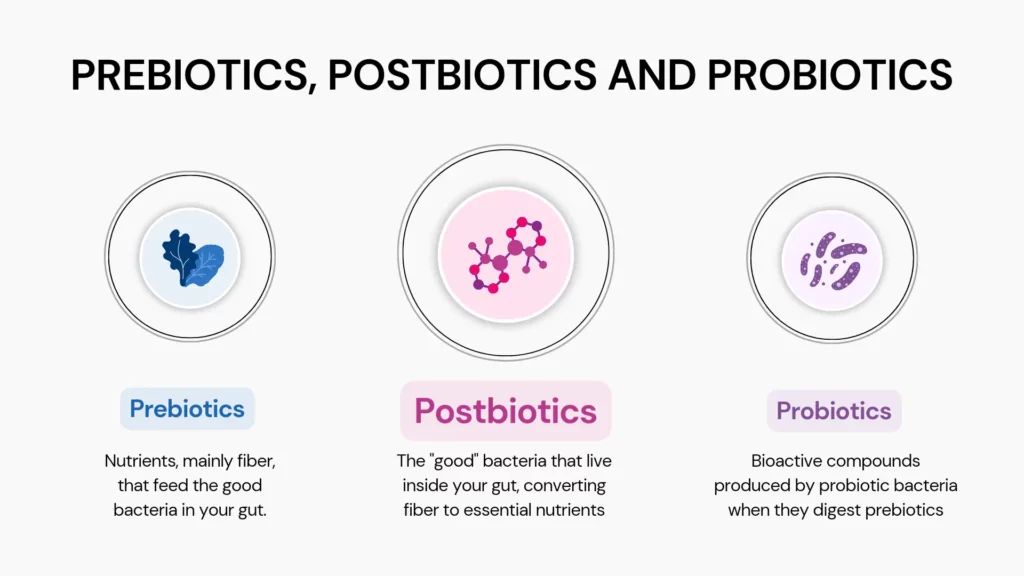
Did you know you could rely on bacteria to improve your health? The numerous 'friendly' bacteria in our body support our gut health efficiently. Research has focused on probiotics and prebiotics to nurture this delicate gut microbiome balance. Now, a new promising player has emerged: postbiotics, also known as metabolites or cell-free supernatants. Read on to understand what they are, where they come from, and how they can support your health in ways you wouldn't expect.
The International Scientific Association of Probiotics and Prebiotics (ISAPP) formally defined the concept of postbiotics in 2021.
According to the ISAPP, the term postbiotics refers to 'preparations of inanimate microorganisms and/or their components that confer health benefits on the host.'
Beneficial gut bacteria produce short-chain fatty acids, B vitamins, enzymes, and amino acids.
These substances are postbiotics and are important to overall health and wellness.
For instance, amino acids are the building blocks of protein, and vitamin B supports your brain health and immune function.
Thus, postbiotics are byproducts of probiotics that support your health.
Here are some examples of postbiotics:
Since probiotics are live microorganisms, keeping them alive and stable is necessary but could be a challenge.
Also, the risk of infection increases since your body is dealing with live bacteria.
Postbiotics, on the other hand, are easier to formulate and store and have a longer shelf-life.
Postbiotics are usually well-tolerated.
You won't run the risk of developing an infection or allergy.
You can take probiotics along with postbiotics for maximum health benefits.
Your gut bacteria's stability depends on age, diet, and environmental factors.
Taking them together will help maintain a balance in your gut microbiome.
Scientists have yet to fully understand how postbiotics work.
However, butyric acid, a well-known postbiotic product, might help us understand it better.
Bacteria use butyric acid, a short-chain fatty acid, as fuel.
It can alter the levels of certain bacteria in your colon.
Your colon has the highest levels of bacteria compared to anywhere else in the body.
It's important to regulate them to support your immune system.
Scientists have found that you can manipulate bacterial presence in your colon by increasing butyric acid levels.
That's an example of the effects that postbiotics have on our gut.
Some research has shown that postbiotics can improve digestive health and support the immune system.
Some additional benefits of postbiotics include:
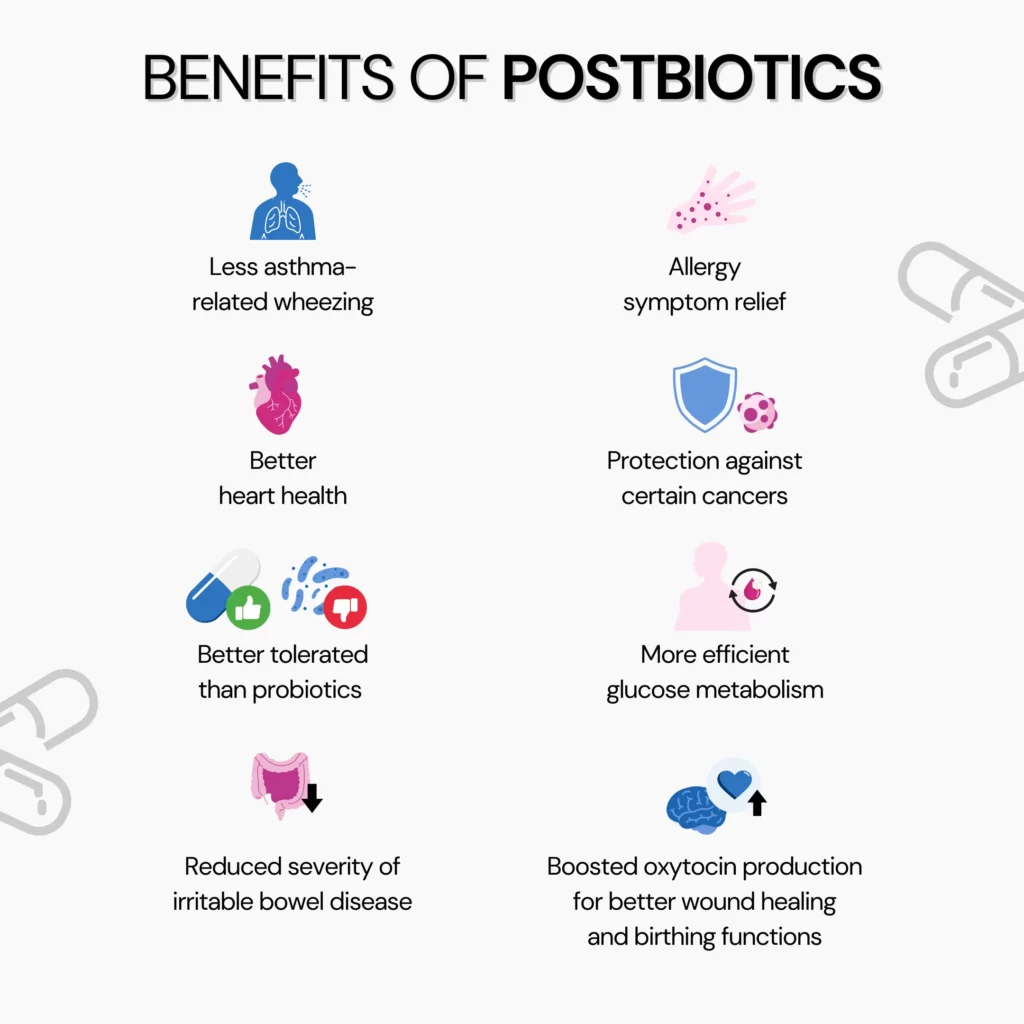
Despite limited research, some studies have shown that postbiotics might aid weight loss.
Postbiotics like short-chain fatty acids can suppress hunger signals, thus aiding in weight loss.
You can naturally boost postbiotic levels in your body by eating probiotic and prebiotic-rich foods.
When your gut bacteria get more fiber to feed on, they naturally produce more postbiotics.
Some prebiotic-rich foods are oats, barley, chia seeds, flaxseeds, onions, and garlic.
Fermented foods like kimchi, yogurt, kefir, tempeh, miso, and sourdough bread also help boost gut bacteria.
The gut bacteria, in turn, increase postbiotics in the body.
Hand-picked Article For You: Difference Between Pre And Probiotics
Postbiotic supplements contain a concentrated dose of short-chain fatty acids, peptides, or enzymes.
They act as food for your gut bacteria and help them thrive.
They can also influence your immune system, regulate inflammatory response, and boost overall immunity.
Taking postbiotic supplements could be beneficial if you're targeting specific health concerns.
Supplements are a simple and reliable way to ensure you get your required dose.
Always consult your doctor before starting any supplements.
Most postbiotic supplements are safe.
However, you should still be careful and regularly consult your healthcare provider.
Research around postbiotic supplements is still in the initial stages.
Thus, when buying a supplement, ensure they are from a reputable brand and the health claims are backed by research.
You might be at a risk of developing an adverse reaction to a postbiotic supplement if:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9027423
https://www.nature.com/articles/s41575-021-00440-6
https://www.nature.com/articles/d42473-020-00552-8
https://pubmed.ncbi.nlm.nih.gov/32024037
https://www.healthline.com/nutrition/postbiotics
Magical black powder or just a placebo effect? Activated charcoal is a new-fangled treatment that claims to alleviate stomach bugs. Its popularity is exploding as a potential fix for various health issues. Since there's a lot of misinformation on the benefits of activated charcoal, it's essential to stay informed on its mode of action and make sense of all the data available on its efficacy. Read on to understand the usage, benefits, and risks of using activated charcoal for stomach bugs.
Stomach bugs, known as viral gastroenteritis, are intestinal infections that cause watery diarrhea, abdominal cramps, nausea, vomiting, and sometimes fever.
While generally not severe in healthy individuals, they can pose risks to infants, older adults, and those with compromised immune systems.
Now, let's talk about the causes of stomach bugs. The primary transmission routes for stomach bugs are:
Additionally, viruses can trigger stomach bugs.
Some countries, including the United States, offer vaccines to prevent viral gastroenteritis infections.
Since there's no specific cure for stomach bugs, prevention is crucial. Key preventive measures include:
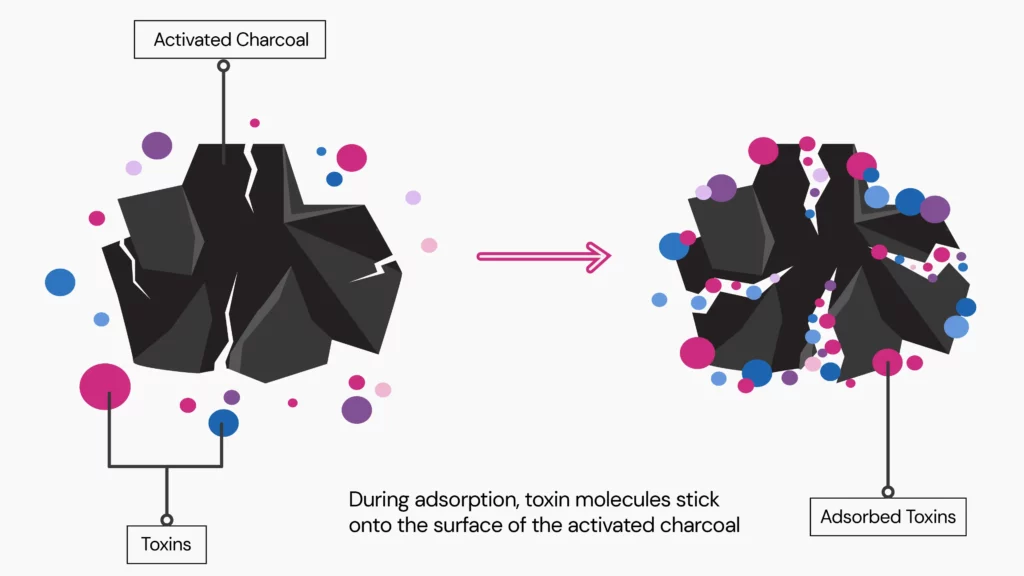
Activated charcoal functions through a process known as adsorption.
It attracts and binds substances in your digestive tract, preventing them from being absorbed.
This property makes it useful in medical emergencies, such as accidental poisoning, where medical professionals use it to trap excess drugs and mitigate potential toxicity.
However, activated charcoal's role is less evident in the context of stomach bugs.
While it may bind excess fluids and potentially alleviate diarrhea symptoms by hardening stools, it does not address the underlying cause.
Activated charcoal cannot eliminate the viruses, bacteria, or parasites that typically cause stomach bugs.
Activated charcoal is not a treatment or preventative strategy for stomach bugs.
Activated charcoal can adsorb toxins, but viruses, bacteria, or parasites cause the disease.
While some limited evidence shows that charcoal may help with diarrhea, a frequent symptom of stomach infections, its overall effectiveness remains to be determined.
Some studies suggest using it to control diarrhea in palliative care, but its benefits need further research.
Most stomach bugs disappear on their own within a few days.
Relaxation and enough water intake are the most effective strategies for acquiring fluids and electrolytes lost due to vomiting or diarrhea.
Doctors don't recommend activated charcoal to treat a stomach virus.
This condition does not respond to activated charcoal because it lacks antiviral, antibacterial, or antiparasitic properties.
Scientific evidence supporting its effectiveness against the stomach virus is limited.
Therefore, it's generally advised not to use activated charcoal for stomach viruses.
Activated charcoal can help with gut bacteria, particularly in cases of diarrhea resulting from bacterial infections.
A 2017 study highlights activated charcoal's ability to attract and expel ingested toxins from the gastrointestinal tract, like harmful bacteria whose toxins cause diarrhea.
Activated charcoal adsorbs these substances on its surface and prevents them from being absorbed into the body, thus helping to manage diarrhea symptoms.
However, while it shows promise, more research is required to fully understand its effectiveness and potential benefits in managing gut bacteria-related conditions.
| Age Group | Dosage (grams) |
| Children <1 year | 10g to 25g |
| Children 1 - 12 years | 25g to 50g |
| Teenagers and Adults | 25g to 100g |
Yes, there are risks with taking activated charcoal for stomach bugs.
Inhaling charcoal can cause side effects like vomiting, bowel blockages, and aspiration pneumonitis.
Aspiration pneumonitis is a severe lung problem that can make breathing hard.
People at higher risk for these side effects include those who:
Giving activated charcoal to an unconscious person is also risky.
It can cause vomiting, which could lead to choking.
If someone with vomiting and diarrhea becomes unconscious, it is a medical emergency.
So, while activated charcoal can help with stomach bugs, it's essential to talk to a doctor first to avoid these risks.
Activated charcoal is not suitable for everyone.
Doctors advise against using activated charcoal for patients with an unprotected airway, particularly those who are barely conscious.
It could cause severe breathing problems or even death from accidental inhalation (aspiration).
Here are the conditions under which you should avoid activated charcoal:
It's best to have your doctor monitor you in these conditions.
Hand-picked Article For You: Five Herbal Teas That Could Soothe Your Gut Instantly
Activated charcoal can be helpful in certain situations, but using it safely and correctly is crucial.
Here are some precautions to keep in mind when using activated charcoal:
Call poison control or a healthcare professional immediately if poisoning occurs.
For treating poisoning, the recommended dosage is:
For multiple doses, after the initial dose, the recommended amounts are:
Always seek professional advice before using activated charcoal.
https://www.mayoclinic.org/diseases-conditions/viral-gastroenteritis/symptoms-causes/syc-20378847
https://www.webmd.com/vitamins-and-supplements/activated-charcoal-uses-risks
https://www.medicalnewstoday.com/articles/activated-charcoal-for-a-stomach-bug
https://pubmed.ncbi.nlm.nih.gov/29231746
https://www.niddk.nih.gov/health-information/digestive-diseases/viral-gastroenteritis/treatment
https://www.healthline.com/health/activated-charcoal-gastroenteritis
https://www.tandfonline.com/doi/full/10.1080/03007995.2017.1416345
https://www.mayoclinic.org/drugs-supplements/charcoal-activated-oral-route/proper-use/drg-20070087
Have you taken an ancestry test with 23andMe, AncestryDNA, or other companies? Then, you're already on the path to unlocking the incredible insights within your raw DNA data. This article delves into the world of DNA raw data analysis, guiding you through the tools to help decode the secrets hidden within your genes. Are you ready to discover the best platform to upload raw DNA data? Join us as we explore the top 10 tools that can help you get the best out of your raw DNA!
Your DNA is a complex instruction manual written using only four letters: A, T, G, and C.
Each human has a unique manual of their own.
These manuals are 99.99% similar across humans, but the 0.01% can make a big difference.
For instance, some people could have an A in a spot where a C should be instead.
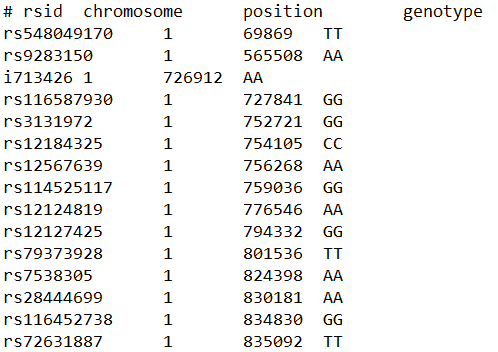
A raw data file from companies like 23andMe or AncestryDNA digitally tabulates these differences, which are called single-nucleotide polymorphisms (SNPs).
Here’s a small example of what data might look like in a raw DNA file:
| SNP | Chromosome | Position | Genotype |
| rs123456 | 1 | 12345678 | AT |
| rs789101 | 2 | 910112132 | GT |
| rs445566 | 3 | 98765432 | CG |
Raw data contains a list of variant loci on your DNA called SNPs. Scientists and researchers can use this raw data to study and learn more about genetics, human ancestry, and even some health conditions.
They can compare your genetic markers with those of others to find patterns and make connections.
SNPs are little tweaks to your DNA that make you unique. While 99.99% of your DNA is the same as everyone else’s, it’s that 0.01% that makes all the difference.
SNPs can also tell you about your ancestral roots. They help trace where your ancestors came from and how they migrated for thousands of years. That’s how companies like 23andMe can tell you you’re 30% Irish or 10% Native American.
Certain SNPs have links to health conditions. For instance, a specific SNP could increase your risk for conditions like heart disease, diabetes, or certain cancers. An awareness of your risk for health conditions can help you take the necessary preventive measures or get screened early.
Your SNPs can offer insights into how your body responds to different exercise plans or diets. You can optimize your workout routine and nutrition plan based on what works best for your genetic profile.
It’s important to remember that raw DNA data is a blueprint of your genetic information.
It can reveal sensitive personal details, and you should handle it carefully.
Only share it with trusted sites that maintain your privacy and data security.
We’re here to help you with just that!
The DNA data file from genealogical tests has information on around 700,000 SNPs in your DNA.
The portions of DNA close to each other (markers) are often passed down together.
Genetic ancestry tests use these markers to track your lineage and report ancestry and ethnicity.
They compare your DNA data with that of millions of other people and find regions of similarity.
The more the similarity, the more closely you are related to that person.
However, this information is only a drop of water compared to the ocean of information you can get from your DNA raw data file.
There are many third-party tools and DNA upload sites that interpret your DNA raw data for you.
Some of the well-known DNA raw data analysis tools are Xcode Life, Genome, Stratagene, and GEDMatch.
Note: Most of these companies accept only genotyping raw data (like the ones from 23andMe and AncestryDNA).
Analyzing your DNA raw data can tell you much about your health and wellness.
You can get insights into your:
Learning so much about yourself has never been this simple.
Many third-party companies allow you to upload your DNA raw data to provide easy-to-understand genetic reports on health and wellness.
| Tool | Price | Categories covered |
| Xcode Life - the highest number of reports - 3000+ markers analyzed - 750 + traits covered | Starting at $30 (Free reports available with pack products) | Nutrition Fitness Allergy Skin Health Sleep Personality BRCA and Breast Cancer MTHFR and Methylation Personalized Medicine Caffeine (free) |
| Promethease | $12 | Basic health and reports |
| Genetic Genie | Free; Option for voluntary donation starting from $5. | Only methylation and detox analysis |
| GEDMatch | 3 free tools, 45+ premium tools. | Ancestry. Mainly for family matches using combined 23andMe, Ancestry DNA, Family Tree DNA databases. |
| Genomelink | Free (~100 traits); $14 monthly subscription for 312 traits | Nutrition, personality, intelligence, physical, and sports traits |
| SelfDecode | 1 free report; $278-$695 and $99 annual memebership fee | Nutrition, fitness, and health |
| MyTrue Ancestry | Basic version is free.; Membership costs up to $596 | Ancestry reports only |
| Genomapp | 3 reports are free; Other reports cost up to $25 | Health conditions and precision medicine |
| Livewello | 1 free trait; Up to $25/month subscription | Nutrition and Precision Medicine |
| Strategene | $95, only one report | Metabolic pathway information |
| Enlis Genomics | 1 free report; Other reports up to $80 | Scientific health reports only |
| Nutrahacker | 1 free report, other reports up to $145 | Genetic traits, nutrition, metabolism, fitness, lactation etc |
| DNAFit/Circle DNA | 5 bundle reports ($379) | Fitness, medicine, skin, mental health, maternal health etc |
Happy choosing!
Xcode Life is a global genetics and bioinformatics company that analyzes raw DNA data files from companies like 23andMe, AncestryDNA, FTDNA, MyHeritage, and LivingDNA.
Xcode provides a variety of expertly curated reports, starting at just $20.
The reports contain specific, helpful recommendations for people with the same genetic type.
They are delivered within 24 hours.
Report interpretation assistance is also available upon request.
Xcode provides bundle options, consolidating over 1000 traits into a single analysis report.
Professional practitioners such as physicians, surgeons, nutritionists, sports trainers, chiropractors, and more use Xcode for their raw DNA data analysis needs.
Get your 23andMe raw data analyzed here.
Promethease is a software program that was developed by SNPedia to perform raw data analysis.
It uses your 23andMe raw data to generate disease-based reports.
They charge $12 per report.
It’s important to note that Promethease reports may be overly technical for most users, who usually don’t have expert knowledge of polymorphisms and biostatistics.
The system is based on literature search and retrieval.
It builds a report based on the SNPedia database against the raw DNA data from sites like AncestryDNA, 23AndMe, or FamilyTreeDNA.
The reports primarily contain information about health and precision medicine.
For instance, the report can mention your genetic risk for diseases like Alzheimer’s.
Though it is a popular service, its scientific integrity is often questioned due to its reliance on SNPedia, an open-source service.
Promethease was originally offered free of charge. However, MyHeritage acquired the DNA analysis service in 2019.
They maintain SNPedia as a free resource for academic and non-profit users.
Non-European users’ DNA raw data was shifted into new accounts on MyHeritage.
Users retain ownership of their DNA raw data file and may delete their data from MyHeritage’s server at their discretion.
Genetic Genie provides free methylation and detox reports.
This tool uses your DNA raw data from companies like 23andMe and AncestryDNA to perform methylation analysis.
The site also provides a tool for a detox analysis that looks for defects in the cytochrome P450 detox enzymes.
Incorrect methylation leads to a wide range of serious medical conditions.
This makes the methylation profile offered by Genetic Genie a good report.
The following genes are included in Genetic Genie’s Methylation panel:
14 markers in these genes are reported in the panel.
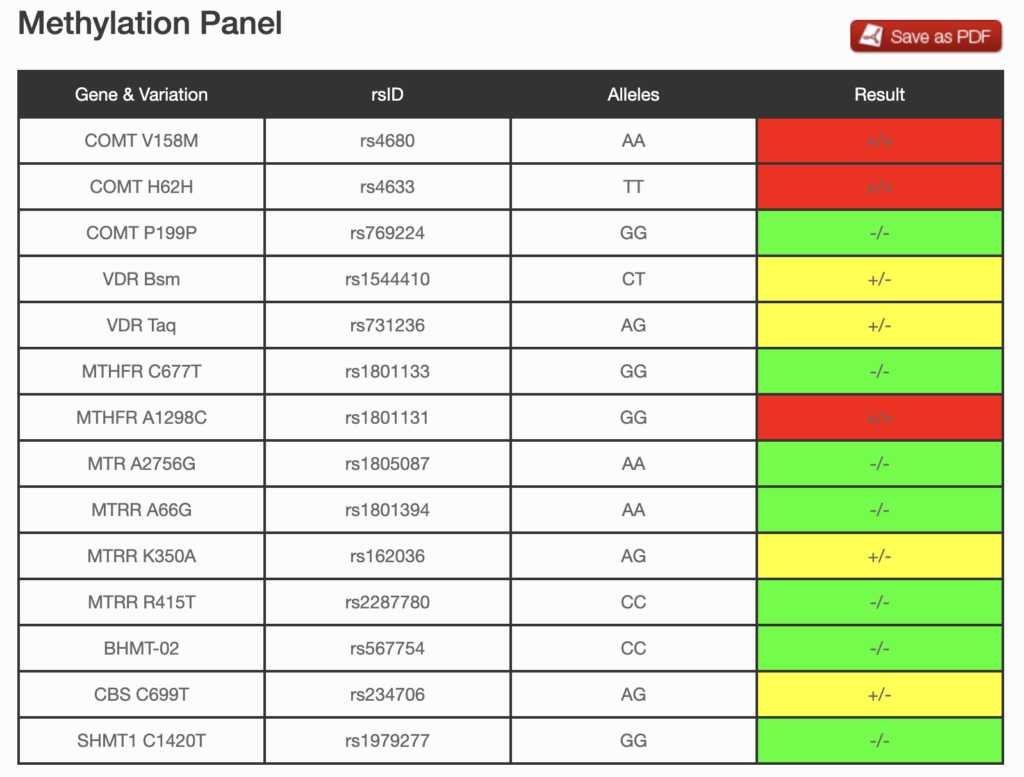
The detox profile looks at single nucleotide polymorphisms (SNPs) in genes that affect the detoxification pathway of the body.
The following genes are included in Genetic Genie’s Detox panel:
22 markers in these genes are reported in the panel.
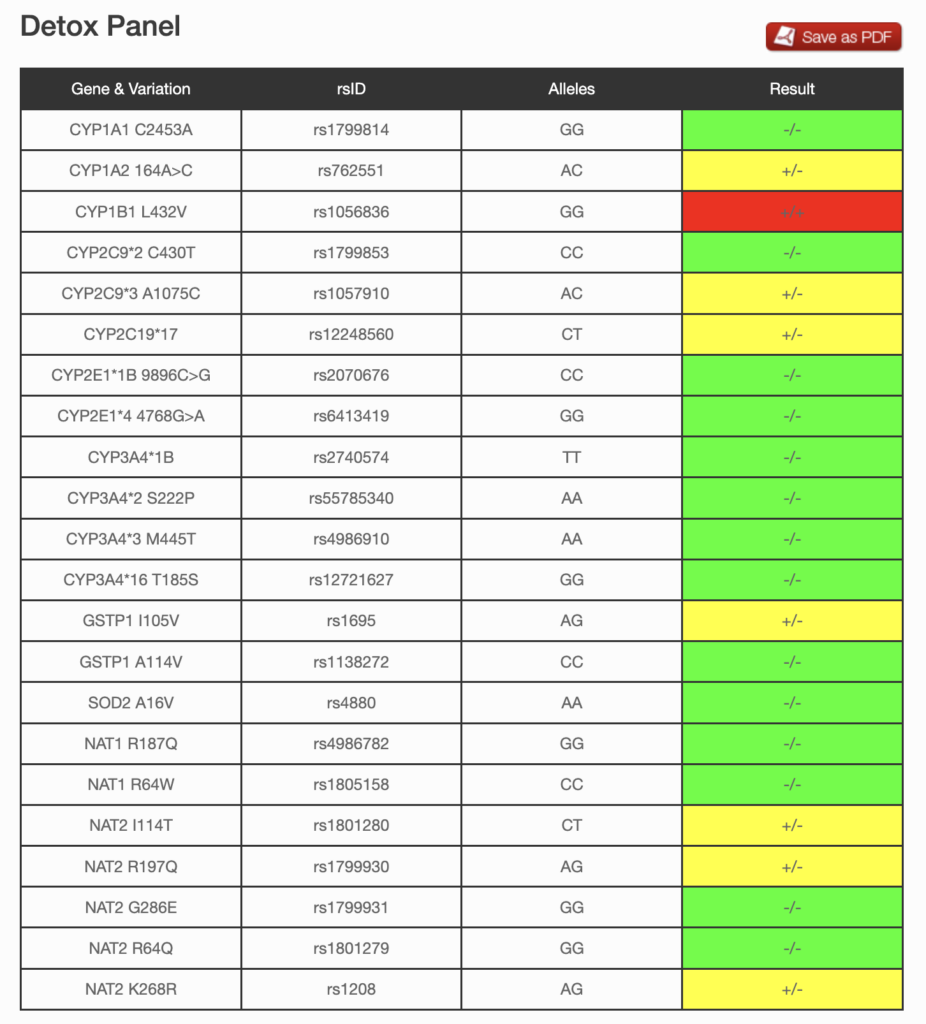
This is a free service, but a voluntary donation starting from $5 is accepted.
MTHFR Report: Xcode Life vs. Genetic Genie - In-depth Analysis
GEDMatch is a platform that helps understand your lineage via raw DNA files from genealogy companies.
The service is free, but the user experience can seem challenging for users who need to be used to exploring genetic data to understand the reports.
GEDmatch provides a range of complimentary tools and a selection of more advanced features that require a paid subscription.
You can log in to your GEDmatch account in 4 simple steps:
If you forgot your password, you can reset it with this link
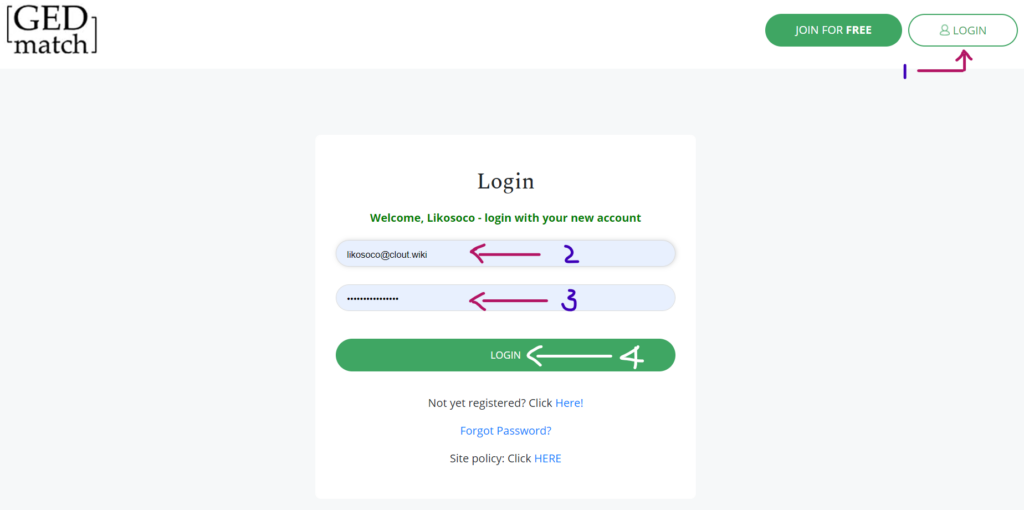
Once you create your account, you can upload your raw DNA data here.
On the upload page, you’ll need to enter the following details:
Once the upload is successful, you should be assigned a kit number.
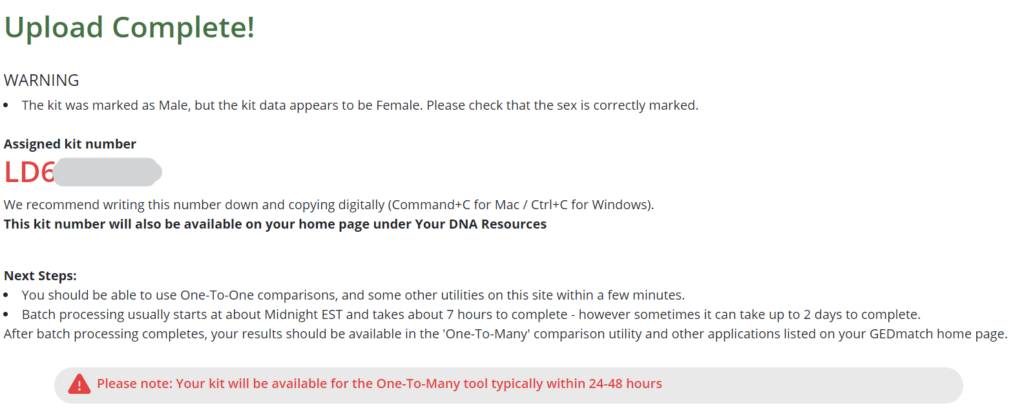
GEDmatch provides three free tools:
Purchasing a Tier 1 membership at $10 per month unlocks access to:
Various online genealogy groups recommend the GEDmatch tool.
Interestingly, GEDmatch helped law enforcement to arrest the Golden State Killer, responsible for more than 50 rapes and at least 13 murders in the 1970s and 80s.
Ever since then, GEDmatch has gained popularity as a crime-solving tool.
Read an in-depth review of GEDMatch here.
Genomelink lets users upload raw DNA data from 23andMe, Ancestry, or MyHeritage.
The site can also connect directly to their accounts on these websites to retrieve their DNA data.
Users who upload DNA data will receive a free report on 100 traits immediately.
However, to unlock more traits, you’ll need a subscription to their website for $14/month, which may not be cost-effective.
If you sign up, all your reports will be consolidated and presented in your dashboard, which you can only access online.
It’s important to note that downloadable PDF reports are unavailable from Genomelink.
A feedback option near each trait can help you review how accurate the trait results are.
Overall, they provide over 352 traits across 20 reports.
Most of these reports are genealogical and focused on revealing ancestry.
Their website does not advertise bundled reports anymore.
The actual prices of each report remain concealed until a user creates an account with Genomelink.
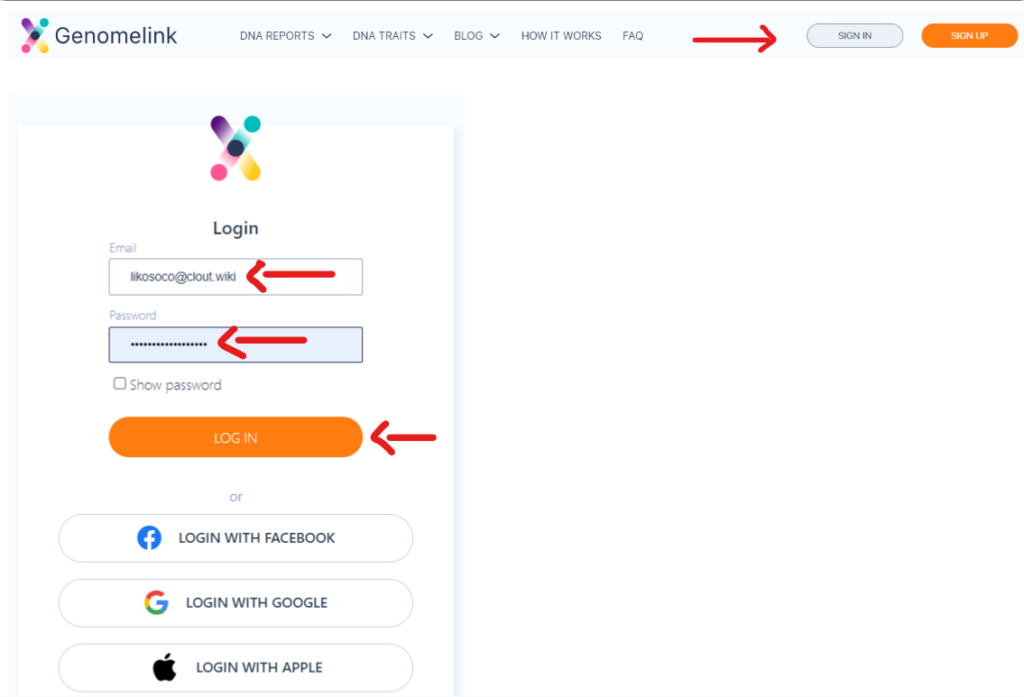
Follow these steps to log in to your Genomelink account:
Genomelink can be a good, cost-free place to start if you are new to genetic tests.
The results are moderately user-friendly and readable.
They seem to have in-depth information on privacy and the use of users’ data.
The free version of Genomelink is worth a try.
However, think twice before purchasing a subscription.
The primary benefit of the subscription is that Genomelink emails you one trait result each week.
The report bundles are overpriced for the number of traits they cover.
Although the sample reports look visually appealing, the web-based reports could tell a different story.
Genomelink Traits and Reports – A Comprehensive Review [2025]
SelfDecode offers personalized DNA testing and provides health and wellness reports by analyzing your genetic data.
It also offers genome analysis with a personalized genetics blog that helps you understand your DNA results.
Once you create a SelfDecode account, you can upload your raw DNA data.
A free report for a few traits is generated within a couple of hours.
The annual membership subscription fee for SelfDecode is $99.
Depending on the services you’re interested in and whether or not you already have a raw DNA file, the total upfront payment can range from $298 to $695.
After that, you will be billed a $99 fee annually.
SelfDecode Review: What You Should Know Before Buying
Livewello accepts raw data files from 23andMe, AncestryDNA, Family Tree DNA, and Gene By Gene.
It offers 15 genetic reports and 160 health reports. However, the range of these reports is much smaller, with only a few SNPs studied per report.
Some of the reports include:
You can create an account for free, but reports require a membership.
Livewello’s payment plans range from $6.95 to $25 monthly or $75 to $215 yearly, with progressively better amenities.
A DNA kit may be purchased for $165 if required.
Livewello offers 20 reports. Some of them include:
StrateGene initially offered a $295 DNA kit as the only sample collection model.
Now, they have switched to a virtual DNA data upload model.
You can upload your DNA raw data files from 23andMe to StrateGene.
They offer one report, priced at $95, with information on nine essential processes in your body, including pathways for:
Users find the reports too complex to be of actual use.
Strategene may not be the best choice for those who prefer easily understandable results and readily implementable recommendations.
This 23andMe raw data analysis service provider is more for educational than direct consumer purposes.
Their service caters to research scientists.
They analyze DNA data to find health risks associated with specific genetic variants.
The initial intention of developing this software is to allow researchers to analyze whole genome files.
They have also added a software program for personal use and a free genome report accessible directly from their site.
While the service is free, understanding and interpreting the report takes a reasonable amount of scientific knowledge.
Nutrahacker accepts raw DNA data from 23andMe, AncestryDNA, tellmeGen, or MyHeritage.
Upon registering with your details and uploading your raw DNA data, you can access a ‘Genotype Imputation’ report for free.
NutraHacker offers eight other genetic reports, including:
They advertise two bundle packs, a Detox and PharmaShield panel($300/year) and the WGS Critical Genetics panel ($395 one-time).
DNAFit now redirects to CircleDNA. They offer five categories of analyses, including:
Each of these reports costs $379 and includes collection kits.
A children’s DNA kit is available for $299 as well.
The report is available online.
Initially, the information feels overwhelming.
However, the reports do have reasonably relevant background information.
The reports comprehensively include a list of the genes analyzed in the test and information about each gene.
If you are a hardcore athlete, consider CircleDNA.
Before you buy, check out our comparative blog on the top 5 DNA fitness report providers.
According to DNA Testing Choice, a popular genetic testing company review website, their privacy policy contains clauses regarding how DNAFit could pass on user data to third parties for research with or without client consent.
Lifenome accepts DNA raw data files from 23andMe, AncestryDNA, and FamilyTreeDNA.
They offer reports on the following traits:
The reports are comprehensive and easy to understand, with clear implications and recommendations.
The site does not clearly indicate pricing or how to purchase these reports, which could deter some users from using Lifenome’s services.
With the most reports and over 750 traits analyzed rapidly, Xcode Life is undoubtedly the best raw DNA data analysis tool in 2024.
Additionally, its website is user-friendly and compatible with 10+ DNA testing companies, including 23andMe, AncestryDNA, and FTDNA.
Xcode provides comprehensive, jargon-free, and interactive reports starting at just $20 with clear recommendations and information on each trait marker analyzed.
GenomeLink has a user-friendly website with different products that users can apply to all walks of life.
They provide a free report with over 100 traits upon account creation.
While the reports appear lucrative, it’s important to note that the rest of their reports and traits are accessible only through a $14/month subscription. Additionally, the value of their report bundles does not match their cost.
Despite this, their reports can help users understand their ancestry, curate their diets, and improve their workouts for a healthier lifestyle.
SelfDecode offers whole genome analysis, generating readable reports within a few hours.
It also offers free trait reports for a handful of markers upon account creation.
The comprehensive nature of these reports can significantly improve consumers’ knowledge of their disease risk and behavioral patterns.
Users thus remain informed and prepared on their genetic makeup.
Several genetic testing companies offer services to analyze raw DNA data and provide helpful insights about health and wellness.
Xcode Life stands out due to its affordable, comprehensive, and user-friendly genetic reports that are delivered within 24 hours.
Your raw data likely contains the following columns: RSID, chromosome, position, and genotype.
Each row analyzes the genotype of an SNP (single nucleotide polymorphism), or a mutation in your DNA, at a certain position on a specific chromosome.
Genetic testing companies like Xcode Life can decode your raw data to give you valuable information about your health and wellness for as little as $30.
While some companies may offer a couple of health-related reports for free, getting a comprehensive health report from your raw DNA can give you a clear picture of your overall wellness and possible risks.
Xcode Life offers a comprehensive Gene Health report that studies your risk for over 45 chronic conditions for just $50.
While most genetic testing companies charge over $100 for their DNA analysis services, Xcode Life offers individual reports priced between $30 and $50, with comprehensive report bundles priced between $160 and $199.
Inflammation is a complex process that, in many cases, is essential for our body's defense and healing. However, when it becomes chronic, it can lead to a host of health issues. Managing chronic inflammation requires a holistic approach, including a balanced diet, regular physical activity, and effective stress management. This guide focuses on the first pillar: nutrition. Discover how an anti-inflammatory diet can help you control inflammation and improve your overall health. We'll provide you with a comprehensive food list and meal ideas in a downloadable PDF, making it easier for you to incorporate these anti-inflammatory foods into your daily routine. Let’s dive into the ultimate guide to an anti-inflammatory diet and learn which foods to embrace and which to avoid.
Inflammation is not an enemy in typical cases. When your immune system identifies something as foreign, it triggers an inflammatory response, protecting your body against viruses and other pathogens.
However, in some cases, the inflammation continues to persist even if there's no foreign invader.
This is where inflammation is the enemy, as it can increase your risk for conditions like:
An anti-inflammatory diet focuses on consuming foods that help naturally reduce inflammation in the body while avoiding foods that can trigger or worsen inflammation.
If you have a health condition that causes chronic inflammation, consuming an anti-inflammatory diet may alleviate your symptoms.
While the anti-inflammatory diet is safe, you must consult your doctor before starting it.
An anti-inflammatory diet benefits people with conditions that are caused by or worsen due to chronic inflammation. Some of these include:
Some research also states that eating an anti-inflammatory diet may reduce the risk of cancer.
Hand-picked Article For You: Gary Brecka 30-30-30 Diet: How To Follow, Pros, And Cons
There are different types of anti-inflammatory diets, depending on the foods they recommend. Let’s take a brief look at the three most popular ones!
This diet focuses on the consumption of:
It recommends avoiding the following foods:
DASH, or the Dietary Approaches to Stop Hypertension, is similar to the Mediterranean diet, which focuses on consuming less or no salt and includes more low-fat dairy products.
This diet combines a few parts of the Mediterranean diet with the DASH diet and is considered healthy for the brain.
It may guard against Alzheimer’s disease and other forms of dementia.
The MIND diet recommends the consumption of:
Like other anti-inflammatory diets, the MIND Diet advises limiting the following foods:
| Foods to Increase | Foods to Decrease |
| Fruits and Vegetables - Berries, cherries, peppers - Sweet potato, pineapple, yellow bell pepper, squash, peaches - Dark leafy greens, Brussels sprouts, cabbage, green beans - Blueberries, blackberries, grapes, eggplant, olives, plums, purple cabbage | Proteins - Grain-fed beef - Processed meats |
| Fiber - Whole grains - Bran cereal - Nuts - Brown rice - Potato | Trans-fats - Partially hydrogenated oils - Baked goods - Fried foods |
| Proteins - Plant-based proteins (found in beans, legumes, nuts and seeds) - Grass-fed meat and fish | Saturated fats - Meats like lamb, pork, fatty beef, chicken with skin - Dairy products - Fruit juices |
| Herbs & Spices - Ginger - Turmeric - Sage - Cumin - Cloves - Cinnamon - Paprika - Tarragon | |
| Omega-3’s - Fatty fish - Fish oil - Whole grains - Walnuts *Eat more omega-3 fatty acids than omega-6 fatty acids. | |
| Monounsaturated Fatty Acids - Olive oil - Avocados | |
| Desserts/Snacks Dark chocolate containing 70% or more cocoa |
Oily or fatty fish, like sardines, salmon, trout, and herring, are rich in omega-3 fatty acids.
These fatty acids have been associated with a reduction in C-reactive protein, a key inflammation marker.
Several beverages and drinks can help reduce inflammation. Some of these include:
Omega-3 fatty acids are the most potent natural anti-inflammatory.
They are found abundantly in the following foods:
Others are reading: MTHFR Diet: What To Eat, What To Avoid For MTHFR Mutation
An anti-inflammatory diet may take a few weeks to become effective.
We must remember that an anti-inflammatory diet is not a magic pill; it can take longer than six or seven weeks to show effects.
If you are on an anti-inflammatory diet, you must limit or avoid the consumption of the following foods:
How quickly your heart rate drops after exercise speaks volumes about not just your fitness but overall well-being. Known as Cardio Recovery Rate or Heart Rate Recovery (HRR), this measurement is a key indicator of cardiovascular health. In this article, we'll dive deep into the concept of HRR, explaining why it's important, how to measure it, and what it can reveal about your heart. Whether you're a fitness enthusiast or just starting your health journey, understanding HRR can empower you to make informed decisions and track your progress effectively.
Cardio recovery rate, also known as heart rate recovery, reflects how swiftly your heart returns to its resting pace after exercise.
It's calculated by taking the difference between your peak heart rate during exercise, and your heart rate a minute after you end your workout.
This difference is typically measured in beats per minute (bpm).
Doctors utilize HRR during exercise stress tests to evaluate cardiovascular health. Generally, a quicker HRR indicates a fitter heart.
You can also track your own HRR to measure your fitness level and monitor your progress over time.
The importance of cardio recovery rate lies in its ability to reflect how effectively your heart is functioning and its potential to predict future heart-related problems.
During an exercise stress test, healthcare providers measure your HRR for several reasons:
An abnormal HRR might indicate issues with your autonomic nervous system, which regulates your heart rate and its return to normal post-exercise.
Problems with this system can increase your risk of conditions like:
Research suggests that individuals with a low HRR are more likely to suffer from heart disease and have a higher mortality risk.
HRR indicates how well your cardiovascular system functions and how fit you are.
A fast HRR means your heart is healthy and your body is fit. It efficiently delivers oxygen to your muscles during workouts and clears waste afterward.
Conversely, slow HRR might mean problems with your body's nervous system and could signal health issues like cancer, heart disease, or diabetes.
Thus, HRR signals your cardiovascular health and fitness level, showing how efficiently your body can recover after exertion.
Calculating your cardio recovery rate is simple and requires a reliable heart rate monitor and some basic math. Follow these steps:
For example, if your peak heart rate is 180 beats per minute (bpm) and your heart rate after one minute is 150 bpm, your HRR is 30 bpm (180 - 150 = 30).
Your heart rate recovery has two phases:
Using the one-minute method mainly focuses on the fast phase, which is commonly used and provides valuable insights into heart health.
Consult your doctor to find the best method and understand your ideal heart rate recovery range.
A faster heart rate drop following exercise signifies a good cardio recovery rate.
Ideally, a decrease of 18 beats per minute or more within one minute of rest indicates efficient recovery.
However, what constitutes a favorable recovery rate varies from person to person.
Factors such as existing heart conditions, age, the type of exercise performed, and the duration of rest before checking the heart rate influence this.
Remember, while HRR is informative, it's just one component in your comprehensive health assessment.
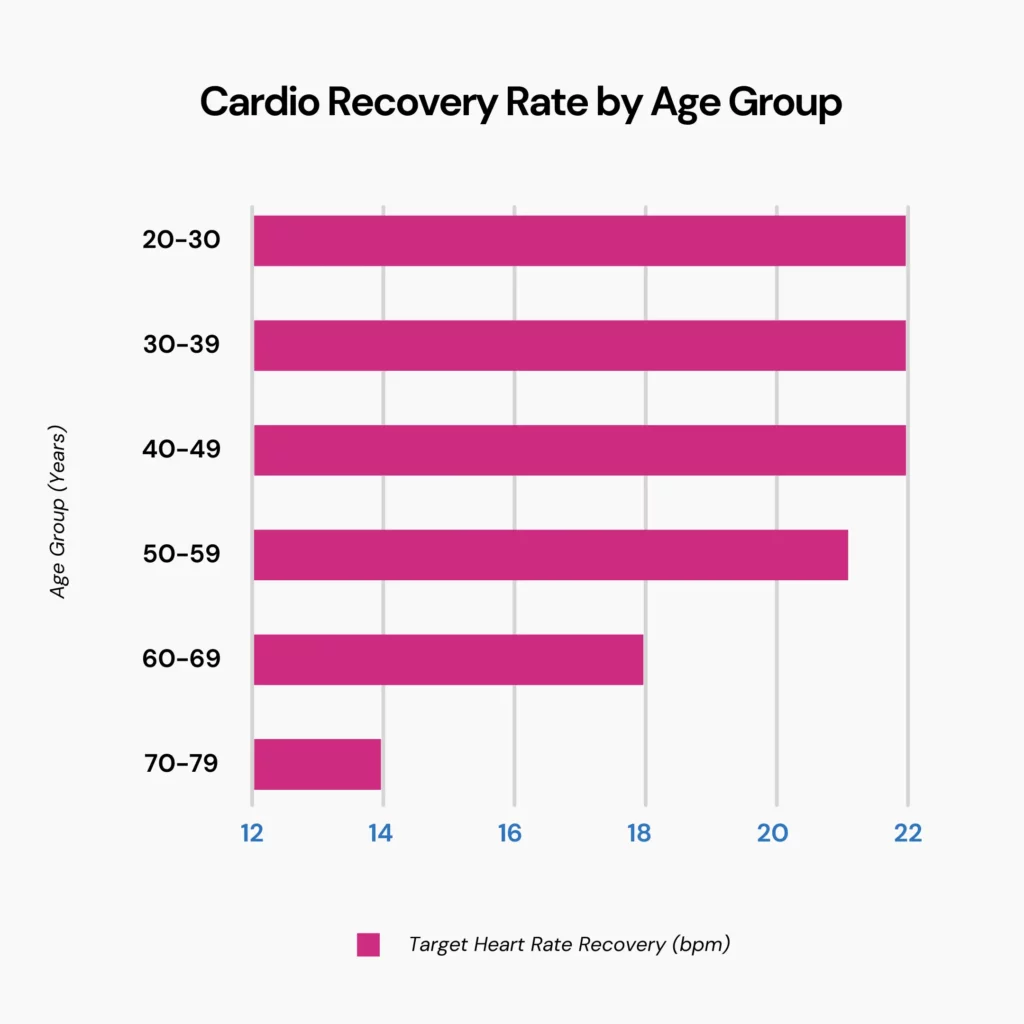
The optimal cardio recovery rate varies depending on your age. Generally, after 60 seconds of rest, a good heart rate recovery for most adults is 18 beats or higher. However, this number changes as you age:
| Age Group (in Years) | Target Heart Rate Recovery (in BPM) |
| 20 to 29 | 22 |
| 30 to 39 | 22 |
| 40-49 | 22 |
| 50-59 | 21 |
| 60-69 | 18 |
| 70-79 | 14 |
It's important to note that the intensity of your workout also affects your heart rate recovery.
During moderate activities, your heart rate typically falls between 50% and 70% of its maximum rate. It usually ranges from 70% to 85% of its maximum for vigorous activities.
So, your heart rate recovery number is based on your maximum heart rate during or at the end of your exercise, which varies depending on your age.
Beyond the previously mentioned factors, several additional influences can impact your cardio recovery rate:
Regular exercise is key to achieving a faster heart rate recovery. The best approach for beginners is to start slowly and gradually increase intensity and duration.
Specifically, focusing on cardiovascular training can really help improve your cardio recovery rate. Mixing up your cardio workouts can yield the best results. Some types include:
If you exercise regularly, it's important to consult your healthcare professional before trying a new workout routine or making any changes to your current plan.
For those with a history of heart problems, specialized cardiac rehab programs can significantly improve heart health and long-term well-being.
Other ways to improve your cardio recovery rate include:
Understanding how your heart recovers is crucial, regardless of age or heart problems. It's never too early to start taking care of your heart for the future.
Cardio Recovery Rate or HRR reflects how quickly your heart returns to its resting rate after exercise, offering insights into cardiovascular health.
A faster HRR indicates a fitter heart, while a slower recovery might warrant investigation.
You can calculate your HRR by subtracting your heart rate one minute after exercise from the peak heart rate right after you stop your exercise.
The ideal HRR varies by age, with an average of 18 bpm or higher for most adults after one minute of rest.
Factors like dehydration, caffeine intake, and fatigue can influence your HRR.
Engaging in regular cardiovascular exercises, improving sleep quality, limiting caffeine intake, and hydrating sufficiently are some effective ways to improve cardio recovery rate.
https://my.clevelandclinic.org/health/articles/23490-heart-rate-recovery
https://www.medicalnewstoday.com/articles/heart-rate-recovery
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5907593
https://www.nature.com/articles/s41598-017-14540-4
https://www.jsams.org/article/S1440-2440(15)00054-7/abstract
How much do you know about your ancestors? A dozen generations ago, where did they live? Where did they travel? Where did they end up? The answer to these questions lies in signposts from the past called haplogroups. These are markers in your DNA that can be used to turn back the clock to reveal your ancestry. They are the branches of the family tree of humanity that can retell the tales of our species’ history and hint to us how certain genetic traits could matter a lot today.
According to the International Society of Genetic Genealogy, a haplogroup is a group of people who share a common ancestor on either their patriline or matriline.
The word is a combination of haplotype and group.
Haplotypes refer to the specific DNA sequences on maternal and paternal lines frequently passed down the generations.
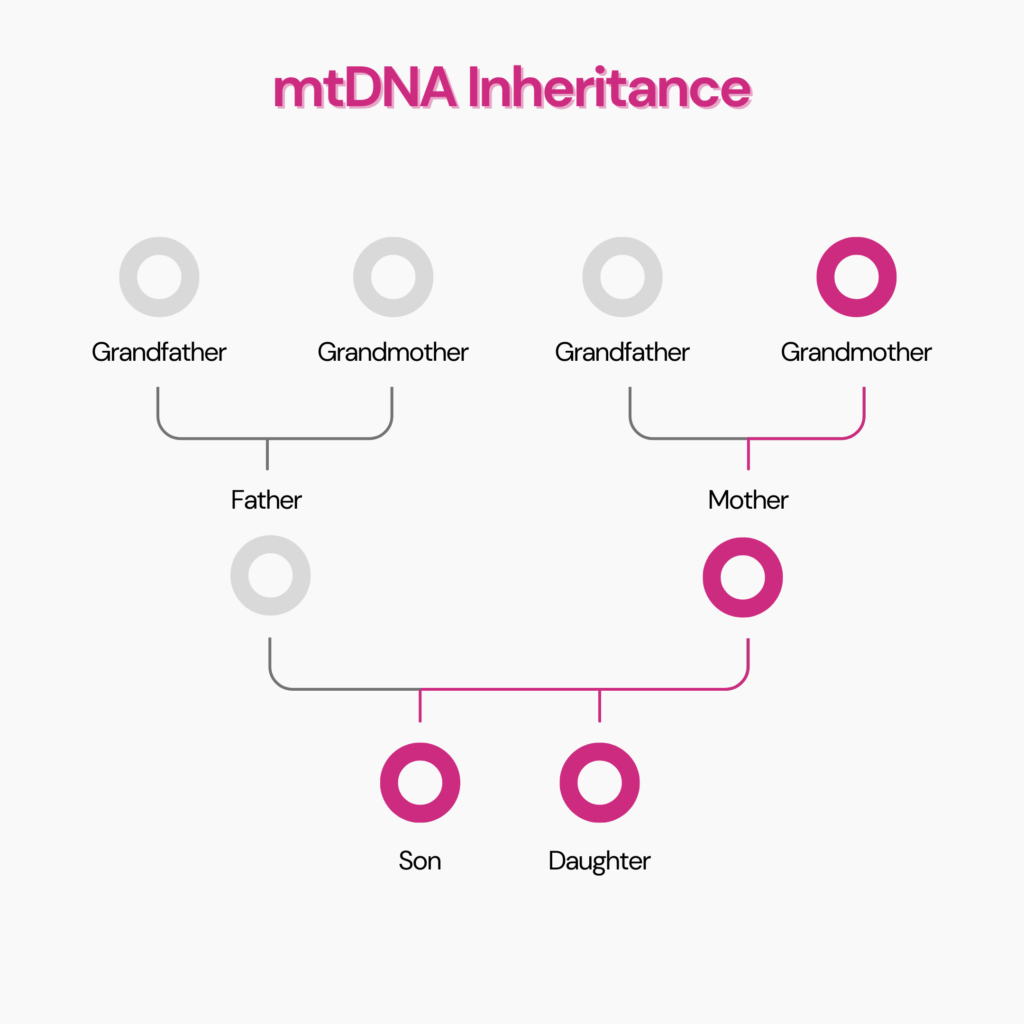
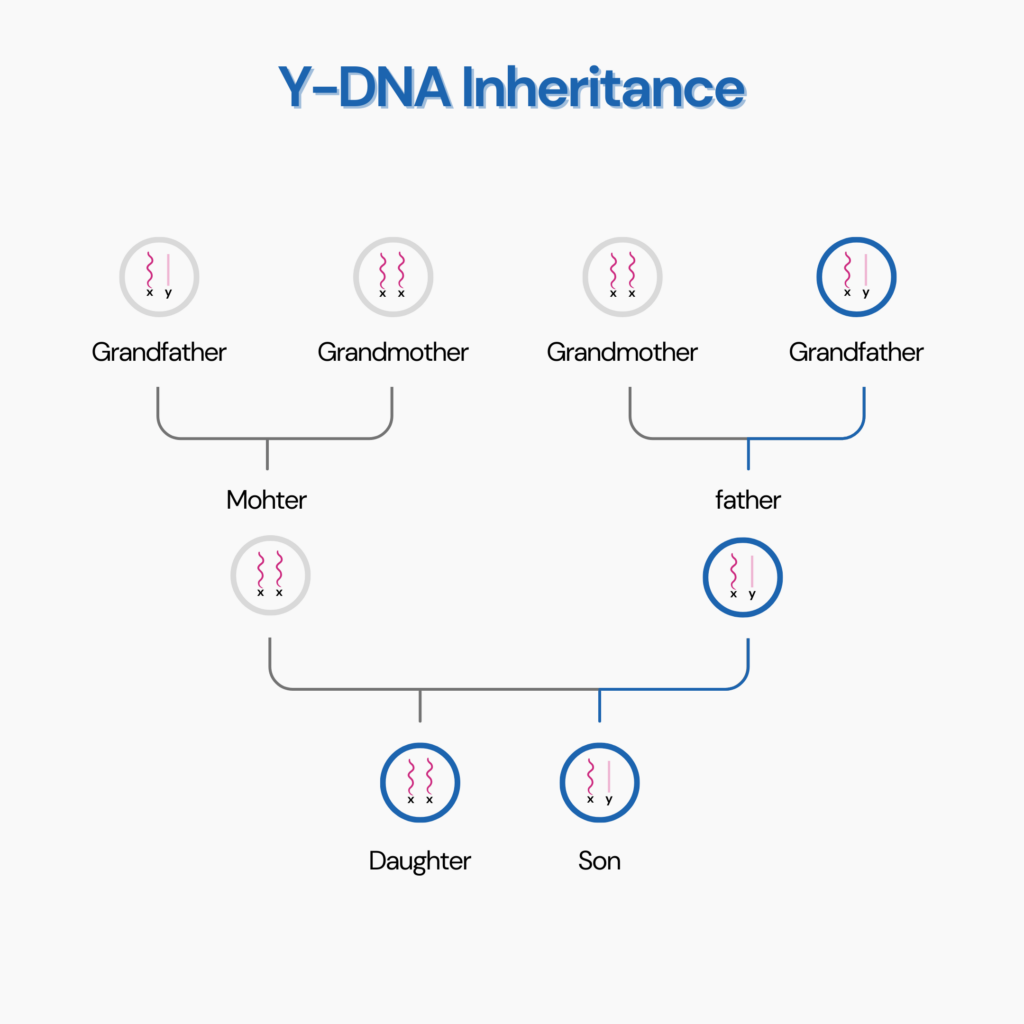
Y-DNA, on the male sex chromosome, is passed down from biological father to son, while mtDNA, or mitochondrial DNA, is passed from the biological mother to both the son and the daughter.
When these DNA sequences are mutated, it causes a split in the evolutionary group, forming a new haplogroup.
When these hereditary pieces of DNA are mutated, an evolutionary group splits off to form a haplogroup.
Each of these mutations is known as a single-nucleotide polymorphism (SNP), and every major haplogroup is associated with a certain set of SNP markers.
Not all people who share a haplogroup are genetic relatives.
Haplogroups tell you about your direct paternal or maternal ancestors.
Since the DNA mutations that define a haplogroup occurred thousands of years ago, the haplogroup would have progressively diverged over generations.
Thus, most people with the same haplogroup are not closely related today.
This also means that your genetic relatives might not be part of your haplogroup.
Did You Know?
The DNA data from your genetic ancestry test can be used to learn important things about your health, from your risk for heart disease and stroke to food intolerances and sleep disorders. You can upload your DNA data to learn 1,500+ things about your health. Learn more.
Variations in the mitochondrial DNA or mtDNA determine maternal haplogroups.
You inherit your mitochondria and the DNA in them only from your biological mother.
Mitochondrial DNA does not recombine (or merge) with other DNA since it is a unique type of DNA found outside the nucleus.
Thus, mitochondrial DNA remains practically unchanged.
It means you’re likely to share the same haplogroup with your maternal relatives, such as your sister, maternal aunt, or maternal grandmother.
The maternal haplogroup can be traced back through the generations to a specific mutation at a particular time.
MtDNA is well conserved, meaning it rarely undergoes recombination.
It has an intrinsic ability to resist degradation.
Also, mtDNA has a higher copy number than nuclear DNA, a measure of its abundance in a cell.
Each cell contains 1000 mitochondria, with 2-10 copies of DNA per mitochondrion.
Thus, the amount of mtDNA available from a sample is quite large.
The variations in the Y chromosome determine the paternal haplogroup.
The Y chromosome is a sex-determining chromosome found only in males, passed down from biological fathers to sons.
The Y chromosome is a reflection of your ancient paternal ancestry.
The Y chromosome is generally considered inert and associated with a minimal number of genetic processes and mutations.
While it does undergo recombination with the X chromosome during cell division, the actual changes are made only to the ends of the Y chromosome.
95% of the chromosome is passed down the generations without mutations.
All modern Europeans are classified into seven groups called mitochondrial haplogroups.
A set of mutations in the mitochondrial genome defines each haplogroup.
It can be traced to a specific prehistoric woman along a person’s maternal line.
In his book The Seven Daughters of Eve, Bryan Sykes refers to these women as “clan mothers.”
The clan mothers correspond to one or more human mitochondrial haplogroups:
Today, there are more than these seven haplogroups.
For example, haplogroup L is a sibling group of haplogroup T and a secondary descendant of haplogroup K.
While these clan mothers represent ancient people, a system has been devised to keep track of the most recent common ancestor (MRCA).
The MRCA is the oldest person whose direct lineage can be traced to the current generation.
The Y-chromosomal Adam is the MRCA on the paternal line.
His direct descendant is alive today and carries conserved fragments of the MRCA’s Y chromosome.
Similarly, the Mt-chromosomal Eve is the MRCA on the maternal line.
It’s not a given that they are related or even each other’s contemporaries since the data available reduces drastically as we go back generations.
Estimates of when the chromosomal Adam and mitochondrial Eve lived can vary and will shift as newer information about SNP markers becomes available.
The oldest haplogroups are from Africa, the cradle of life.
According to paleontological records, Homo sapiens began to migrate from Africa 60-70,000 years ago.
They moved to the Eurasian continent from Africa, and some reached the Indian coast.
Some migrants reached the Indian coast through Southeast Asia.
They then moved to Australia around 50,000 years ago.
Since then, humans have followed different migratory routes and spread worldwide.
We can better understand and trace these migratory routes by defining the mutation in Y DNA and mtDNA.
This table depicts the most common maternal and paternal haplogroups in different parts of the world today.
| Region | MtDNA Haplogroup | YDNA Haplogroup |
| Europe | H (40% of population) | R1 |
| Central and Northern Asia | H | R1a and C3 |
| Africa | L1, L2 and L3 (most common) | C and A |
Haplogroups can identify the genetic lineage of a person.
It can also identify the early migration routes of human beings.
Sometimes, there are specific diseases found in certain populations.
These diseases can be traced back to a mutation in the Y chromosome or the mitochondrial DNA.
Testing for such mutations during haplogroup studies can help us treat these disorders better.
Dawn Says
I have been struggling for years searching for answers for health issues I have been having. Sending in my DNA to getting the results took less then 24hours. So simple, most importantly I may now have the answers I have been seeking all this time. Will definitely keep spreading the word. There is way to many people that could truly benefit from this. Read More Reviews.
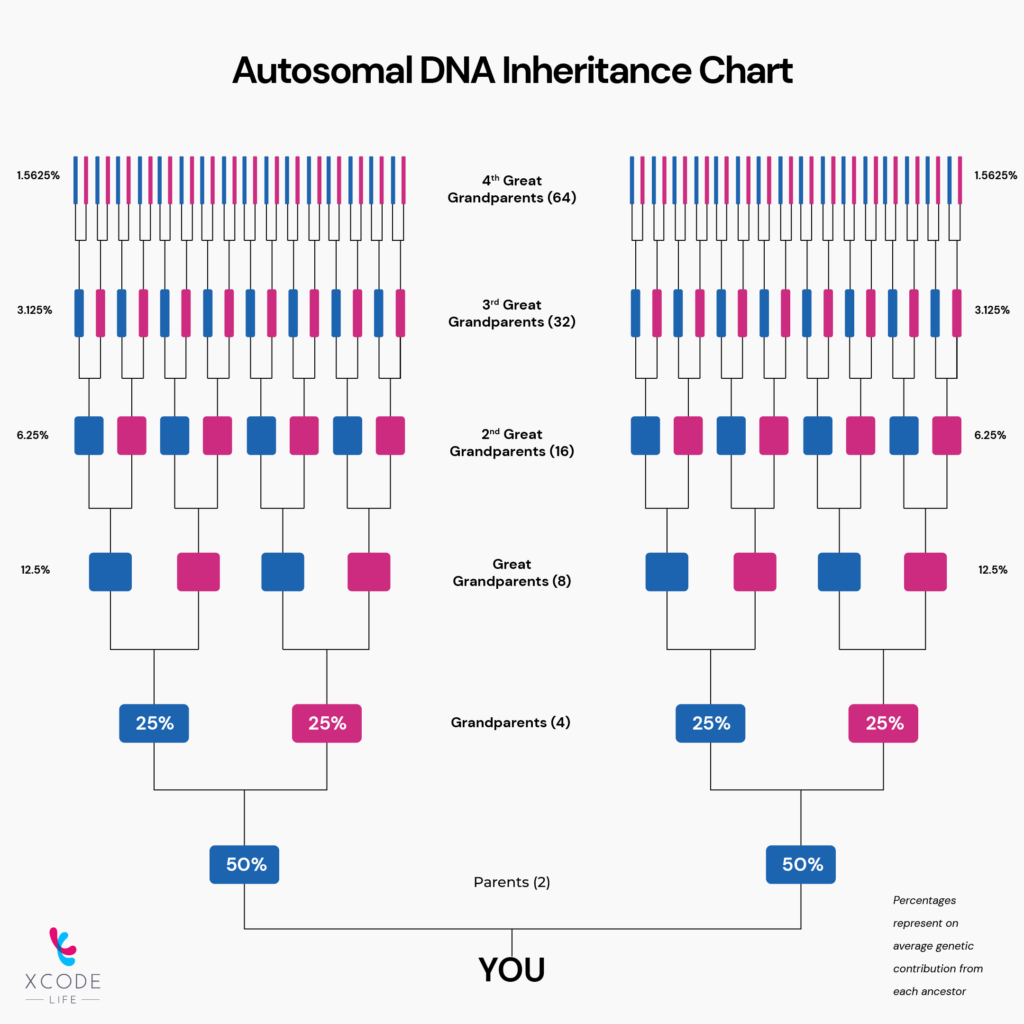
Autosomal DNA from your numbered chromosomes makes up the majority of your genome.
It undergoes recombination as part of cell division, a process that naturally causes some mutations with each generation.
Consequently, analyzing autosomal DNA can only reveal your recent ancestry within ten generations.
On the other hand, haplogroups from your allosomal DNA on the X and Y chromosomes are a window into the far reaches of your ancestral line.
Thus, testing for your haplogroup could show different results than testing your autosomal DNA.
The Y chromosome or the mitochondrial DNA can undergo small mutations, what researchers call SNPs.
SNPs and their prevalence are tested to identify haplogroups in a person.
Identifying the haplogroup will help determine your ancestral relatives on your father or mother’s side, tracing your heritage back to the chromosomal Adam or the mitochondrial Eve.
A Short Tandem Repeat (STR) analysis can determine a person’s haplogroup.
This works by comparing a known mutated segment of DNA across regions that are likely to have been mutated.
Since certain mutations are specific to certain lineages, a person’s haplogroup can be estimated through STR.
However, only a Y SNP test can confirm a person’s haplogroup.
It covers an SNP-rich region of the Y chromosome and accurately compiles a report of all its unique SNPs.
Testing for SNPs in the Y chromosome can help us identify a person’s haplogroup.
Since women don’t have the Y chromosome, they can test their mtDNA to identify their haplogroup.
A male relative on her mother’s side can be tested if a woman wants to identify her Y DNA haplogroup.
Upload Your DNA data for 1000+ health & wellness insights
While the most pertinent outcome of a haplogroup study is the migration patterns of your ancestors, knowing your haplogroup can tell you more than you might think.
Haplogroup analysis is particularly helpful in tracking the emergence and spread of diseases we deal with today.
Diseases found in specific populations, like Parkinson’s or Alzheimer’s, can be traced to a mutation in YDNA or mitochondrial DNA in a specific haplogroup.
Studying the nature of the mutation can help scientists combat the disease better today.
Understanding your haplogroup can give you an idea of the diseases you’re susceptible to, the traits you carry from your ancestors, and what you can expect to see in your children and future generations.
Due to a significant occurrence in Scandinavian regions like Norway and Sweden, the haplogroup Y-R1a1 is considered a marker of Viking heritage that spread towards Britain during a migratory period.
Haplogroup analysis is robust enough to study the genealogy of even ancient historical figures. An analysis of King Tut’s DNA showed that his DNA belonged to the haplogroup R1b1a2, which is predominant in half of European men today.
The haplogroup D4h3a is the least predominant in the world today. It can be found only in a few indigenous populations in South America, comprising less than 0.01% of the population.
Other accounts say that the Y-K2a haplogroup is the smallest, with only two people in the entire world carrying its DNA.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5793196/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC379119/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6562384/
https://www.sciencedirect.com/science/article/abs/pii/B9781455707379000321