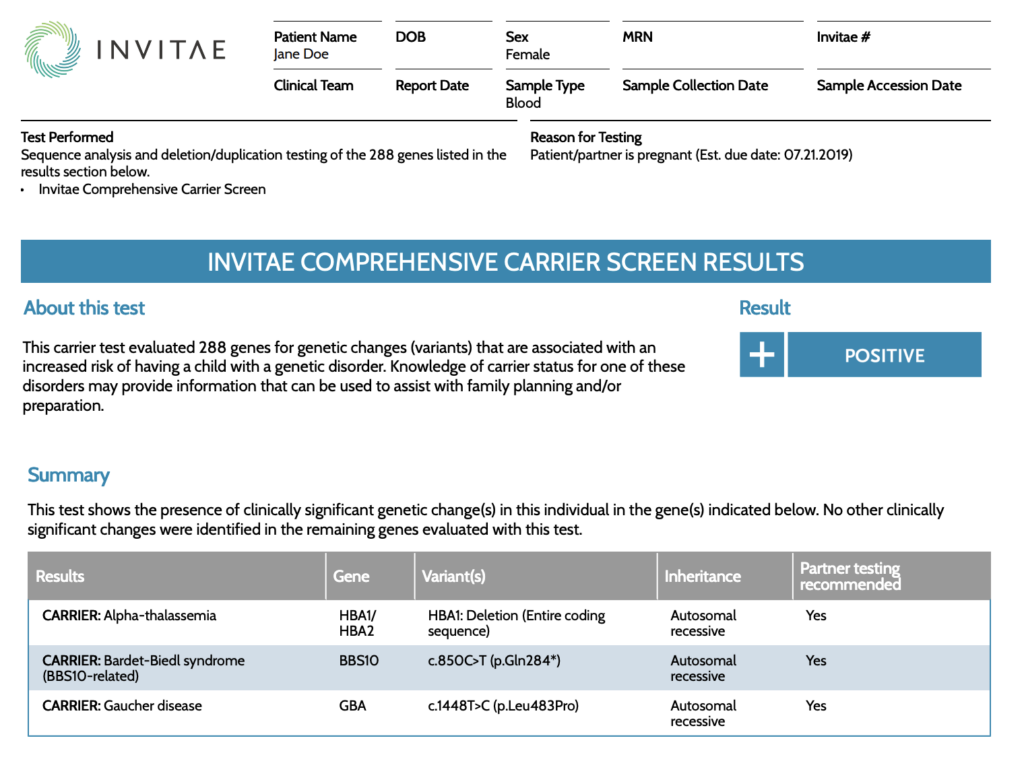
Invitae Carrier Screening
A carrier is an individual that carries one copy of a gene with error(s) associated with a disease, which can be passed down to a child.
If it is a positive result, the report includes information about the variant and the mode of inheritance.
Image: Snippet from Invitae sample carrier screening report
The report also comes with information about the condition and the recommended next steps.
It gives insights into what you can do if your partner tests positive for the same condition.
Invitae Non-invasive prenatal testing
This test covers common genetic disorders, like Down Syndrome, that result from additional or missing pieces of genetic material in the genome.
The report identifies aneuploidies (if present) in chromosomes 13, 18, 21, and sex chromosomes.
Aneuploidy is the presence of an abnormal number of chromosomes.
It is followed by the "next steps" section.
The report ends with the "Limitations" and "Disclaimer" sections.
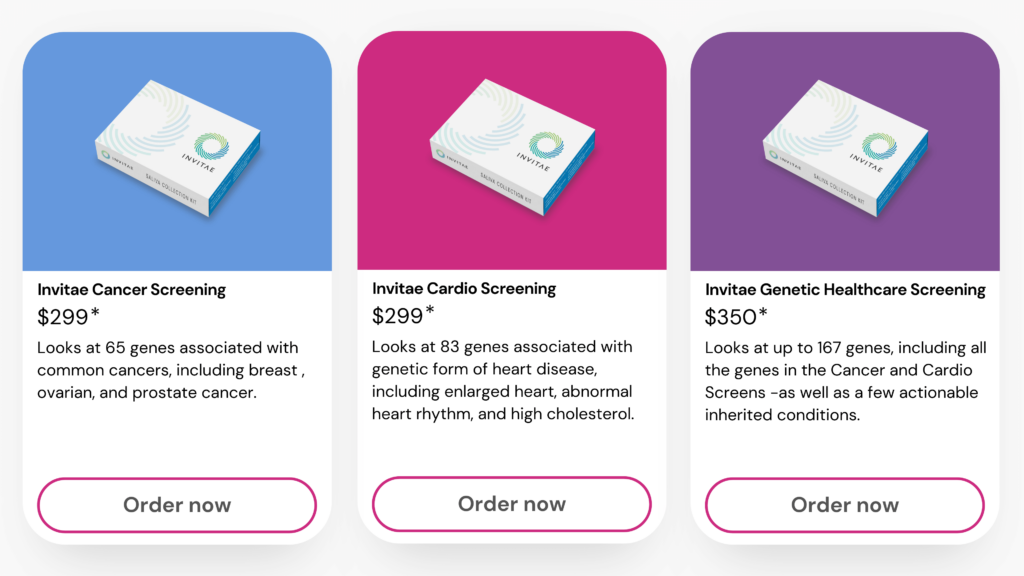
Cancer Screen: The report includes information on 61 genes associated with common cancers like breast, ovarian, and prostate cancer.
Cardio Screen: This test looks at 75+ genes known to influence the risk of many inherited heart diseases like hereditary high cholesterol levels.
Genetic Health Screen: The report provides information on over 145 genes associated with many inherited conditions.
Image: Comparison of the tests in Invitae Proactive/Staying Healthy Pack
| Test | Price |
| Invitae Cancer Screen | $299 |
| Invitae Cardio Screen | $299 |
| Invitae Genetic Health Screen | $350 |
Many of the invitae diagnostic tests may be covered by insurance.
The company also offers Medicare and Medicaid beneficiaries for patients residing in the US if they meet the eligibility criteria.
Invitae offers testing at little or no expense for patients who qualify through their Patient Assistance Program.
Invitae also offers sponsored testing, partnering with biopharma companies like Alnylam to provide genetic testing for selective genetic diseases for patients who meet eligibility criteria.
The company claims that they do not sell or share users’ identifiable data with any third parties. However, they share information about genetic variants and anonymized genetic information with service providers, business partners, and third-party or public databases for research purposes. In addition, Invitae allows users to alter their privacy settings manually.
Invitae’s privacy policy may change from time to time, with updates posted on the website.
| Invitae | Xcode Life | |
| DNA kit | Provided | Not provided |
| DNA raw data upload | Not allowed | Allowed |
| DNA data exploration tools | Not available | Available |
| Report updates | No | Quarterly |
| Report price | $250 or $350 | Individual reports: $30 - $50 Bundle packs: $160 - $199 |
| Diagnostic | Yes | No, but the reports are a powerful tool physicians can use to make health recommendations. |
| Report categories | Hereditary cancer, Cardiology, Neurology, Pediatric Genetics, Metabolic disorders, Immunology, and Hematology | Nutrition, Fitness, Skin, Allergy, Health, Personality, Breast Cancer, MTHFR, Personalized Medicine, Sleep, Genetic Reports |