About 75% of Americans drink morning coffee, and nearly half of them are regular drinkers.
One cup of coffee (8 oz) contains 95 mg of caffeine.
For decades, people have believed that caffeine in their coffee made them feel alert and energetic.
Researchers now think otherwise.
On comparing the neurological effects of coffee vs. caffeine, researchers have reported that coffee and not caffeine led to increased brain activity and cognitive functioning.
If so, where does this leave caffeine at? Keep reading to learn more about this study.
The relationship between the CYP1A2 gene and caffeine is a two-way street. The gene affects how you metabolize caffeine. At the same time, your caffeine consumption habit influences the activity of this gene. Knowing your CYP1A2 gene status can help you learn about your ideal caffeine consumption.
Caffeine is a natural bitter substance found in more than 60 types of plant sources.
A few of the most common sources of caffeine are:
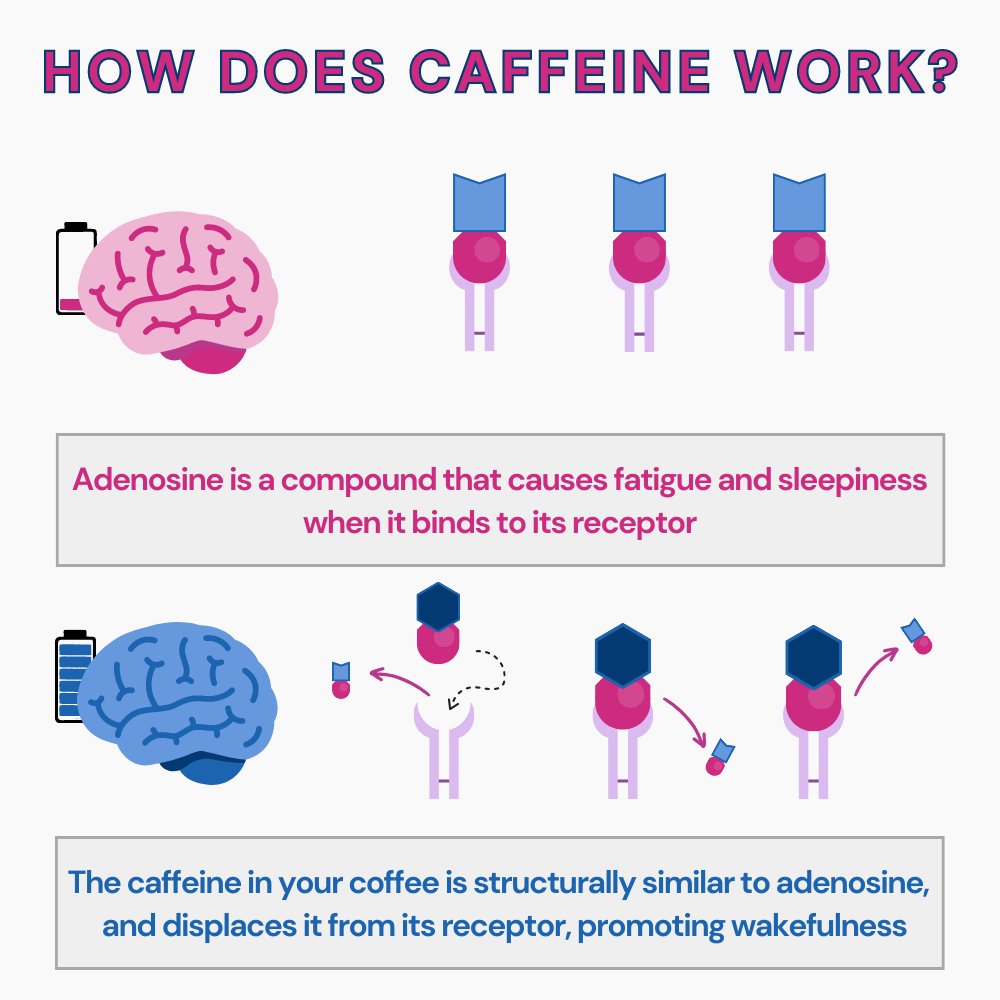
Caffeine is a known stimulant of the Central Nervous System (CNS).
This substance activates the noradrenaline neurons in the CNS and encourages dopamine release.
Dopamine is a neurotransmitter that makes people focused, happy, energetic, and alert.
This is why most people drink morning coffee first thing in the day.
They feel the cup of coffee improves wakefulness.
Coffee is made by roasting, grinding, and brewing coffee beans.
It contains multiple compounds that affect the human body and mind, including the following:
Caffeine is the most commonly used drug worldwide.
One cup (240 g) of coffee contains about 96 mg of caffeine.
The average caffeine consumption in the United States is 200 mg/day.
Adults consume caffeine in the form of coffee and caffeinated beverages.
While low to moderate caffeine consumption is safe and beneficial, very high doses of caffeine can lead to cardiovascular problems.
Caffeine abuse can lead to a condition called Caffeine Dependence Syndrome.
This is marked by behavioral, psychological, and cognitive changes in the person.
For a long time now, it has been believed that the caffeine in coffee gives people an energy boost, focus, and other mental changes.
However, a 2023 study published in the Frontiers in Behavioral Neuroscience reports that some of these changes could be an imaginary sensory effect of drinking morning coffee and unrelated to caffeine intake.
Coffee brings various physical and mental changes to the body.
Not all of these changes are recorded or explained.
A group of researchers conducted Functional Magnetic Resonance Imaging (fMRI) on habitual coffee drinkers to understand the neurobiological impact of the drink.
Two groups of participants were a part of this study.
Coffee group - 47 individuals with an average age of 30
Caffeine group - 36 individuals with an average age of 32.1
The fMRIs of the study participants analyzed changes in the Default Mode Network (DMN), the higher visual network, and the Right executive control network (RECN).
DMN is a group of brain areas that activate when the person is not focused on what’s happening around them.
The DMN system has been associated with various mental health conditions like depression and anxiety.
The RECN is responsible for the brain's information manipulation, decision-making, and problem-solving capabilities.
Higher visual networks of the brain are areas associated with complex visual response processes.
The study observed interesting differences in the fMRIs of the coffee and caffeine groups.
The fMRI data of coffee drinkers reveal the following.
One of the interesting observations of the study was the effect of caffeine and coffee on the posterior DMN connectivities, especially in the precuneus region.
Precuneus is associated with tasks like self-consciousness, cue reactivity, integration of information, and memory retrieval.
The decreased nodal connectivity in the precuneus region could be why people experience higher preparedness from rest to action mode.
Another interesting observation was the decreased functional connectivity between the motor networks and prefrontal cortex after consuming coffee and caffeine.
According to these researchers, this connectivity trend could be a reason for increased preparedness for action in coffee drinkers.
A stark difference in the fMRI of coffee and caffeine drinkers was that only coffee drinkers experienced increased connectivity in the higher visual and RECN networks.
This increase wasn’t noticed in the caffeine group.
According to these experts, other components of coffee could be causing higher connectivity in executive control and visual imagery.
These experts feel that an imaginary sensation could trigger the pleasure responses in coffee drinkers.
This imaginary sensation has nothing to do with the already established neurochemical responses.
It is, instead, associated with the sensory experiences of sipping a cup of coffee.
This study concludes that coffee's effects, like alertness to external stimuli and being prepared for action, could all result from other complex compounds in the drink and not due to caffeine.
These researchers report two different responses to coffee in the brain - the neurochemical effects of caffeine in the body and brain and the sensory experiences of the beverage.
While the neurochemical responses can be attributed to caffeine, the sensory experiences must be explored further.
The sensory experience could be a placebo effect of drinking the beverage, a response to the relief from caffeine withdrawal, or a result of other coffee compounds.
The researchers mention that fMRIs can be stressful to some people and this may have skewed the results.
The absence of a non-drinker control sample is a limitation of the study too. This could have helped rule out withdrawal symptoms as a reason for these sensory changes.
The fMRIs in this study only analyzed resting-state brain connectivity. Measuring the connectivities in task-oriented states may provide more precise results.
How Genes Regulate The Effects of Caffeine on Sleep?
While coffee is certainly helpful in feeling more alert in the morning, here are other ways to move from rest to preparedness without depending on caffeine.
One of the easiest ways to feel more alert in the morning is to pull the window shades up and let sunlight enter the room.
You could also take a quick walk outdoors to soak up the sunlight.
Sunlight helps shake off the morning grogginess.
One of the main reasons people feel tired and sleepy in the morning is not having 7-8 hours of restful sleep at night.
Going to sleep and waking up at set times and having a good night’s sleep can both help stay alert and active in the morning.
Even 10-15 minutes of exercise in the morning can help get the blood pumping across the body and brain and help clear up grogginess.
Consuming a protein-rich breakfast in the morning will help give the body the needed energy to go through the day actively and with better focus.
Some medications you take may cause grogginess and excessive daytime sleepiness.
Talk to your doctor about this in that case, and try switching medicines or altering doses.
for Osteoarthritis
The Gene Nutrition panel of Xcode Life includes 47 important nutritional aspects. 10 significant markers are analyzed for caffeine consumption and metabolism.
If you have done an ancestry genetic test with companies like 23andMe, AncestryDNA, MyHeritage, etc., you can learn your CYP1A2 gene status in just 3 steps.
Not yet tested?
If you're new to the world of genetic testing, we've got you covered!
You can now get your ancestry DNA kits at an additional discount!
By following the link provided in this article, you can purchase a DNA kit at 10% OFF (the discount will be reflected when you add the product).
This will ensure that you have everything you need to embark on your genetic journey.
Once you receive your kits, you can follow the instructions given by the respective service providers to collect your sample and ship it.
After you receive your DNA test results from the kit, you can upload your DNA data to our secure platform.
https://www.frontiersin.org/articles/10.3389/fnbeh.2023.1176382/full
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4997286/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3777290/
https://pubmed.ncbi.nlm.nih.gov/15635355/
https://pubmed.ncbi.nlm.nih.gov/1356551/
https://medlineplus.gov/caffeine.html
https://my.clevelandclinic.org/health/articles/22581-dopamine
https://www.intechopen.com/chapters/71528
https://www.webmd.com/sleep-disorders/ss/slideshow-wakeup-tips
Botox for hair loss - doesn’t this sound exciting?
Botox injections have become one of the favorite cosmetic procedures performed worldwide to help reduce the signs of aging.
Researchers are now exploring using osteopontin in skin moles to accelerate hair growth in people with baldness and hair fall.
If successful, this may soon replace the need for expensive hair transplantation surgeries and help people with alopecia areata get a permanent solution to balding.
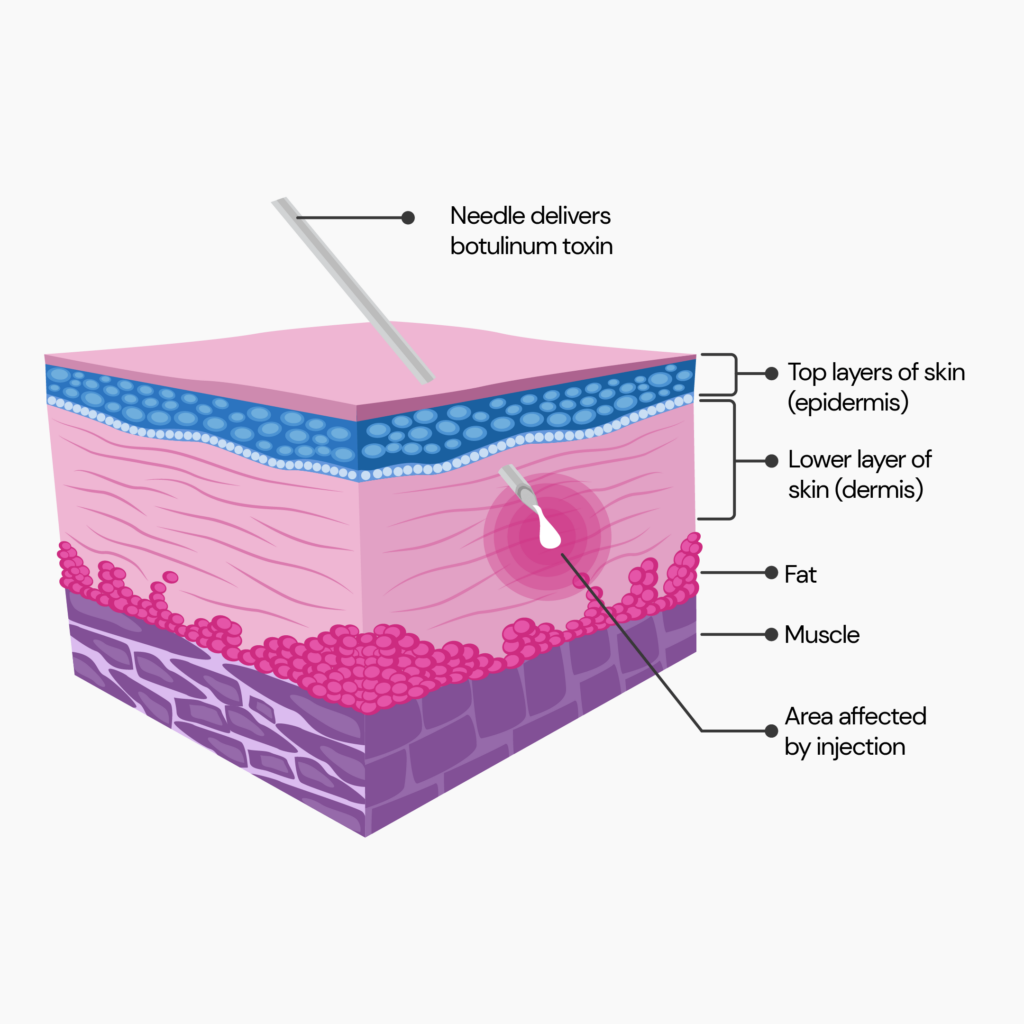
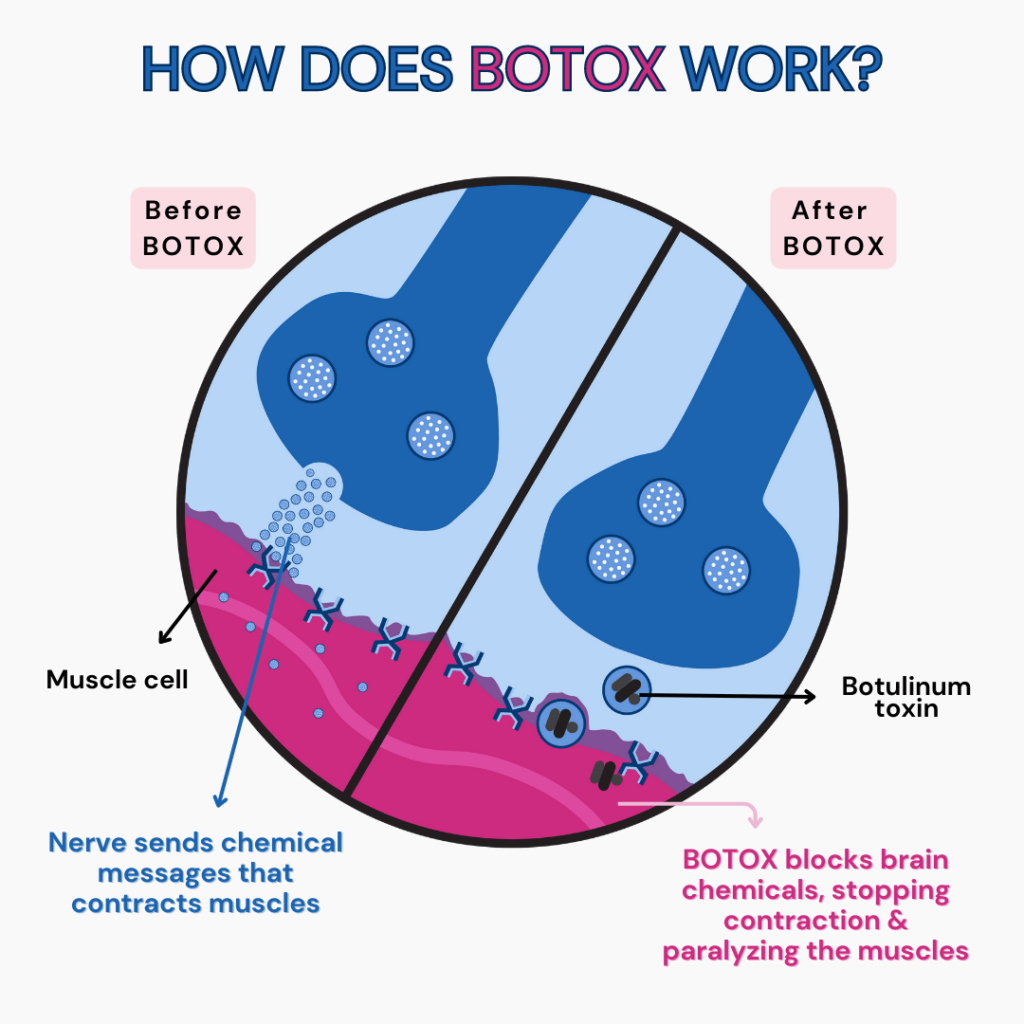
Botulinum toxin (botox) is a drug made from the Clostridium botulinum bacterium.
This bacterium causes a rare disease called botulism, characterized by muscle weakness, breathing difficulties, and even death.
In small doses, botox can help relax facial muscles and reduce the appearance of wrinkles, fine lines, and frown lines.
Botox functions by inhibiting the release of certain neurotransmitters in the muscles.
It is also sometimes used to treat certain health conditions like muscle spasms, excessive sweating, and migraine.
Botox injections are prevalent cosmetic procedures in the United States, with 3 million injections opted annually.
In recent times, there have been several products marketed as hair Botox.
However, these are not the same as Botox injectables for the skin.
Hair botox is just an attractive name given to hair nutrients created to give shinier, thicker, and lustrous hair.
Many of these hair nutrient masks contain collagen that coats the hair strands, making them look smoother, shinier, and thicker.
Such botox for hair loss products is available over-the-counter and has to be applied externally to the hair strands.
According to experts in the hair styling industry, these products don’t create any long-lasting impact and need to be used regularly to maintain the look.
Currently, researchers are exploring the idea of extracting a molecule from skin moles and using them to stimulate hair stem cells.
If successful, this could be the real ‘botox for hair loss’ people have been waiting for.
Melanocytes are cells that produce melanin.
Melanin is a pigment that gives color to our skin, eyes, and hair.
Sometimes, melanocytes group together and form patches on the skin, creating moles.
It is very common to see a single strand of thick hair growing from the center of skin moles in the body.
Researchers have now identified a particular compound in these moles that cause overproduction of these hair strands.
This compound also leads to hair growing darker and thicker.
They now want to explore the idea of using cells from the mole to create botox-like injectable solutions for the hair.
In June 2023, Wang, Plikus, and their team published an article in Nature that explored the effect of hyperactive melanocyte cells on hair growth.
In simpler terms, this is being called botox for hair loss.
According to the researchers, melanocytic moles or nevi in the skin often display excessive hair growth.
The researchers believe that this could be because of hair stem cell hyperactivity.
They are exploring the idea of extracting the molecules that lead to hyperactivity and injecting them in balding areas of the scalp to promote hair regrowth.
This study was performed on mice models.
The effect of hyperactive melanocyte cells on human balding and hair loss is yet to be studied.
The study identified a molecule named osteopontin in hairy moles that wasn’t found in significant amounts in regular skin cells.
Osteopontin is a type of signaling protein that plays a role in multiple biological processes, including:
According to the researchers, osteopontin could cause thicker, denser hair strands to grow from moles.
Osteopontin was predominantly found in higher quantities in aged melanocytes (senescent cells).
Researchers report that this signaling protein in senescent cells could activate dormant hair cells into their anagen phase (growth phase).
This could be why hairy moles develop thicker hair very quickly.
Hair loss is usually a result of the decrease in the quantity of signaling proteins in the hair follicles, which activate the anagen phase.
By extracting osteopontin and micro-injecting it into the cells on the scalp of mice models, the researchers were able to promote better hair growth.
They want to experiment with the same effect on human hair stem cells to see if this would solve alopecia and general hair loss.

In some cases of hair loss, the stem cells of hair may have remained dormant for a very long time.
Researchers aren’t sure if such dormant cells can be reactivated again with this method.
Even with osteopontin, the new hair growth would depend on the features of the hair follicle.
So, it may not be possible to grow thicker and lustrous hair in everyone who uses this botox for hair loss.
If a person always had thin and brittle hair, they would probably regrow hair with similar features.
Right now, the only permanent cure for baldness is hair transplantation surgery.
Not many choose to opt for this invasive and expensive process.
Only a handful of FDA-approved alopecia products are on the market; these don’t work 100% for everyone.
As this research progresses, there is hope for people with balding and excessive hair fall issues to regrow their hair back without surgery.
Amplifica, a biopharmaceutical company based out of California, has just started human trials on this botox for hair loss treatment.
According to Amplifica, the first human dose was given on June 27th, 2023.
The researchers at this biotech company expect the study to be completed by the first quarter of 2024.
Meanwhile, other companies could also explore these botox for hair loss treatments and produce results earlier.
Oral Minoxidil For Hair Loss: A Complete Guide
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5782443/
https://www.nature.com/articles/s41586-023-06172-8
https://medlineplus.gov/botox.html
https://www.cdc.gov/botulism/index.html
https://www.mayoclinic.org/tests-procedures/botox/about/pac-20384658
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7874868/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2778587/
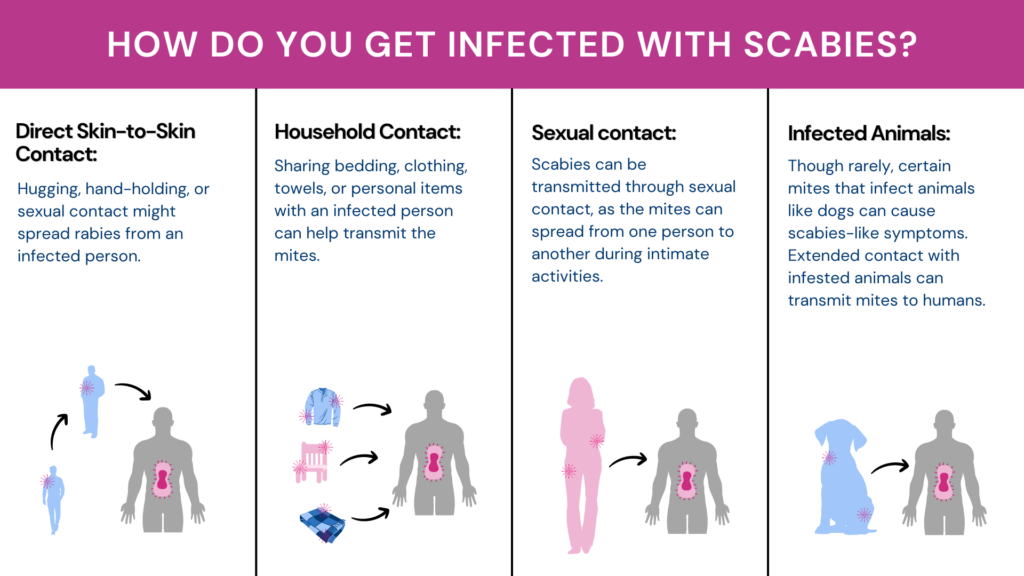
If you are concerned about your sexual health, “scabies” must already be on your radar. When it comes to sexually transmitted diseases, AIDS, Chlamydia, and Syphilis are all some familiar names we come across. However, research suggests that even though scabies is a skin condition, it can be passed through sexual contact, prompting the question, is scabies an STD?
Did You Know? Certain gene changes influence your risk for various skin conditions like dermatitis, acne, psoriasis, etc. Learning about this genetic risk can help customize your skincare and elevate your skin health.
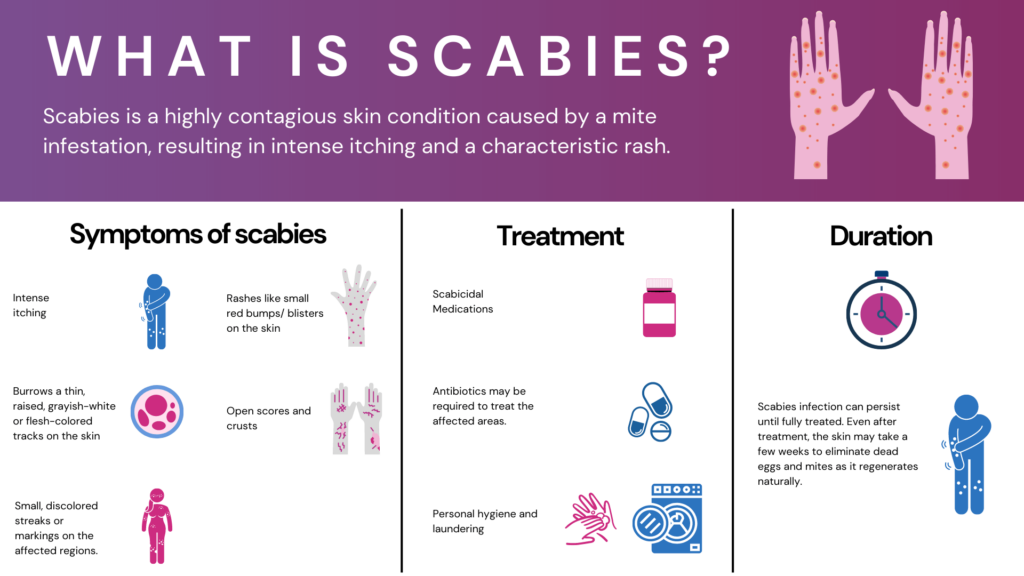
Scabies is a highly contagious skin disease.
It is an intensely itchy skin condition caused by a type of mite.
It spreads through physical contact within families, schools, or nursing homes.
Scabies is caused by a tiny mite called Sarcoptes scabiei.
When this mite reproduces, it lays eggs under the surface of human skin.
When these eggs hatch, the new mites crawl on the skin, making new burrows.
It causes intense itching, which increases at night.
Scabies mites are found in the genital area, on the wrists and elbows, underneath the arm, on the stomach, feet, and ankle.
The most common symptoms of scabies are:
These symptoms show up three to six weeks after initial infection.
However, if you have had scabies previously and got reinfected, you might start showing symptoms immediately.
Yes, scabies is considered an STD as it can spread by sexual contact. But scabies can also apply by nonsexual routes.
Furthermore, unlike other STDs, barriers like condoms or dental dams don't guard against scabies.
Scabies can also be transmitted without sexual contact.
People can get scabies by being in close contact with an infected person.
You can also get infected if you share bedding or clothing with an infected person.
Poor personal hygiene can make you more prone to getting a scabies infection.
Crusted or Norwegian scabies is a severe form of scabies infestation.
Typically, a host has no more than 10-15 mites on their body.
But in crusted scabies, people can have hundreds of mites crawling under their skin, causing extreme itching.
The rashes are more prominent and look like crusted patches of skin that crumble when touched.
People with weakened immune systems usually suffer from crusted scabies.
Usually, older people and children, people suffering from an immunosuppressive disorder such as AIDS, suffer from crusted scabies.
However, it can also spread by hugging or being in close contact with an infected host.
Scabies is highly contagious and spread through skin-to-skin contact.
The most common form of scabies transmission is sexual contact.
However, scabies can also spread in nonsexual contact, such as:
You are more likely to get scabies from sustained skin-to-skin contact with a person.
Usually, a simple handshake does not transmit scabies.
Pet animals cannot spread human scabies.
Pets can be infected with another type of scabies mite that usually doesn’t infect humans.
Scabies mites can live on a host for 1-2 months.
They are contagious during this period.
Even after treatment, the itching and discomfort might last longer.
However, scabies cannot live for more than 48 hours off the host.
Mites die above 50 degrees Celsius.
A simple physical exam can diagnose scabies.
Your doctor might also perform ink tests and tissue biopsies to detect scabies.
Scabies can be treated with overnight creams or lotions.
Your doctor will advise you how to use these treatments.
The itch may be persistent, and antihistamines can help.
Scabies can survive on mattresses or other inanimate objects for 2-3 days.
You can kill them with a vacuum or use high-temperature steam.
Scabies is considered an STD as the condition can spread through sexual contact.
It is caused by a mite that lives and burrows under human skin.
Scabies can also spread by casual physical contact, such as shaking hands or living with an infected person.
Practicing good personal hygiene habits and avoiding close contact with infected people are some ways to avoid scabies.
https://www.healthline.com/health/is-scabies-an-std
https://www.cdc.gov/parasites/scabies/index.html
https://www.who.int/news-room/fact-sheets/detail/scabies
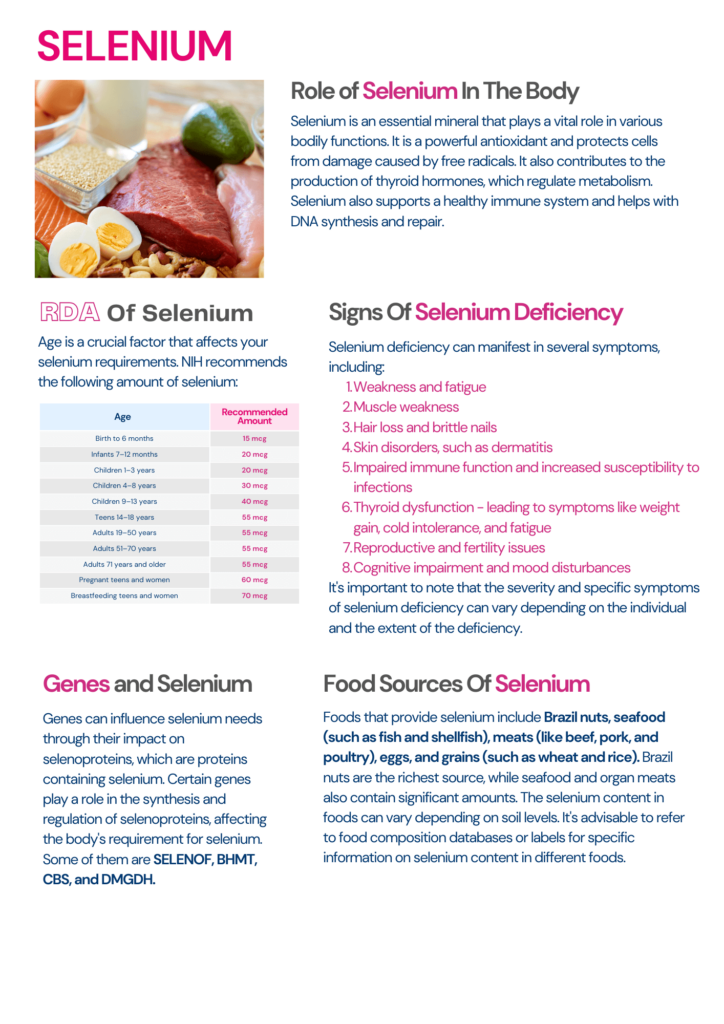
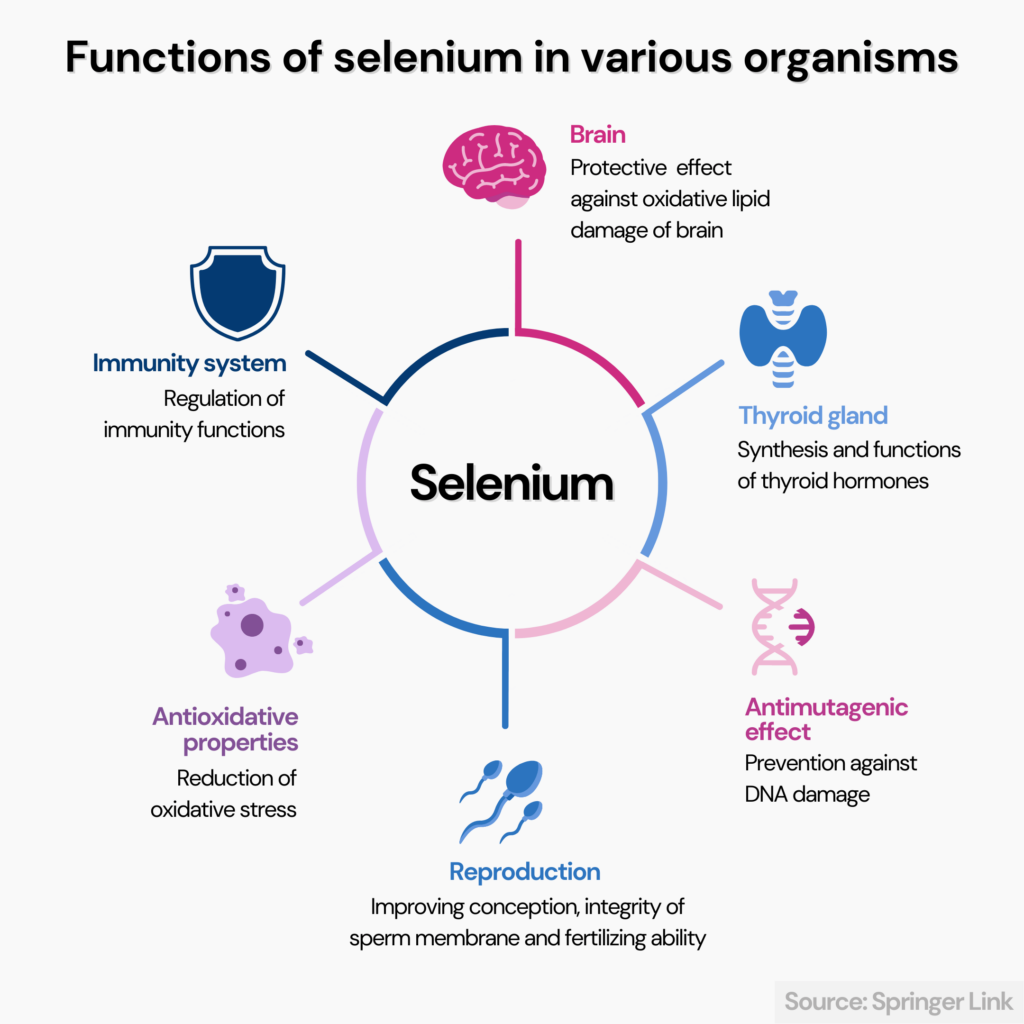
When it comes to a balanced diet, most people only focus on the macronutrients and dismiss the equally important trace minerals. One such micronutrient is selenium. This trace mineral plays a role in various functions of the body and is especially important for women. From aiding in increasing estrogen levels to improving fertility and preventing pregnancy-related complications, maintaining adequate levels of selenium will help women stay healthier physically and mentally. This article will take you through seven science-backed selenium benefits for women and also go on to suggest the best food sources to consume recommended levels of the mineral.
Did You Know? Your genes influence how much your body absorbs and utilizes selenium from food. Certain gene changes can increase your risk for selenium deficiency. Learn more.
Selenium is a rare mineral found in the earth’s crust.
Plant sources that grow in regions where the soil is rich in selenium absorb this mineral.
Animals that graze on these plants end up ingesting selenium.
As a result, many plant and animal-based foods that humans consume have traces of selenium.
Selenium plays a role in many everyday functioning of the body, including the following.
According to the National Institute of Health, the following are the recommended dietary allowance of selenium for women.
| Age | Recommended amount of selenium (mcg) |
| 0-6 months | 15 |
| 7-12 months | 20 |
| 1-3 years | 20 |
| 4-8 years | 30 |
| 9-13 years | 40 |
| 14+ years | 55 |
| Pregnant women | 60 |
| Lactating women | 70 |
While the right amounts of selenium benefit both men and women, this trace mineral may be especially favorable for women because of its ability to boost estrogen.
Estrogen is the primary female hormone responsible for developing female sexual characteristics in women.
Low estrogen levels may increase the risk of certain cancers, heart diseases, osteoporosis, and insomnia.
Low estrogen levels may also cause vaginal dryness, mood swings, hot flashes, and night sweats.
For estrogen to be helpful to the body, it needs to be broken down into various other compounds that the body uses.
Selenium helps the liver break down estrogen into usable forms.
Adequate selenium intake may reduce the risk of heart disease.
A 2006 meta-analysis analyzed the effects of selenium on coronary health in 25 observational and six randomized trials.
The study reported that selenium concentrations were inversely proportional to heart disease risks.
A 2016 meta-analysis of 16 observational and 16 randomized control trials also reported similar results.
Lower selenium levels are associated with decreased survival rates after a breast cancer diagnosis.
A 2021 study analyzed the relationship between selenium levels and ten-year survival rates in women diagnosed with breast cancer.
This study reported that the cumulative 10-year survival rate for women with lower serum selenium levels was 65.1%.
In comparison, the 10-year cumulative survival rate of women with higher serum selenium levels was 86.7%.
Free radicals are found in the atmosphere and are also byproducts of metabolic processes.
Excess free radicals cause oxidative stress and damage the body's cells.
Cell-level oxidative damage causes various diseases, including inflammation, premature aging, Alzheimer’s, heart conditions, and cancers.
Selenium has antioxidant properties and helps protect against oxidative damage.
Selenium is essential for thyroid health.
This trace mineral plays a role in the production of thyroid hormones.
A 2015 cross-sectional observational study analyzed the effects of selenium levels on thyroid function in 6,152 participants in China.
According to the study, low serum selenium levels increased the risk of thyroid diseases.
According to the U.S. Department of Health and Human Services, one in five women experience a mental health condition such as depression, anxiety, or bipolar disorder.
A 2022 article on selenium and mental health states that the anti-inflammatory properties of selenium may help handle signs of depression.
Selenium may help manage various mental health conditions by regulating the thyroid hormones.
Brain-Derived Neurotrophic Factor (BDNF) is a protein that plays a role in brain neuron growth, maintenance, and development.
Low BDNF level is associated with various mental and neurological issues, including cognitive dysfunction, depressive disorders, Alzheimer’s disease, and Parkinson’s disease.
An older study on rodents reports that low selenium levels may lead to low BDNF levels in the brain and affect mental health.
Studies report that selenium plays a role in bringing down inflammatory responses in the body and improving adaptive immune responses.
Selenium deficiency may lead to slower immune response and abnormal immune cell functions.
While many studies relate adequate selenium levels to improved male fertility, this trace mineral also seems to have similar effects in women.
A 2022 systematic review reports that selenium supplementation may improve reproductive efficiency in women undergoing in-vitro fertilization treatments.
The same report also adds that maintaining the right selenium levels may prevent problems like preeclampsia and preterm birth in pregnant women.
According to the U.S. Department of Health, the tolerable upper intake limit of selenium for adults over 14 is 400 μg/day.
This is the maximum dose people can consume without dangerous side effects.
Consuming extremely high doses of selenium may lead to toxic effects.
According to experts, both acute and chronic ingestion of high quantities of selenium can cause toxicity.
A 2008 PMC article discusses the potential outbreak of selenium toxicity by a manufacturing company in 2008.
The affected people consumed a dietary supplement that contained 200 times more selenium than what was mentioned on the label.
The following were the symptoms recorded in the 201 identified cases of selenium toxicity.
| Symptoms | Percentage of people with selenium toxicity |
| Diarrhea | 78% |
| Fatigue | 75% |
| Hair loss | 72% |
| Joint pain | 70% |
| Brittle nails and nail discoloration | 61% |
| Nausea | 58% |
Seafood and organ meat are some of the richest sources of selenium.
Some grains and other plant-based food also contain adequate amounts of minerals.
| Sources of selenium | Micrograms/serving |
| Brazil nuts | 544 |
| Tuna | 92 |
| Sardines | 45 |
| Ham | 42 |
| Shrimp | 40 |
| Beef | 33 |
| Chicken | 22 |
| Brown rice | 19 |
| Egg | 15 |
| Milk | 8 |
| Spinach | 5 |
| Cashew nuts | 3 |
Table source: https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/
Selenium offers various benefits to women of all ages.
Selenium-deficient women should talk to their doctor and consider supplementing the mineral orally.
The following categories of women are at a higher risk of selenium inadequacy.
They may also benefit from oral selenium supplements.
Those with adequate levels of serum selenium can maintain or improve the numbers by carefully choosing a diet rich in selenium.
Including seafood, organ meat, and Brazil nuts regularly will help improve serum selenium levels.
How Genes Influence Selenium Requirements
The Gene Nutrition panel of Xcode Life includes 47 important nutritional aspects. 13 significant markers are analyzed for selenium needs.
If you have done an ancestry genetic test with companies like 23andMe, AncestryDNA, MyHeritage, etc., you can learn your selenium deficiency risk gene status in just 3 steps.
Not yet tested?
If you're new to the world of genetic testing, we've got you covered!
You can now get your ancestry DNA kits at an additional discount!
By following the link provided in this article, you can purchase a DNA kit at 10% OFF (the discount will be reflected when you add the product).
This will ensure that you have everything you need to embark on your genetic journey.
Once you receive your kits, you can follow the instructions given by the respective service providers to collect your sample and ship it.
After you receive your DNA test results from the kit, you can upload your DNA data to our secure platform.
https://academic.oup.com/jcem/article/100/11/4037/2836081
https://pubmed.ncbi.nlm.nih.gov/19033020/
https://pubmed.ncbi.nlm.nih.gov/25990689/
https://pubmed.ncbi.nlm.nih.gov/16093440/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7998294/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2698273/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5986464/
https://pubmed.ncbi.nlm.nih.gov/9584835/
https://www.nature.com/articles/s41598-022-05078-1
https://academic.oup.com/jcem/article/100/11/4037/2836081
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6321086/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6321086/
https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/
https://www.healthline.com/nutrition/selenium-benefits
https://www.webmd.com/a-to-z-guides/supplement-guide-selenium
https://www.medicalnewstoday.com/articles/287842#recommended-intake
When it comes to ovarian cancer, identifying the risk factors is crucial for early detection and prevention strategies. In this article, we delve into an intriguing area of research: is diabetes one of ovarian cancer risk factors? We investigate the scientific evidence and examine whether diabetes could influence the development of ovarian cancer.
Genetic ancestry tests are becoming increasingly popular. While your DNA can be used to learn about your roots, did you know that it can also reveal important things about your health risks and wellness aspects? This allows you to take proactive measures for health conditions, even before the symptoms appear, thereby preventing it. You can upload your DNA data to learn 1,500+ things about your health. Learn more.
Diabetes is a metabolic disease characterized by high blood sugar levels.
If your blood sugar levels are high but not high enough for diabetes, you may have prediabetes.
People with prediabetes are at a greater risk of developing diabetes.
However, with the right lifestyle modifications, it is possible to reverse prediabetes.
Depending upon the cause, diabetes is of three types:
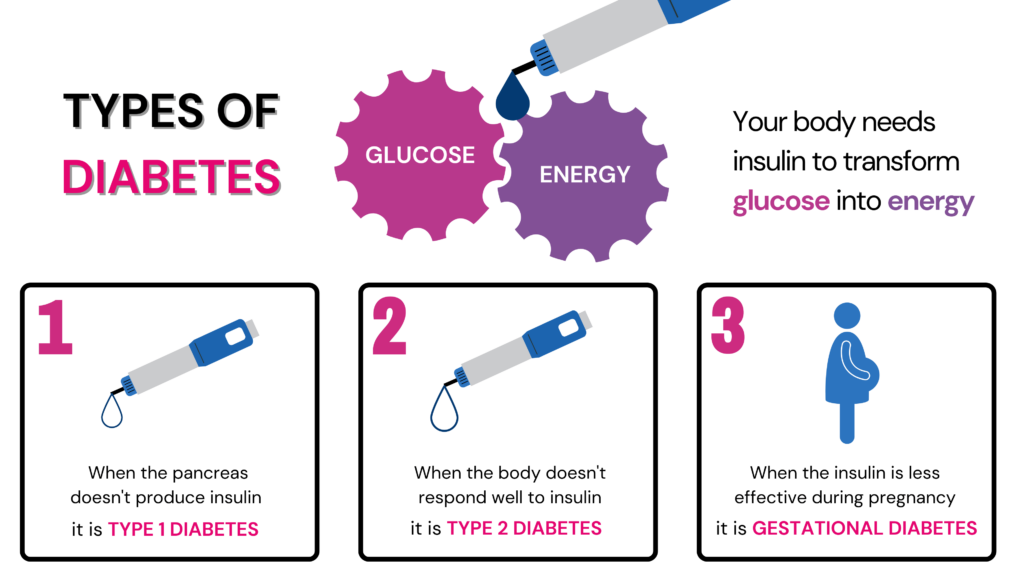
Glucose is the primary source of energy in the body. We get this glucose from the food we eat.
The pancreas secretes a hormone called insulin to help this glucose enter each cell in the body to generate energy.
In people with diabetes, glucose stays in the blood and is unable to reach the body cells for either of the following reasons:
Diabetes is a known risk factor for various diseases and complications.
This condition may increase your risk for kidney, eye, nerve, or heart damage.
Recent studies have also linked diabetes to some types of cancers.
Cancer is a condition characterized by the excessive growth of abnormal cells in the body.
These cells form a tumor.
Ovaries are a pair of organs that produce eggs (for reproduction) in females.
When cancer affects the ovaries, it is termed ovarian cancer.
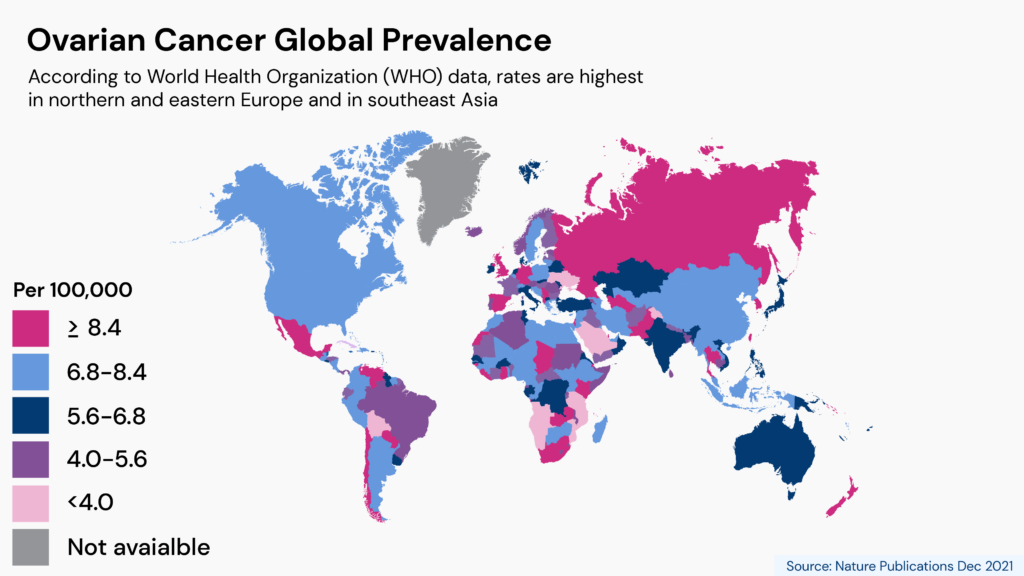
Ovarian cancer is the 8th most common cancer occurring in women.
A woman’s lifetime risk of developing ovarian cancer is 1 in 78.
Ovarian cancer occurs when there are abnormal genetic changes (mutations).
Two genes known to be high risk for ovarian cancer are the BRCA1 and the BRCA2.
Mutations in these genes are also associated with other gynecological cancers like breast cancer.
There are different types of ovarian cancer, depending on the tissue affected.
The most common type of ovarian cancer is epithelial cell cancer which begins in the cells that cover the ovary.
Other less common types of ovarian cancer are stromal and germ cell tumors.
While few ovarian cancer are benign, others are malignant.
Hysterectomy And Tubal Ligation May Increase Heart Disease Risk
While any person with ovaries can develop ovarian cancer, some are at a higher risk.
Risk factors for ovarian cancer include:
The relationship between type 2 diabetes and cancer has long been recognized.
Several studies link diabetes to an increased risk of various cancers, such as breast and endometrial tumors.
Furthermore, individuals with diabetes facing these diseases often experience more severe outcomes.
The impact of elevated blood sugar levels goes beyond diabetes management, as it leads to molecular changes that create a more favorable environment for tumor growth.
These changes can result from oxidative stress, inflammation, or even the facilitation of new blood vessel formation, which provides nourishment to rapidly dividing cells.
The metabolic abnormalities in association with obesity and diabetes are said to contribute significantly to the development and progression of cancer.
This could happen due to changes in the various signaling pathways in the body that get disrupted due to high blood sugar levels.
Some alterations from diabetes that promote cancer may be permanent, lasting even after blood sugar is under control, due to a phenomenon known as “metabolic memory.”
Recent research has provided strong evidence linking diabetes to an increased risk of ovarian cancer.
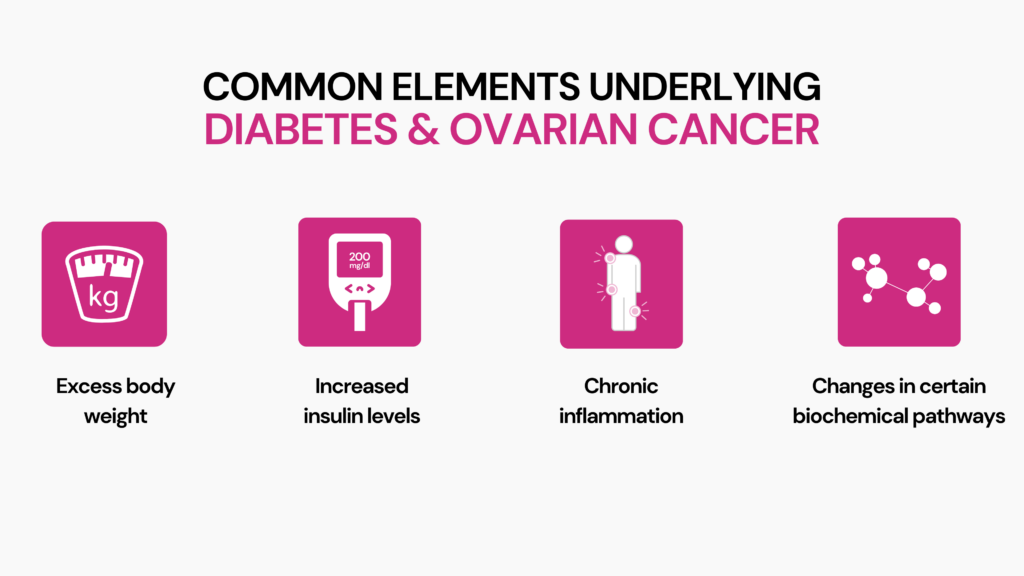
The research also suggests that there are common factors between type 2 diabetes and ovarian cancer, giving us clues about how diabetes might contribute to the development of ovarian cancer.
Researchers have discovered that a specific biochemical pathway called STAT3, which is more active in type 2 diabetes, also plays a role in helping ovarian cancer spread.
Another connection lies in the clinical data, which indicates that type 2 diabetes leads to higher levels of ovarian hormones that cause chronic inflammation.
This chronic inflammation can create an environment that encourages the formation and progression of tumors.
Moreover, the biochemical effects of diabetes can activate signaling pathways that promote ovarian cancer growth.
The side effects of diabetes can increase the levels of estrogen - research suggests that this may play a role in ovarian cancer.
Understanding these connections between type 2 diabetes and ovarian cancer can help us learn more about the risk factors and underlying mechanisms of this disease.
According to a 2021 review, diabetes increases the risk of developing various cancers, including ovarian cancer.
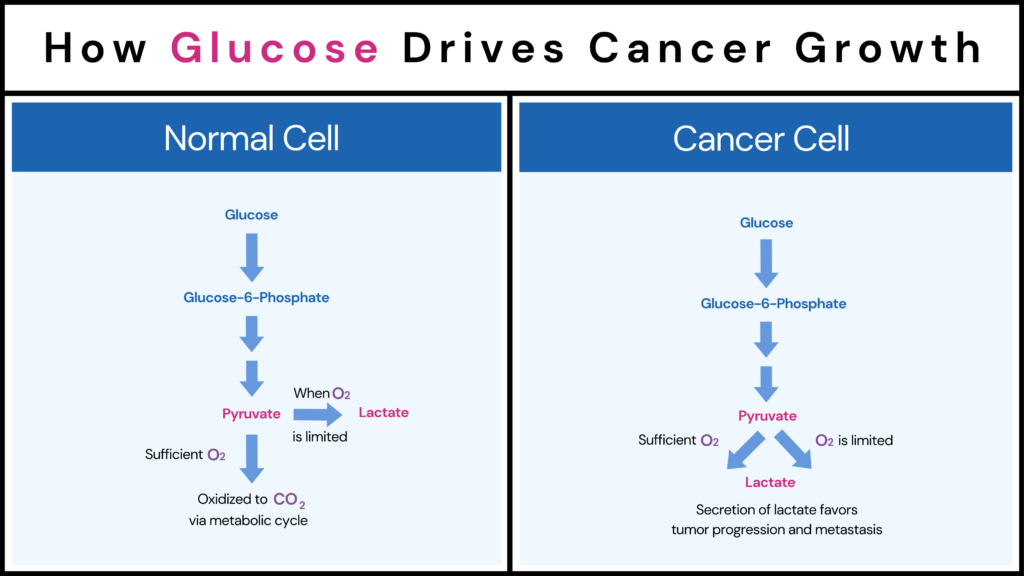
Cancer cells and tumors are actively dividing cells that show abnormal growth. So, they have high energy needs.
For this reason, in people with good blood sugar control, cancer cells grow more slowly and are often self-limiting.
However, in people with diabetes, the elevated blood sugar levels can feed the energy-hungry cancer cells, thereby encouraging their growth.
The growth and progress of ovarian cancer may be glucose-driven.
It has been found that diabetes can complicate cancer treatment.
At the same time, some newer treatments, like targeted therapy, can trigger the development of diabetes.
This is apparent in patients at a higher risk of developing the condition.
Diabetes makes cancer treatment challenging because:
Diabetes management requires a multidisciplinary approach in people who have cancer.
Depending upon the anticancer therapy you may be on, you may require managing hyperglycemia, fluids and electrolytes, hypertension, and cardiovascular complications.
Here are some ways to keep your blood sugar levels under control to lower your ovarian cancer risk:
Remember, these recommendations are general guidelines, and it's important to consult with your healthcare provider for personalized advice based on your individual needs and medical history.
Did you know that your genes can hold vital clues about your risk for certain health conditions? One such condition is familial hypercholesterolemia, a genetic disorder affecting cholesterol levels and increasing heart disease risk. In this blog post, we'll explain how familial hypercholesterolemia genetic testing can help you better understand your genetic risk for this condition. Whether you're new to genetic testing or seeking more information about your cholesterol levels, this article will be your guide.
Did You Know? Your 23andMe DNA Data includes 700,000 markers, which can be used to learn everything about your health and disease risk, including information on familial hypercholesterolemia. Learn more.
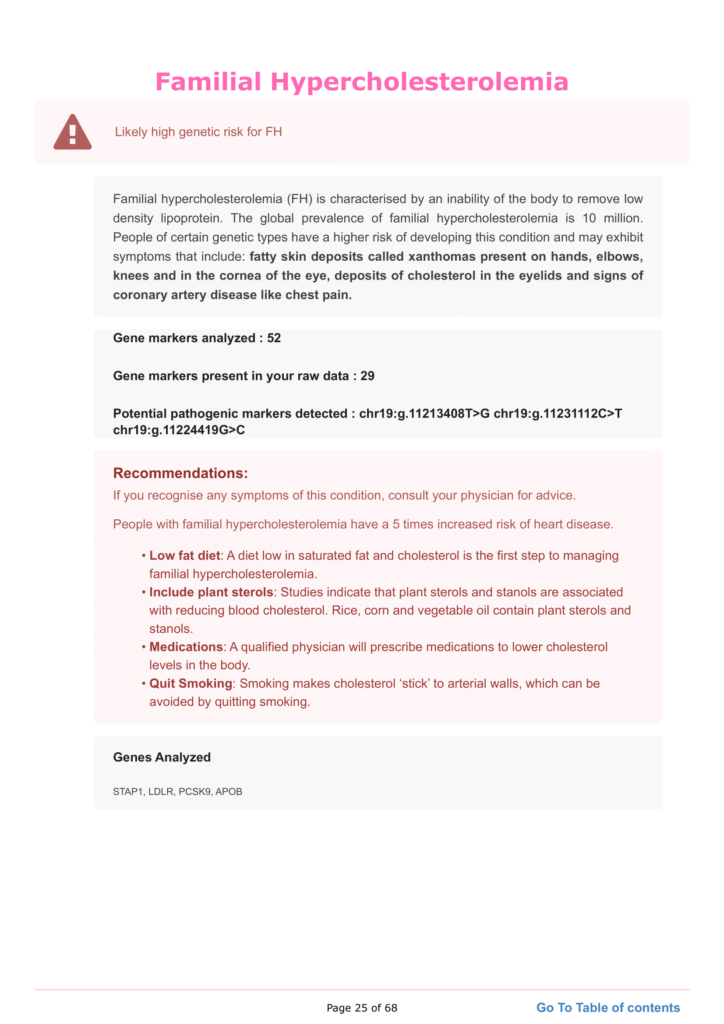
Familial Hypercholesterolemia (FH) is a genetic disorder.
It causes high cholesterol levels in the blood, specifically low-density lipoprotein (LDL) cholesterol, commonly known as "bad" cholesterol.
This condition inhibits the body's ability to remove LDL cholesterol from the bloodstream.
Consequently, it raises the risk of developing cardiovascular disorders like heart attacks and strokes at a young age.
Mutations in certain genes that control cholesterol metabolism in the body are the main cause of FH.
The LDL receptor gene (LDLR) is the most common gene affected by FH, with the apolipoprotein B gene (APOB) and the proprotein convertase subtilisin/kexin type 9 gene (PCSK9) following closely behind.
These mutations disrupt the regular activity of these genes, leading to difficulties in removing LDL cholesterol.
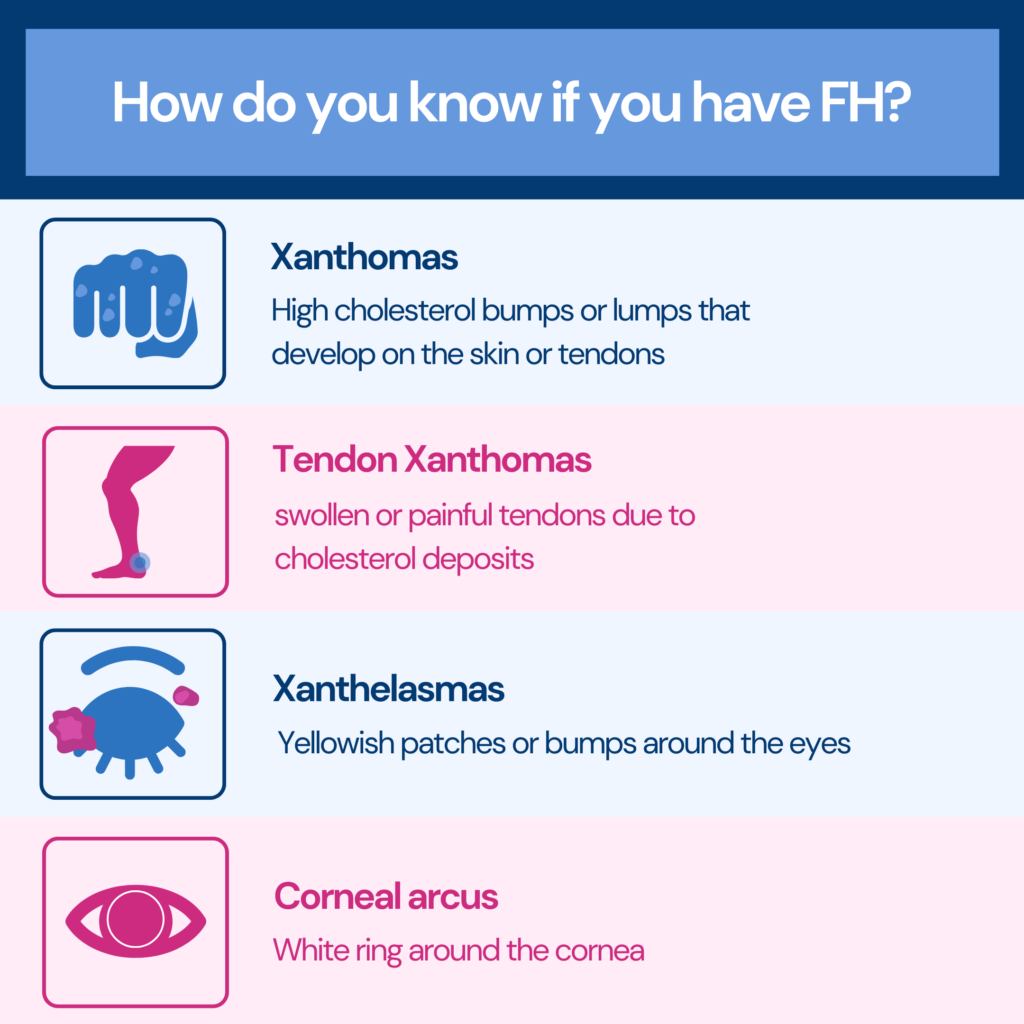
The symptoms of FH are often silent and may go unnoticed until complications arise.
Individuals with FH have high LDL cholesterol levels from birth, leading to the development of fatty deposits called plaques in the arteries.
Common signs and symptoms of FH include:
FH is characterized by non-sex chromosomal or autosomal dominant nature.
If one parent has the condition, the child has a 50% chance of getting it.
This condition is commonly referred to as Heterozygous Familial Hypercholesterolemia (HeFH).
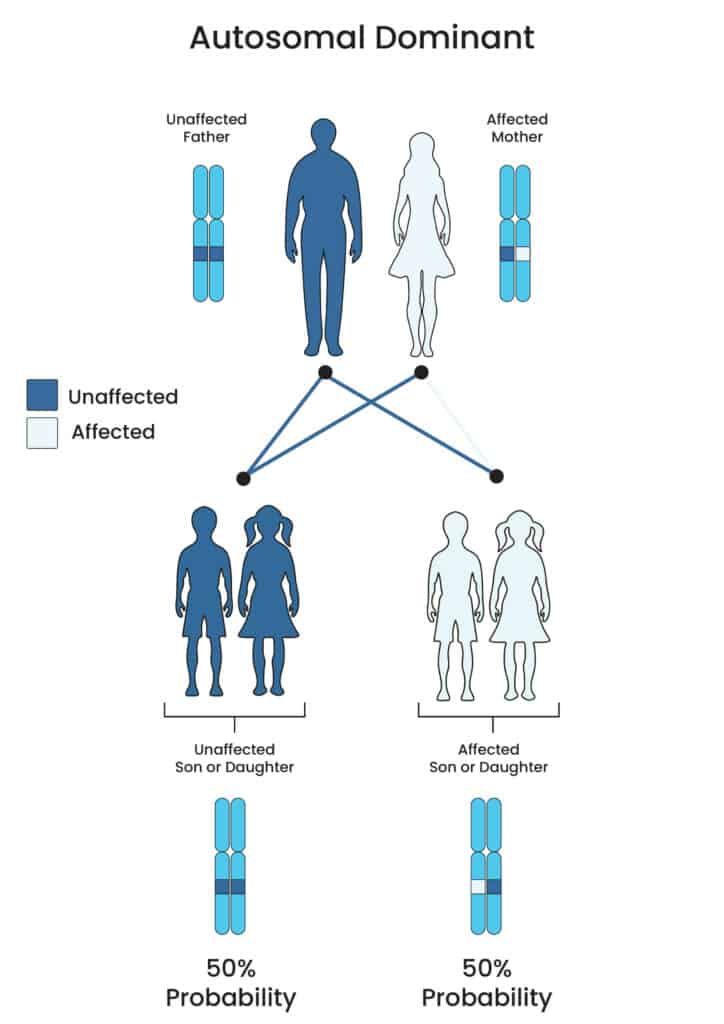
On the other hand, in Homozygous Familial Hypercholesterolemia (HoFH), both parents carry the FH gene, leading to a higher chance of their child experiencing this disorder.
Paul N. Hopkins, MD, a professor at the University of Utah School of Medicine, highlights that males with untreated HeFH face a 50% chance of experiencing a heart attack.
This risk is specifically associated with reaching the age of 45.
Females may encounter this occurrence between the ages of 55 and 60.
Genetic testing for FH is crucial in diagnosing the condition, identifying affected individuals, and providing appropriate management strategies.
The test analyzes specific genes associated with FH and detects genetic mutations that cause the disorder.
The criteria for FH genetic testing vary depending on the clinical guidelines. However, some common criteria include:
Simon Broom Diagnostic Criteria for FH
The Simon Broome criteria consider a variety of parameters, including cholesterol levels, clinical symptoms, molecular diagnosis, and family history. Focusing on determining the risk of severe CHD in individuals with Familial Hypercholesterolemia, these criteria are summarised in the table below.
| Diagnosis of definite FH cases |
| Total cholesterol levels above 290 mg/dL (7.5 mmol/L) or LDL-cholesterol levels above 190 mg/dL (4.9 mmol/L) in adultsTotal cholesterol levels above 260 mg/dL (6.7 mmol/L) or LDL-cholesterol levels above 155 mg/dL (4.0 mmol/L) in children under 16 years of age |
| ➕ |
| Tendon xanthomas in a patient or a 1st-degree relative (parent, sibling, child) or in a 2nd-degree relative (grandparent, uncle, aunt)Evidence of specific gene mutations related to LDLR, PCSK9, or APOB |
| Diagnosis of probable FH cases |
| Total cholesterol levels above 290 mg/dL (7.5 mmol/L) or LDL-cholesterol levels above 190 mg/dL (4.9 mmol/L) in adultsTotal cholesterol levels above 260 mg/dL (6.7 mmol/L) or LDL-cholesterol levels above 155 mg/dL (4.0 mmol/L) in children under 16 years of age |
| ➕ |
| Family history of early myocardial infarction (MI) before the age of 50 in a close relative (2nd degree) or before the age of 60 in a direct relative (1st degree)Family history of elevated total cholesterol levels > 290 mg/dL (7.5 mmol/L) in adult relatives or > 260 mg/dL (6.7 mmol/L) in children or siblings under 16) |
The Dutch Diagnostic Criteria for FH
The Dutch Diagnostic Criteria provide a modified approach to the Simon-Broome criteria by adding a scoring system and considering the underlying molecular defect of Familial Hypercholesterolemia. The table below summarizes the criteria, including family history, clinical history, physical examination, LDL cholesterol levels, and DNA analysis, enabling a more comprehensive diagnosis of FH.
| Criteria | Score |
| Family History | |
| First-degree relative with premature coronary and vascular disease (men ≤55 years, women ≤60 years) | 1 |
| First-degree relative with known LDL-cholesterol ≥95th percentile for age and gender | 2 |
| First-degree relative with tendon xanthomata and corneal arcus | |
| Children aged ≤18 years with known LDL-cholesterol ≥95th percentile for age and gender | |
| Clinical History | |
| Patient with premature coronary artery disease | 2 |
| Patient with premature cerebral or peripheral vascular disease | 1 |
| Physical Examination | |
| Tendon Xanthomas | 6 |
| Corneal arcus at age ≤45 years | 4 |
| LDL Cholesterol (mmol/L) (mg/dL) | |
| LDL-C ≥ 330 mg/dL (8.5 mmol/L) | 8 |
| LDL-C 250 - 329 mg/dL (6.5 - 8.4 mmol/L) | 5 |
| LDL-C 190 - 249 mg/dL (5.0 - 6.4 mmol/L) | 3 |
| LDL-C 155 - 189 mg/dL (4.0 - 4.9 mmol/L) | 1 |
| DNA Analysis | |
| Functioning mutations in the genes LDLR, APOB, and PCSK9 | 8 |
| Stratification | Total Score |
| Definite Familial Hypercholesterolemia | >8 |
| Probable Familial Hypercholesterolemia | 6-8 |
| Possible Familial Hypercholesterolemia | 3-5 |
| Unlikely Familial Hypercholesterolemia | <3 |
The MEDPED Diagnostic Criteria for FH
The MEDPED Diagnostic Criteria for Familial Hypercholesterolemia use age- and relative-specific total cholesterol values. It highlights the lower diagnostic cut-off levels for total cholesterol in persons with first-degree, second-degree, or third-degree relatives when compared to the general population cut-off levels. These factors help identify people at risk for FH based on their total cholesterol levels.
| Age (years) | First-degree relative with FH | Second-degree relative with FH | Third-degree relative with FH | General population |
| <20 | 220 mg/dL(5.7 mmol/L) | 230 mg/dL(5.9 mmol/L) | 240 mg/dL(6.2 mmol/L) | 270 mg/dL(7.0 mmol/L) |
| 20-29 | 240 mg/dL(6.2 mmol/L) | 250 mg/dL(6.5 mmol/L) | 260 mg/dL(6.7 mmol/L) | 290 mg/dL(7.5 mmol/L) |
| 30-39 | 270 mg/dL(7.0 mmol/L) | 280 mg/dL(7.2 mmol/L) | 290 mg/dL(7.5 mmol/L) | 340 mg/dL(8.8 mmol/L) |
| ≥40 | 290 mg/dL(7.5 mmol/L) | 300 mg/dL(7.8 mmol/L) | 310 mg/dL(8.0 mmol/L) | 360 mg/dL(9.3 mmol/L) |
Genetic testing for FH is essential for several reasons:
The Top 3 Genetic Liver Diseases Of 2023
Genetic testing for FH is typically conducted using a targeted approach focused on the known genes associated with the condition.
Three genes (LDLR, APOB, and PCSK9) are known to cause FH.
The process begins by identifying people with FH through clinical diagnosis, which includes a lipid test, physical examination, and evaluation of family history.
Once FH is confirmed in an individual, genetic testing can be extended to other family members through cascade screening.
This approach identifies the specific genetic variant responsible for FH within the family.
Genetic testing is usually done under the supervision of a trained genetic counselor or a healthcare practitioner with skills in genetic testing.
According to NCBI, the cost of genetic testing for FH varies depending on the perspective and specific circumstances.
From the healthcare provider's standpoint, the simulation considered the direct costs of medical care.
Recently, many laboratories have introduced next-generation sequencing targeted panels for FH cases.
These panels offer genetic testing at a cost of less than $500.
Subsequent testing for relatives who may carry a known pathogenic variant is typically more affordable.
Their mentioned model of genetic testing for FH costs $250.
However, it may offer free testing for relatives within 90 days as part of the cascade testing process, particularly if they are identified as close relatives of an FH proband.
**Please note that the costs mentioned may change and vary depending on individual situations, insurance coverage, and regional differences.**
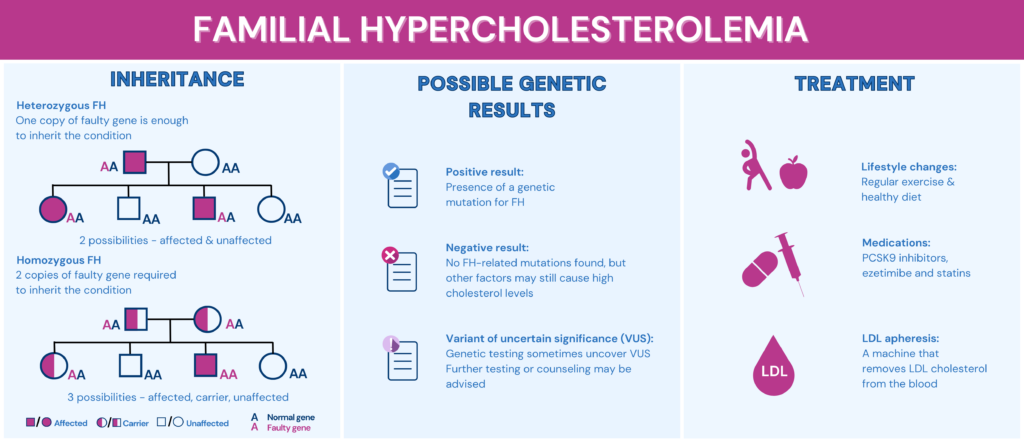
Individuals who undergo FH genetic testing receive precise results that provide essential data about their genetic makeup and risk of developing cardiovascular problems.
The possible genetic testing results for FH include the following:
Access to genetic testing results enables individuals to take charge of their health and proactively make informed decisions. With FH genetic testing results, individuals can take some of the following steps:
The 23andMe genetic testing service provides a specialized report called the Familial Hypercholesterolemia Genetic Health Risk Report.
This report focuses on detecting specific genetic variants associated with FH, characterized by high LDL cholesterol levels and a higher chance of heart disease.
To access this report, individuals can undergo genetic testing by purchasing and using the 23andMe Health + Ancestry Set.
The health panel of Xcode Life includes 45+ conditions. 52 significant markers are analyzed for Familial Cholesterolemia.
If you have done an ancestry genetic test with companies like 23andMe, AncestryDNA, MyHeritage, etc., you can learn your FH risk gene status in just 3 steps.
Not yet tested?
If you're new to the world of genetic testing, we've got you covered!
You can now get your ancestry DNA kits at an additional discount!
By following the link provided in this article, you can purchase a DNA kit at 10% OFF (the discount will be reflected when you add the product).
This will ensure that you have everything you need to embark on your genetic journey.
Once you receive your kits, you can follow the instructions given by the respective service providers to collect your sample and ship it.
After you receive your DNA test results from the kit, you can upload your DNA data to our secure platform.
I recently used xcode life to get one of their gene health reports. My experience was very good. I received the report the same morning within the time frame they stated. It was well detailed giving clear and easy to understand information and came in PDF form so it was easy to print. My personal experience has been brilliant and I would use them again.
- Ben Duncombe
FH can be classified into three possible genotypes, such as:
HoFH: The most severe form of FH occurs when an individual inherits two copies of the defective gene from both parents, resulting in a specific genotype.
HeFH: The heterozygous genotype is a common and less severe form of FH. It happens when an individual acquires one copy of the faulty gene from one parent.
CeFH (Compound heterozygous FH): This genotype occurs when an individual inherits two mutated genes responsible for FH, one from each parent. It is a rare form of FH and is typically more severe than HeFH.
FH treatment involves a blend of lifestyle adjustments and medication to decrease LDL cholesterol levels and reduce the risk of complications.
Here is an overview of the different treatment options for people with FH:
Lifestyle changes: Making lifestyle changes is crucial for people with FH. Lowering LDL cholesterol levels and decreasing the risk of heart disease can be achieved through these changes.
Medications: PCSK9 inhibitors and ezetimibe are alternative medications that can help people with FH who cannot reach target levels through lifestyle changes alone. Statins, the most frequently used FH medication, can also effectively lower LDL cholesterol levels.
LDL apheresis: LDL apheresis is a procedure that uses a machine to remove LDL cholesterol from the blood. It is an option for people with FH who have excessively high LDL cholesterol levels that cannot be regulated by lifestyle changes or medication.
Familial Hypercholesterolemia is a genetic disorder that results in high levels of LDL cholesterol in the bloodstream, developing the chances of cardiovascular diseases. This condition occurs from mutations within genes responsible for regulating cholesterol metabolism, namely LDLR, APOB, and PCSK9.
Diagnosing FH involves genetic testing, which analyzes specific genes associated with the condition to detect genetic mutations. There are various criteria for FH genetic testing, including cholesterol levels, family history, and specific symptoms like xanthomas and corneal arcus.
Genetic testing is crucial for early detection, family screening, and developing personalized treatment plans for individuals with FH. It is typically performed under the guidance of a genetic counselor or healthcare practitioner.
The cost of genetic testing for FH varies, but recent advancements with some labs offering testing for less than $500. Insurance coverage and regional differences can affect the cost.
Genetic testing can provide accurate information about a person's genetic makeup and risk of developing heart disease. Positive results confirm the presence of FH-associated mutations, while negative results signify the absence of known mutations. VUS results require further testing or genetic counseling.
With genetic testing results, individuals can consult with healthcare professionals to develop personalized treatment plans, adopt a heart-healthy lifestyle, raise awareness among family members, and follow prescribed medications.
https://www.cdc.gov/genomics/disease/fh/FH.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2873730/
https://www.genome.gov/Genetic-Disorders/Familial-Hypercholesterolemia
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8403726/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3104361/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4217354/