Researchers have identified several genes associated with vitiligo.
In the sample report below, we've attempted to analyze some important genes that increase the risk of vitiligo.
You can identify your genetic risk of vitiligo by using your 23andMe DNA data and placing an order for the Gene Health Report.
Autoimmune diseases occur when the immune system attacks the body, destroying healthy cells.
In normal cases, the immune system can differentiate between healthy body cells and foreign cells and attack only the latter.
In people with autoimmune conditions, this differentiation does not happen.
Vitiligo is an autoimmune condition characterized by loss of pigmentation (color) in the skin.
Melanin is a pigment in the skin, eyes, and hair that gives them color. Melanin is produced by the melanocyte cells.
In this condition, the body’s immune cells start destroying melanocytes. As a result, melanin production is reduced or stopped.
This leads to the formation of white patches on the skin. Over time, the white patches spread throughout the body.
About 0.5% to 2% of people worldwide are affected by vitiligo.
There are two types of vitiligo identified.
This is also called generalized vitiligo and is more common. In this case, the white patches spread throughout the body and are often seen in:
This is also called localized vitiligo or unilateral vitiligo and is more common in children than adults.
The white patches appear on just one or around a limited body area.
The telltale symptom of vitiligo is the appearance of pale or white patches on the skin.
The pigmentation loss usually starts on the hands and face and spreads to other areas.
People also notice that the lighter patches are more sensitive to sunlight and can itch and become red on exposure to the sun.
Vitiligo is a multifactorial condition, which means several factors can cause the condition.
Genetics plays a significant role in causing vitiligo. We will discuss more of this in the coming sections.
Along with genetics, certain factors may trigger the onset of the condition.
Studies confirm that the heritability of vitiligo can range from 46% to 72%. The risk increases when the person has a first-degree relative with vitiligo.
A twin study done among the European population showed that the concordance rate (the probability that two people sharing the same genes will develop the same condition) of developing vitiligo is 23% in monozygotic twins.
According to experts, more than 50 genes could influence the risk of developing vitiligo. Some of these include:
| Gene | Related protein |
| RERE | Arginine-Glutamic acid dipeptide repeats |
| FASLG | FAS ligand |
| UBE2E2 | ubiquitin-conjugating enzyme E2 E2 |
| HLA-A | HLA class I histocompatibility antigen, A |
| IRF4 | interferon regulatory factor 4 |
| TYR | Tyrosinase |
| PMEL | pre-melanosome protein PMEL |
| XBP1P1 | X-box binding protein 1 |
Globally, 1% of the population develops vitiligo.
In the case of people with a first-degree family member with the condition, the risk is up to 5 times higher.
Unlike what people assume, vitiligo does not necessarily skip a generation.
With a first-degree relative with this condition, 1 in 20 people may develop vitiligo too.
Studies show that men and women have an equal risk of developing the condition.
25% of people develop the condition before age 10, and about 70-80% of people start seeing signs before 30 years of age.
If you have a first-degree relative with vitiligo, genetic testing may help know your extent of risk.
If you belong to the high-risk category, taking precautionary measures like the below may help postpone the onset of the condition.
Image: Contributions to vitiligo - Genetics vs. environment
Studies show that up to 25% of people with vitiligo may have another associated autoimmune disease. Other health conditions associated with vitiligo are:
A majority of vitiligo cases could be genetically influenced. Studies say that 46% to 72% of people with vitiligo inherit the condition from family members.
In some cases, a person could have the gene changes affecting vitiligo but not develop the condition or develop it very late in life.
Environmental triggers can hasten the onset of the disease, and 70-80% of people develop symptoms before the age of 30.
Genetic testing may help identify the risk early on and help people take proactive steps to handle it.
According to the Centers for Disease Control and Prevention (CDC), every year, about 800,000 people in the United States have a stroke. In India, it is estimated that about 334-424 people out of 100,000 in urban areas and about 84-262 out of 100,000 people in rural areas suffer from stroke A stroke occurs when a blood vessel that supplies oxygen and nutrients to the brain is either blocked by a clot or bursts. When this happens, part of the brain cannot get the oxygen it needs, so it starts to die. Are strokes hereditary? Keep reading to find out.
Researchers have identified several genes associated with stroke.
In the sample report below, we've attempted to analyze some important genes that increase the risk of stroke.
You can identify your genetic risk of stroke by using your 23andMe DNA data and placing an order for the Gene Health Report.
Stroke is a condition in which the blood supply to the brain is blocked, resulting in a lack of oxygen to the brain cells and, finally, death of brain cells.
It occurs when the blood vessels going to the brain is either blocked by a clot or burst.
A stroke can lead to partial or complete paralysis or even death.
In India, the highest fatality, 42%, from stroke is seen in Kolkata.
In the U.S, stroke is the 5th leading cause of death and the leading cause of disability.
There are three types of strokes, classified based on the type of disruption and the extent of disruption in blood supply to the brain:
The ApoE gene mutation was found to be associated with increased levels of cholesterol, LDL and ischemic heart disease.
It has also been shown to be significantly associated with stroke.
Specifically, the ApoE gene mutation was shown to be associated with carotid intima-media thickness, which plays a role in ischemic stroke.
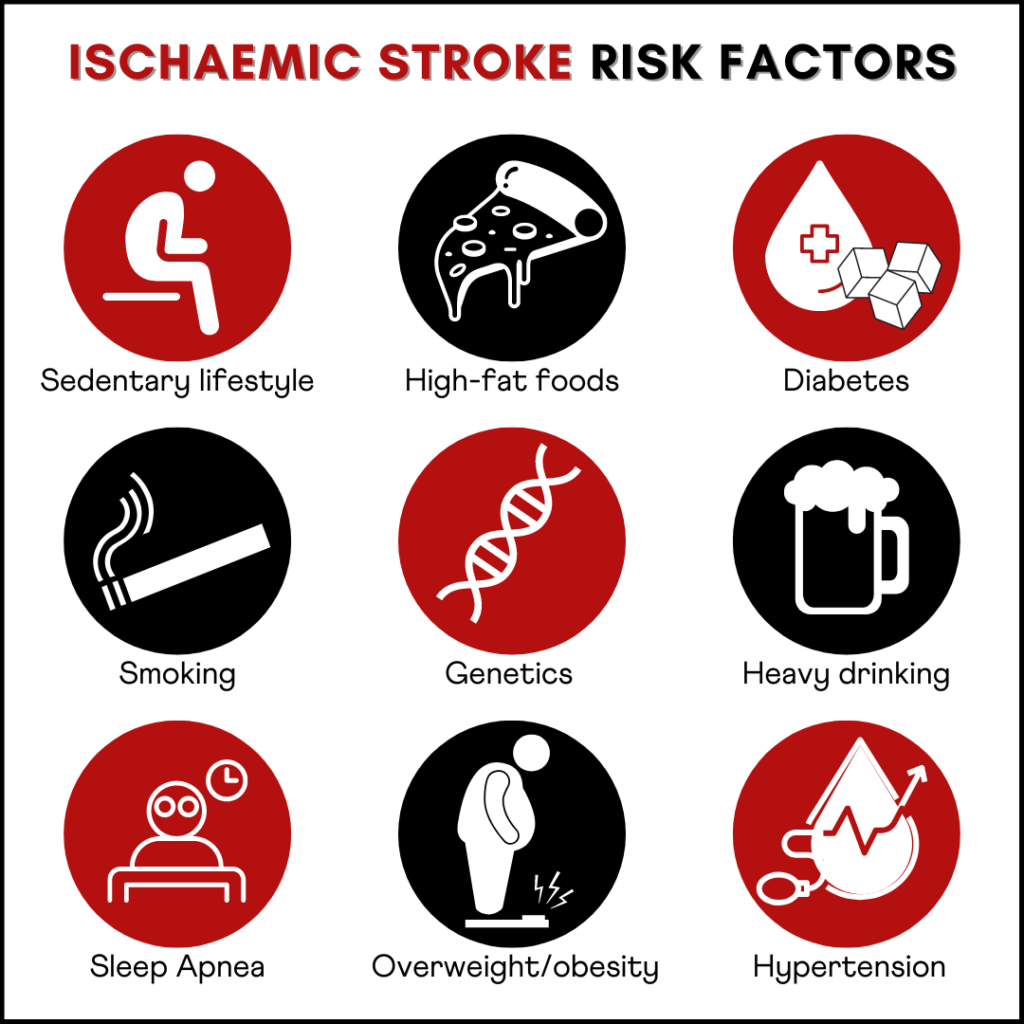
Many vascular conditions are driven by an interplay between genetic factors and environmental factors.
Hence, there has been a surge in circulation-related problems coincident with a surge in the consumption of high-calorific food and an increase in a sedentary lifestyle.
Genetic risk factors, such as the ApoE gene mutation, appear to play a significant role in the disease pathogenesis of stroke.
Testing for this gene mutation may help identify a risk factor and take preemptive actions.
These factors may be modified to reduce the risk associated with the ApoE gene mutation.
In most instances, the severity of stroke can be controlled when the patient is provided with emergency medical support.
Genetic risk is an indicator of risk and does not guarentee disease onset or signify a poor prognosis.
A person with a high genetic risk for stroke should quit smoking, stay active, eat a well-balanced diet, stay away from alcohol, and keep a watch for warning signs and symptoms.
A stroke occurs when blood and oxygen flow to the brain is blocked.
The ApoE gene, famously associated with Alzheimer's, also plays a role in stroke risk.
Environmental factors like a sedentary lifestyle, consuming high-fat foods regularly, and health conditions like diabetes and hypertension can also impact stroke risk.
Common treatment options involve surgically removing the clot.
Physiotherapy and motility aids may help patients move and do some of their personal things to an extent.
Researchers have identified several genes associated with osteoarthritis.
In the sample report below, we've attempted to analyze some important genes that increase the risk of osteoarthritis.
You can identify your genetic risk of osteoarthritis by using your 23andMe DNA data and placing an order for the Gene Health Report.
Osteoarthritis (OA) is a degenerative disease of the joints. The condition makes joints stiff, weak, and painful and reduces mobility.
This is very common in older adults, and OA can affect all body parts, including knees, hands, shoulders, and hips.
Cartilage is a flexible tissue that covers joints and bones.
It allows joints to move smoothly without friction.
OA breaks down the cartilage, so the joints and bones start rubbing against one another as they move. This leads to pain, swelling, stiffness, and lowered mobility.
OA is a wear and tear condition.
As people age, the cartilage and joints go through age-related wear and tear, causing pain and stiffness.
Studies show that up to 35-65% of cases of osteoarthritis could be genetically influenced. We will discuss more on the genetic influences in the coming sections.
There could be so many environmental and lifestyle causes that increase a person’s risk of developing OA.
Some of the commonly experienced symptoms of OA are
Source: https://www.versusarthritis.org/about-arthritis/conditions/osteoarthritis/
Studies show that OA has a polygenic inheritance.
This means that the condition is influenced by multiple genes instead of just one.
The age of onset of OA, its progression, and the severity of the condition could all be influenced by different gene changes and their interactions.
OA in the hands and hips could be 65% inherited, while OA in the knee could be about 40% inherited.
As mentioned above, multiple genes determine a person’s risk of developing OA. Some of the important ones are mentioned below.
The COL2A1 gene provides instructions for producing type II collagen. This collagen makes connective tissues like cartilage stronger and gives them flexibility.
Changes in this gene may lead to a lowered production of type II collagen, leading to early cartilage breakdown and OA.
Other genes that control the production of collagen in the body may also increase or decrease a person’s risk of developing OA. These include
| Genes | Manifestation |
| COL11A1 | Early onset of OA |
| COL11A2 | Early onset of OA |
| COL1A1 | Protective against hip OA in females and people assigned female at birth |
| COL9A1 | Early onset of knee OA |
Interleukins are types of proteins that are produced by White Blood Cells (WBCs).
These play a role in cell-cell communication.
Certain genes that control the production of interleukins may increase or decrease a person’s risk of developing OA.
Some of these interleukin genes are:
| Genes | Manifestation |
| IL-1A, IL-1B, IL1RN | Can cause knee and hip OA |
| IL4R | Can cause hip OA in females and in people assigned female at birth |
| IL6R | Can cause hip OA |
| IL17A, IL17F | Increases risk of developing OA |
Other genes that have been associated with OA are:
| Genes | Manifestation |
| Insulin-like growth factor 1 (IGF-1) | Increases risk of developing OA |
| Matrilin-3 (MATN3) | Can cause early onset of OA in hands and knees |
| Vitamin D receptor (VDR) | Increases overall risk of developing OA |
| Cartilage Oligomeric Matrix Protein (COMP) | Early onset of hip OA |
Some of the non-genetic risk factors for developing osteoarthritis are:
Since OA is a wear and tear disease, the risk of developing the condition increases with age.
OA occurs more frequently in women and people assigned female at birth than men and people assigned male at birth.
Carrying excess weight puts unnecessary stress on the joints, leading to OA.
Any serious injury to the joints that didn’t heal well may increase a person’s risk of developing OA.
Any deformity to joints that happened by birth may increase the person’s risk of developing OA.
Congenital deformities are one of the most common reasons people develop OA in the hip.
When the cartilage gets broken down, the body tries to repair the same using Vitamin D. Lack of vitamin D may prevent the body from healing the cartilage and lead to OA.
Image: Risk factors and treatment for osteoarthritis
While osteoarthritis could result from certain medical conditions, age, and injuries, genetics remains an important cause.
Genetics may influence the age of onset, the progression, and the severity of symptoms of OA.
Genetic testing can help understand your risk of developing the condition. If you have close family members with OA, then genetic testing may help.
Preventive medications, physical activities, and other lifestyle changes can bring down the damage to the cartilage and delay the onset of OA in high-risk individuals.
Triple-negative breast cancer is not as well known as other types of breast cancer, but it is just as serious. This type of cancer is difficult to treat because it does not respond to hormone therapy or targeted therapy drugs. Diet is a key factor that can play a role in your health, and certain foods may help prevent and even fight triple-negative breast cancer.
Estrogen and progesterone are important hormones for the female reproductive system.
Certain cells have receptors (proteins) to which these hormones bind to fuel them.
Breast cancer cells with estrogen and progesterone receptors are ER+ and PR+ breast cancer, respectively.
Her2 is another protein that acts as a growth factor, and breast cancer cells with receptors for this protein is called Her2+ breast cancer.
Triple-negative breast cancer (TNBC) is a type of breast cancer that does not have receptors for the hormones estrogen, progesterone or the Her 2 protein.
Hence, hormonal treatments targeting such receptors are ineffective against TNBC.
Your diet plays a big role in your breast cancer risk.
Consuming processed meats and high-fat dairy can increase your risk while eating plenty of fruits and vegetables can decrease it.
Alcohol consumption is also a factor. Even moderate drinking can increase your risk by 10%.
Maintaining a healthy weight is important, as well. Obesity increases your risk of developing breast cancer, especially after menopause.
According to the American Cancer Society, some foods help boost overall health and reduce the risk of several types of cancers.
Research studies report a link between the Western diet (one that is high in processed foods and added sugars) and an increased risk for breast cancer.
Additionally, Western diet-induced obesity can further increase the risk.
A 2021 study reported that obesity is associated with shorter survival among TNBC patients.
A recent study published in April 2022 analyzed the impact of diet on TNBC chemotherapy response and the risk for chemotherapy-induced heart damage.
The study reported that regardless of the dietary pattern, a high-fat diet increased TNBC growth.
Further, mice fed with the western diet showed cancer metastasis to the lung, and this was not seen in mice fed with the Mediterranean diet.
The former also shower poor cardiac function compared to the latter, with increased fibrosis.
Certain food groups help with a better outcome for TNBC treatment, as well as reduce the risk for TNBC.
They include:
Whole grains, vegetables, fruits, legumes
Phytochemical compounds have anticancer properties
Certain phytochemicals like folate, curcumin, resveratrol, epigallocatechin, and sulforaphane can help manage TNBC.
Recommended foods in this group include broccoli, kale, celery, green tea, turmeric, carrot, spinach, and pears.
According to findings presented at American Association for Cancer Research conference 2013, omega-3 fatty acids can slow down TNBC.
Foods rich in omega-3 fats include salmon, chia seeds, walnuts, and cod liver oil.
Limiting or avoiding the following food items/groups can help with slowing down the progression of TNBC, increase the likelihood of favorably responding to treatments, and reduce the overall risk for TNBC.
TNBC is one of the toughest types of breast cancer to treat since the cancer cells do not have any hormone receptors.
Diet plays a major role in influencing cancer risk, cancer progression, treatment outcome, and survival.
A diet high in processed foods, sugar, and fats has been linked to an increased risk for TNBC and poor chemotherapy outcomes.
A diet rich in whole grains, phytochemicals, omega-3 fats, fruits, and vegetables can help reduce the risk of all types of cancer and can further help with slowing down cancer progression.
About 1 in 4 people faint at some point in their lives.
Fainting or passing out is when an individual loses consciousness for a short period.
This commonly occurs when a sudden decrease in blood pressure causes reduced blood flow to the brain.
A fainting episode typically lasts for a few seconds or minutes.
Though fainting is usually not a cause of concern, it is important to seek medical attention if it happens too often.
A few other causes of fainting include:
Image: How to help someone who has fainted
A few factors increase the risk of fainting, and these include:
Fainting is not just caused by external factors. Your genes have a role to play as well.
A study published in the Neurology journal stated that fainting has a strong genetic component, but it may be affected by multiple genes and environmental factors.
The same study also said that the frequency of fainting among non-twin relatives was low, which suggests that the condition is neither inherited nor caused by a single gene.
Danish researchers found that a part of chromosome 2 may increase an individual’s risk for fainting.
Humans have 23 pairs of chromosomes, i.e., 46 chromosomes.
An individual can have one, two, or no fainting-related genes on chromosome 2.
People with the fainting risk variant on both versions of chromosomes have a 30% higher risk of fainting than those without the variant.
Though some studies indicate that women may be at a higher risk of fainting than men, the exact reason for this is unknown.
Image: 5 facts about fainting
If you have experienced fainting in the past, it is important to observe which activities trigger it. Knowing what triggers your fainting spells can guide you toward avoiding them.
A few strategies you can use to prevent fainting are:
If your fainting episodes are due to a medical condition, your doctor will recommend suitable measures to prevent it.
Kidney stones are mineral and salt deposits that form in the kidneys and affect the functioning of the urinary tract.
Kidney stones are also called nephrolithiasis (NL) or renal stones. According to studies, about 8.8% of Americans develop kidney stones.
About 75% of renal stones are made of calcium. These can also be made up of uric acid, cystine (a protein building block), or minerals like struvite.
Kidney stones can be of different sizes and must pass out of the body through urine.
Smaller stones may pass through the urinary tract unnoticed or with minimal discomfort.
Larger kidney stones can block urine flow and lead to kidney complications. Different factors influence the creation of kidney stones, and genetics is one of them.
Kidney stones often show no symptoms until they start moving and enter the ureters.
The ureters are tubes that carry urine from the kidney to the bladder.
If the kidney stone blocks the ureters, it can give rise to symptoms like
It is often not easy to identify the exact cause of kidney stones.
Stones can develop when your urine has an excess of calcium, uric acid, cystine, struvite, or oxalate, all of which can form crystals and develop stones.
Sometimes, the contents in your urine may encourage crystals to stick together. This may cause stone formation.
We will discuss some risk factors for kidney stones in the coming sections.
Kidney stones are multifactorial (influenced by multiple factors). Genetics, environmental causes, diet, and hormonal changes can play a role in causing the condition.
Inheritance of kidney stones
The inheritance pattern of kidney stones is unclear.
People with a sibling or a parent with kidney stones have an overall increased risk of developing the condition.
Two-thirds of people with calcium-based kidney stones have close relatives with the same condition.
Multiple genes may influence the formation of kidney stones.
Some of the important ones include:
| Gene | |
| ADCY10 | Adenylate cyclase 10 |
| APRT | Adenine Phosphoribosyltransferase |
| SLC26A1 | Solute Carrier Family 26 Member 1 |
| SLC22A12 | Solute Carrier Family 22 Member 12 |
| SLC2A9 | Solute Carrier Family 2 Member 9 |
| SLC34A3 | Solute Carrier Family34 Member 3 |
| VDR | Vitamin D Receptor |
Changes in these genes may cause an imbalance in the urinary inhibitors and promoters of crystallization, increasing or decreasing a person’s chances of developing kidney stones.
Some risk factors that may lead to kidney stones are:
When treating kidney stones, the options vary depending on the size of the stone, the physical discomfort it causes, and the pressure it puts on the kidneys.
For smaller stones, doctors may advise drinking 3-4 liters of water daily to help pass the stone.
For slightly larger kidney stones, the doctor may suggest a particular type of medication called an alpha-blocker.
This relaxes the ureter muscles and helps pass the stone quickly and painlessly.
For larger stones that block the ureter and put pressure on the kidneys, there are three treatment options considered.
Extracorporeal Shock Wave Lithotripsy (ESWL) - Sound waves create vibration and break the larger stone into smaller pieces, which can then be easily passed on in the urine.
Ureteroscopy - A small telescope is passed through the urethra to identify the stone. This is then broken into smaller pieces using special instruments.
Percutaneous Nephrolithotomy - This is a minimally invasive technique where a small incision is made at the back of the body, and a camera and small instruments are sent through the incision to the kidneys. The stone is broken and removed surgically.
Genetic testing will help you understand your risk of developing kidney stones.
Even if you are genetically prone to developing stones, some lifestyle changes below may help combat the risk.
A condition called percutaneous nephrolithotomy may cause high calcium levels in the body, and this could be a reason why a person develops kidney stones frequently.
Controlling the activity of the parathyroid glands may help handle this condition.
Kidney stones, especially the ones caused by excess calcium crystallization, may be genetically influenced.
In most cases, a combination of genes, environmental causes, and lifestyle leads to the formation of kidney stones.
Making small lifestyle changes and testing your genes can help you stay aware of the condition and get treated early on.