Ehler-Danlos syndrome (EDS) is a group of rare inherited conditions that affect the body’s connective tissue.
It affects 1 in 5000 people worldwide.
The connective tissues in the body include skin, blood vessels, bones, muscles, and other supporting tissues.
Any defect or abnormality in the connective tissue can cause signs and symptoms ranging from mildly loose joints to serious, life-threatening complications.
There are 13 types of Ehler-Danlos syndrome, but most are rare.
The most common type of EDS is hypermobile EDS. Others include classical EDS, vascular EDS, and kyphoscoliotic EDS.
The signs and symptoms of EDS depend upon its type.
There is no specific treatment for EDS, but signs and symptoms can be managed with the proper support and advice.
Individuals with EDS can pass the same type of EDS to their children.
While the exact cause of EDS is unknown, at least 20 genes have been found to cause this condition.
Variants in the COL5A1 or COL5A2 genes and rarely COL1A1 can cause the classical type of EDS.
Direct-to-consumer tests like 23andMe do not offer diagnostic testing for genetic conditions like EDS.
This is because they test for a very small number of single nucleotide polymorphisms (SNP) and cannot be used as a replacement for clinical genetic testing.
If you wish to test for a personal or family history of a genetic condition, it is best to consult a healthcare provider and opt for a more detailed gene testing service.
Check the instructions here: How Do I Login To My 23andMe Account - 2023 Updated
Check the instructions here: How to download your 23andMe Raw Data for 3000 + Health Reports
If you don't have your DNA raw data, you can get a 23andMe kit from here.
Choose your reports here, or order the Genome Pack (all health and wellness reports) for 55% OFF
A new study sheds light on a potential link between reproductive health and heart disease.
This little-known connection, reveals that women who have undergone hysterectomy or tubal ligation may have an increased risk of developing heart disease.
This article explores the study's findings and what they mean for women's health. Whether you're considering these procedures or simply curious about the latest research, read on to learn more.
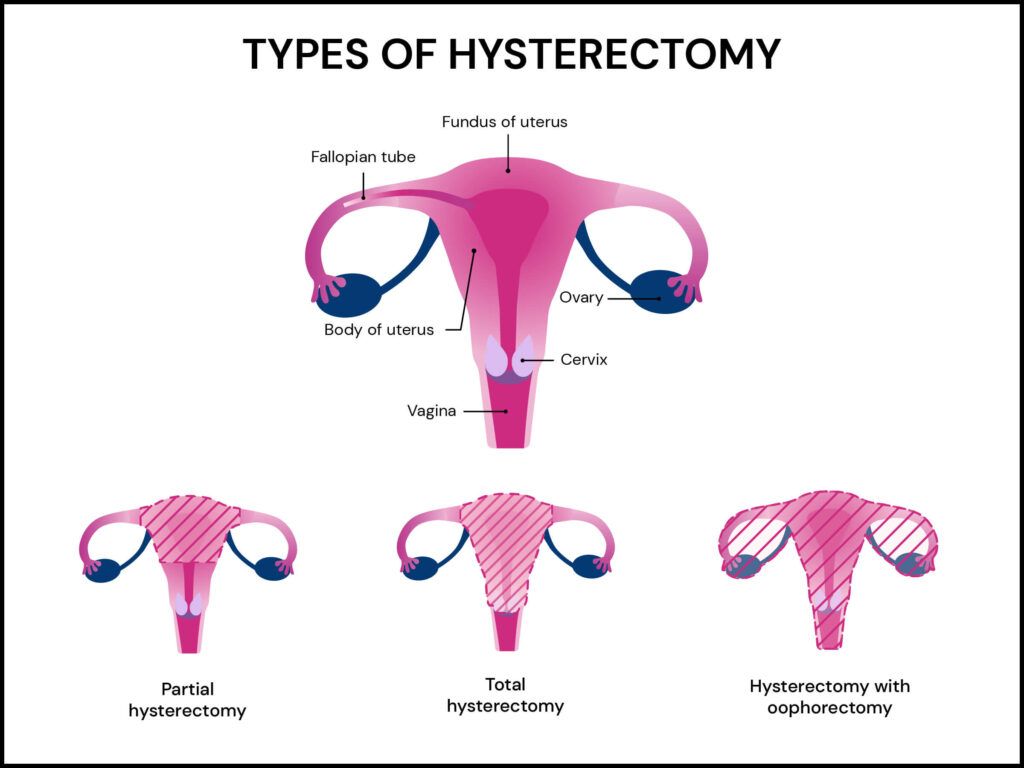
Hysterectomy and tubal ligation are two common gynecological procedures.
A hysterectomy is a surgery that involves removing a woman's uterus. A hysterectomy can be done with or without oophorectomy, which is the removal of the ovaries.
Why would someone need their uterus removed?
There are a few reasons why this procedure might be recommended.
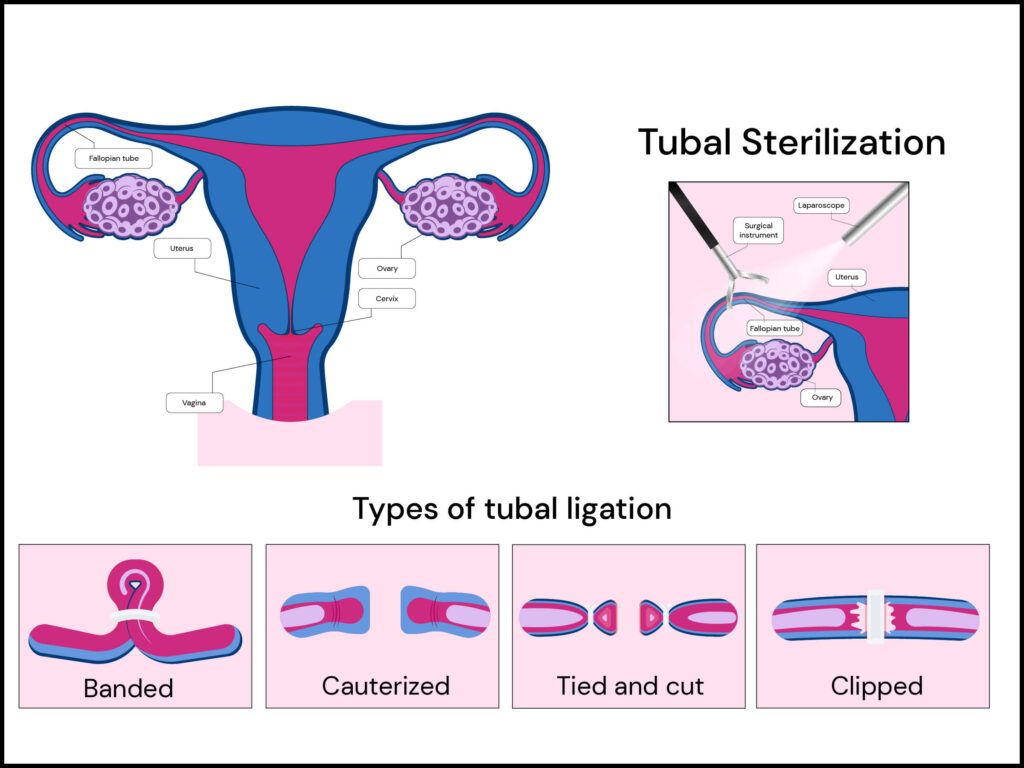
Tubal ligation is often called "getting your tubes tied" and is a permanent birth control method.
During a tubal ligation, the fallopian tubes are blocked or sealed off to prevent the eggs from meeting the sperm. This means that pregnancy becomes highly unlikely.
Tubal ligation may decrease your risk of ovarian cancer, especially if the fallopian tubes are removed.
A recent study published in the Journal Of Women’s Health examined the association between these gynecological procedures and cardiovascular disease risk.
This study was done using the data from participants in the Nurses’ Health Study II, which included over 116,000 people.
The participants were between the ages of 25-42 years.
They were followed from 1989 to 2017 (28 years).
The researchers categorized the participants into the following groups:
They then looked at cardiovascular disease incidents and considered participants who had experienced both fatal and non-fatal heart attacks and strokes, and fatal coronary heart disease.
They also included the participants who underwent a procedure called coronary revascularization, which is a procedure to improve blood flow to the heart.
Hysterectomy with and without oophorectomy and tubal ligation were both associated with a greater risk of cardiovascular diseases and coronary revascularization.
The greatest risk was observed in those who had a hysterectomy surgery before the age of 50 years.
The author also says, “Future research is needed to understand the mechanisms underlying the associations between gynecologic surgery and cardiovascular risk and the risks and benefits associated with these procedures to better counsel patients.”
Certain gene changes can increase your risk for heart disease! Learning about your genetic risk can help reduce the risk and even prevent the condition. Visit the link below for a genetic health report covering over 45 conditions, including heart disease.
Taking care of your heart is essential for a long and healthy life. Here are five effective tips to help you keep your heart in shape.
By incorporating these strategies into your lifestyle, you'll be taking a proactive step towards a healthier heart and a happier you.
Note: The information provided here is based on evidence and facts available at the time of writing. Always consult your healthcare provider for personalized advice and guidance on maintaining a healthy heart.
Have you ever wondered why you are allergic or sensitive to the same foods as your parents and grandparents?
One reason behind this can be your genetics.
Yes, you read it correctly.
Genetics can be a critical factor in deciding whether your body experiences a possible food intolerance.
For instance, if you and your father have lactose intolerance, it highly suggests an underlying genetic factor. But it's nothing to be worried about.
Instead, it is essential to be familiar with these potential triggers so you can take precautionary steps toward sustaining your health.
To help you understand this concept better, here is a comprehensive guide on how genetics make a difference to your immune system (causing food allergies) and your body's capability to digest food (leading to food intolerances).
So, let's delve deeper and gain excellent food genetics knowledge!
Food intolerances and food allergies are two circumstances that cause comparable side effects yet influence the body in various ways.
The immune system attacks and neutralizes foreign invaders, possibly dangerous to the body.
However, in some cases, due to certain genetic changes, the immune system attacks harmless substances, such as certain foods. This is called a food allergy.
This response typically occurs moments after food consumption, with even a tiny amount capable of sparking symptoms.
A typical example is shortness of breath and low blood pressure after contact with peanuts or seafood.
It is critical to seek immediate medical attention for food allergies, and treatment plans may include medication or using an epinephrine auto-injector.
Generally, common food allergens originate from peanuts, tree nuts, shellfish, fish, milk, eggs, and soy.
Food intolerances, in contrast to food allergies, are caused by the digestive tract rather than the immune system.
Food intolerance is generally less severe than a food allergy; however, symptoms can be managed by avoiding problem foods or medication.
Did you know? Food allergy affects up to 15 million people, including 5 million children. Considering that environmental factors have been distinguished as the essential driver of food allergies, certain studies show that genetic qualities may also play a significant role.
For instance, as per a report in the World Allergy Organization journal, identical twins had a 65% chance of sharing their nut allergy—significantly greater than the 10% chance among non-identical twins. This indicates a significant genetic involvement and a resultant genetic component in developing food allergies.
Additionally, a study on 1,500 children with food allergies from the US and Germany uncovered five genetic regions that seem to raise other people's vulnerability to food allergies. This implies that these genetic locales might increase the chances of developing allergies to various food varieties.
Notwithstanding, the human leukocyte antigen (HLA) region was found to be specific to peanut allergy cases. The HLA genes help the immune system distinguish between the body cells and foreign invaders like viruses or bacteria.
In the case of peanut allergies, certain changes in the HLA genes may lead to a greater likelihood of developing an allergy to peanuts specifically. Genetics of Food Allergy (GOFA) found two areas of the genes related to food allergies.
The main area was close to the FLG genes, and the second was on chromosome 5 near a cluster of cytokine genes.
While the rapid increase in the prevalence of food allergies suggests that environmental factors contribute more to their development, genetics play a significant role in determining the risk of developing them.
Identifying the genes involved in food allergies can contribute to understanding the disease in terms of recognition, prognosis, prevention, and possibly therapeutic interventions.
Food intolerance is a condition in which individuals experience trouble processing specific foods.
Research has demonstrated how genetic factors can play a part in food intolerance.
Celiac disease, an autoimmune disorder provoked by gluten consumption, can have strong genetic links.
Research suggests that genetics might explain up to 55% of cases of celiac illness.
Studies have recognized some genes related to celiac infection, including HLA-DQ, IL12A, IL18RAP, MYO9B, and others.
These genes initiate immune and inflammatory responses and regulate intestinal permeability and other aspects of gut health.
Another example of how genetics can affect food intolerance is lactase persistence.
Lactase is a chemical that helps digest lactose, a sugar tracked down in milk.
Many people produce lactase at the outset and in their youth; however, as they age, lactase production diminishes, prompting lactose intolerance.
Certain individuals can produce lactase well into adulthood, permitting them to drink milk easily.
This ability is known as lactase persistence and is also strongly influenced by genetics. The MCM6 gene, in particular, plays a key role in regulating lactase production.
However, not every person with a gene variation related to food intolerance will encounter side effects. Environmental factors also may play a significant role in this.
Genes affect food allergies, intolerances, and autoimmune sensitivities. Autoimmune diseases result from immune system errors wherein genetic and environmental factors play a part.
Autoimmune conditions lead to food sensitivities and intolerance.
Celiac disease, an autoimmune disorder, involves gluten. In addition, genetic factors, including HLA-DQ, IL12A, IL18RAP, and MYO9B genes, influence immune responses, inflammation, and gut health.
Hashimoto's thyroiditis is another autoimmune disease that can cause food sensitivities. Gene variations in CTLA4 and PTPN22 genes contribute to its development. Inflammatory bowel diseases (IBD) cause secondary food intolerances. IBD genetic factors include NOD2, IL23R, and ATG16L1 genes.
Family history is a risk factor that influences autoimmune diseases and related food sensitivities. Genetic research can identify risk factors and pathways. This helps manage autoimmune diseases and sensitivities. In all, genes impact food allergies, intolerances, and autoimmune sensitivities.
Understanding genetic factors can guide dietary choices, thereby minimizing sensitivity impact. Consult healthcare professionals for personalized nutritional advice and autoimmune condition management.
To diagnose food allergies and intolerances, you can seek clinical counseling. Various strategies can also be utilized to analyze these circumstances, including:
To sum up, genetics can influence the food we consume, leading to food allergies and intolerance.
Recognizing these genes can help understand the sickness better and take precautions.
You must be aware of possible triggers if you have a family history of food intolerance or allergies. This can help you take preparatory steps and make better food choices.
Researchers have identified several genes associated with arthritis.
In the sample report below, we've attempted to analyze some important genes that increase the risk of arthritis.
You can identify your genetic risk of arthritis by using your 23andMe DNA data and placing an order for the Gene Health Report.
Arthritis is a medical condition characterized by inflammation and pain in one or more joints.
The primary symptoms of arthritis are stiffness and swelling pain in the joints, which generally worsen as people age.
In America, arthritis affects nearly 59 million people - or one out of every four people.
The majority of Americans in the US suffer from this chronic condition.
Doctors believe genetics may be involved, particularly in cases when the condition strikes at an early age.
Over 100 different forms of arthritis exist, and they can be widely categorized as degenerative, infectious, inflammatory, and metabolic. The two most common kinds of arthritis are osteoarthritis and rheumatoid arthritis.
Rheumatoid arthritis is an autoimmune disease that damages the joints and causes changes in the tissues surrounding the joints, including cartilage (the sliding surface covering the bone) and the bone itself.
Osteoarthritis, the most common kind of arthritis, undergoes similar changes.
The cartilage degrades, thins, and eventually turns rough, giving less protection for the bones.
Other Types of arthritis
Other types of arthritis include:
Psoriatic arthritis is predicted to affect 2.4 million people. Psoriatic arthritis is caused by the inflammation that results from the common skin condition psoriasis. Psoriatic arthritis symptoms include:
Ankylosing spondylitis (AS) is a less frequent type of chronic autoimmune and inflammatory arthritis.
It causes pain and stiffness in the hips and back, eventually leading to the fusion of vertebrae in your spine.
This fusion is termed ankylosing.
The sacroiliac (SI) joints at the base of your spine are the primary targets of AS.
These signs include:
People do not inherit osteoarthritis; rather, they inherit an increased chance of acquiring it. According to research, genetics plays a role in between 40% and 65% of cases of osteoarthritis.
Genes that code for structural proteins of the extracellular matrix of the cartilage, particularly those that code for collagen type II (COL2A1), appear to play a significant role in the development of osteoarthritis.
Osteoarthritis is not caused by only one gene but by a combination of genes, other conditions, and environmental factors.
A thorough analysis of the genetics of Rheumatoid Arthritis (RA) found that the heritability was approximately 60%.
About 37% is believed to originate from genes connected to the human leukocyte antigen (HLA) system, also called the major histocompatibility complex or MHC genes. These are significant genes for the immunological response.
According to studies, there are four main genetic factors associated with Rheumatoid Arthritis:
HLA-DR4: the gene that is most strongly associated with RA. People who carry this gene are more likely to get RA than people who do not, and their symptoms may be more severe.
The STAT4 gene regulates and stimulates the immune response.
TRAF1 and C5 genes are essential for the genesis of chronic inflammation.
PTPN22 gene-Linked to the onset and progression of RA
Even though these gene variations are linked to RA, you can have all of them and not have the illness. However, RA has a significant genetic component but is not directly inherited.
Several HLA gene variations appear to influence the likelihood of developing psoriatic arthritis.
Nevertheless, 40% of those with PsA have at least one close relative with the condition.
90% of Ankylosing Spondylitis (AS) sufferers have the HLA-B27 gene. Some people without the gene also acquire AS, and not everyone with the gene gets AS.
Overweight: The major joints, such as the hips, knees, and ankles, are put under higher stress when a person is overweight.
Overweight people are more prone to experiencing early osteoarthritis.
Age: It has been observed that RA risk rises with age. The disorder is more prevalent in people 60 years of age and older.
Gender: Women are affected 2-3 times more than men by RA.
Unaddressed health concerns: Illnesses and injuries can make you more likely to develop arthritis. Joint injuries left untreated may result in accelerated cartilage aging.
Smoking: Smoking increases the loss of cartilage and makes you struggle more with joint swelling. This develops rheumatoid arthritis and can aggravate the signs and symptoms of osteoarthritis.
Nature of work: Some jobs require repetitive knee bending and squatting. There is a chance that arthritis will develop later in life as a result of that repetitive stress on a single joint.
We all know that alcohol and a good time often go hand in hand, but did you know that those boozy adventures could be playing a secret symphony with your thyroid?
It's time to pull back the curtain on a lesser-known consequence of that boozy escapade.
This article explores the surprising link between alcohol consumption and hypothyroidism, separating fact from fiction.
It’s time to dive deep into the impact of those after-work libations on your body's metabolic maestro.
Certain gene changes can put you at higher risk for developing many chronic conditions like diabetes, hypertension, and even hypothyroidism.
Learning about your genetic risks can help plan preventional strategies even before the symptoms appear.
The thyroid is a gland located in the neck and is known to produce hormones that help in metabolism and influence the growth and development of the human body.
Due to the number of body functions the gland regulates, a properly-functioning thyroid is essential for good health.
The thyroid releases more hormones into the bloodstream when the body requires more energy in certain conditions like pregnancy or temperature fluctuations.
The thyroid produces three hormones, namely:
Iodine is the building block for both these hormones.
Since the body cannot make its iodine, adequate consumption of this trace element is required for proper thyroid functioning.
Abnormal functioning of the thyroid gland can cause hormonal imbalances, which affect other body systems, including the immune and nervous systems.
1 in 20 people is affected by thyroid dysfunction during their lifetime.
Two common conditions that affect the thyroid gland are:
It is characterized by an excessive production of thyroid hormones.
While this condition can occur in both sexes, it is more common in adult women.
This condition is called hypothyroidism.
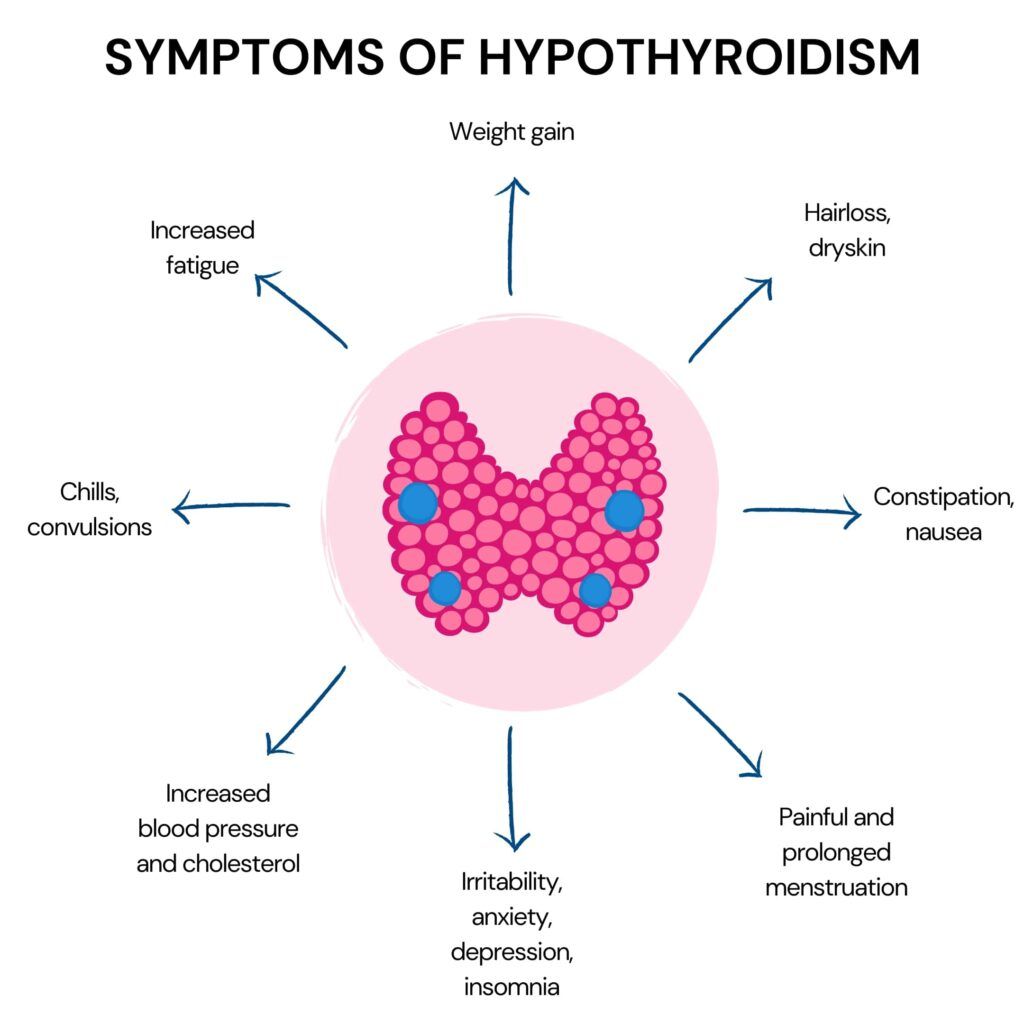
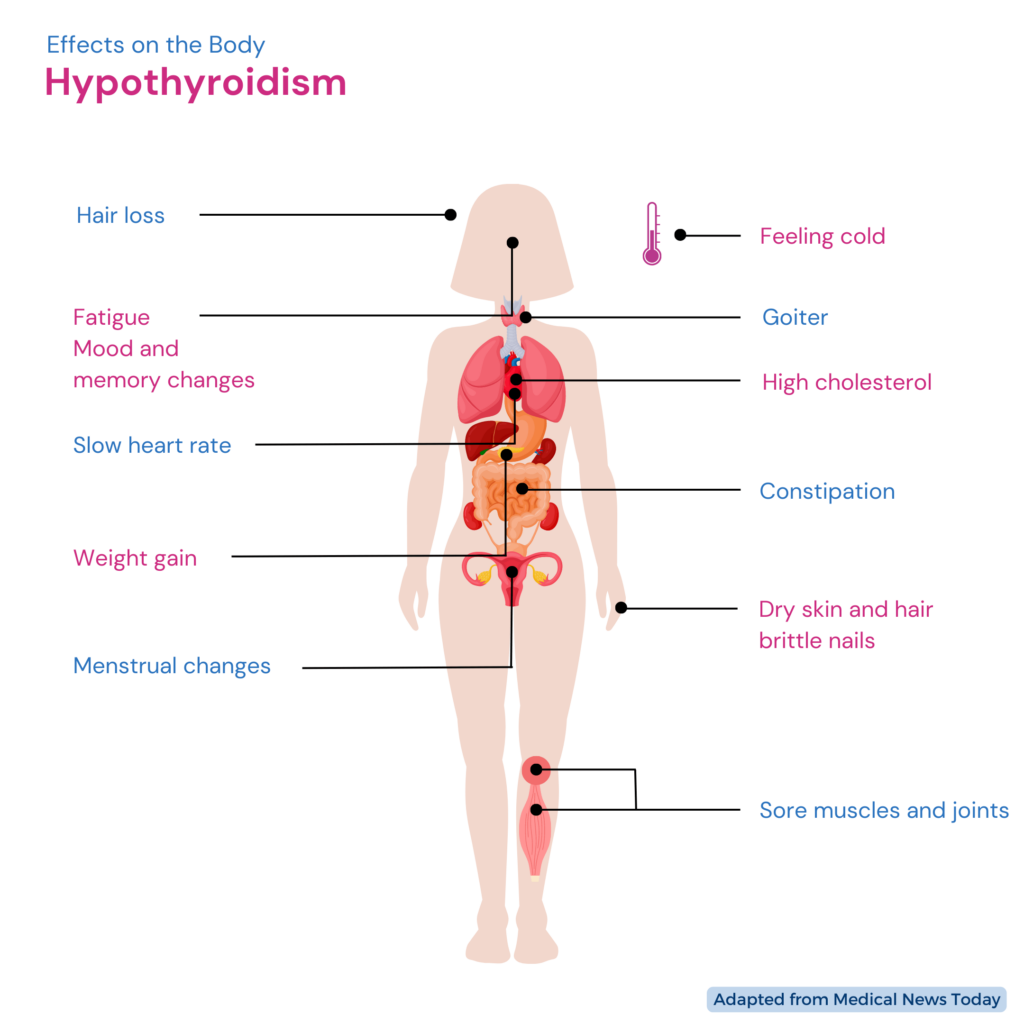
Both an overactive and a sluggish thyroid gland impact metabolism and may cause a variety of symptoms.
When the thyroid gland is underactive, it will release lesser quantities of T3 and T4 into the bloodstream.
This will slow down the body’s metabolism.
Women are more likely to develop hypothyroidism than men, and this condition is more common among people older than 60.
Other risk factors for hypothyroidism include:
The symptoms of hypothyroidism vary from person to person, but a few common symptoms of this condition are:
While not many know, alcohol consumption affects the thyroid gland and may result in hypothyroidism.
The thyroid gland is regulated by the hypothalamic-pituitary axis located in the brain.
Any form of substance abuse, including drugs and alcohol, has a direct suppressive effect on this axis.
This suppressive effect is also observed in the thyroid, which forms a part of the hypothalamic-pituitary-thyroid (HPT) axis.
Several studies have shown that the effect of alcohol on the HPT axis and thyroid functioning is significant.
The exact mechanism of how alcohol consumption affects thyroid function is unclear, but it may have a suppressive effect on the gland.
One suggested mechanism for the same is that alcohol causes cellular toxicity (toxicity caused due to the action of external agents on living cells), resulting in the suppression of thyroid function.
There is some evidence that consuming alcohol suppresses the HPT axis, which in turn reduces the production of Thyroid Stimulating Hormone (TSH).
Reduced TSH also means a reduction in the production of T3 and T4 from the thyroid gland.
Research also suggests that during alcohol withdrawal, peripheral thyroid hormones, i.e., T3 and T4, are suppressed.
The degree of suppression is associated with the severity of withdrawal.
This thyroid suppression may increase withdrawal dysphoria and increase the risk of relapse in people with alcoholism.
The pituitary gland located in the brain produces thyroid-stimulating hormone (TSH).
TSH regulates the production of T3 and T4, which require iodine.
Since alcohol causes cellular toxicity on the thyroid cells, consuming it may suppress thyroid function and reduce thyroid volume.
A study found that T3, T4, and TSH levels were low in people who consumed alcohol for 20 years.
Depending on your alcohol metabolizing genes, the effect alcohol has on one’s body can be different from that of others. Learning about these genes can help you understand your alcohol tolerance and reduce the risk of side effects and health hazards of alcohol.
Alcohol Flush: Red Face After Drinking? Here's Why
There are some studies on how alcohol consumption affects thyroid cancer.
These findings may be because alcohol prevents the effect of rapid TSH production on the thyroid follicular cells, thereby reducing cancer risk.
However, more studies are required to conclusively prove that alcohol has a protective effect on thyroid cancer.
Since alcohol consumption slows down thyroid function, it is always recommended to practice abstinence if you are taking medication for thyroid problems.
Though there are no known interactions between commonly used thyroid medications and alcohol, these substances alter thyroid function.
Therefore, to allow your thyroid to regain its normal functioning, follow your medication prescription and quit alcohol.
Despite the ill effects of alcohol on the thyroid gland, a treatment called alcohol ablation therapy (percutaneous ethanol injection or PEI) is used in thyroid cancer treatment.
This treatment helps destroy cancer cells that reoccur and those which spread to lymph nodes without surgery.
PEI is also used to shrink large fluid-filled thyroid nodules and cysts.
During this procedure, ethanol is directly injected through a needle or catheter.
The side effects and complications of this treatment are found to be minimal.
Have you ever experienced a sudden and unexplained pain in your back?
While incorrect posture and a sedentary lifestyle can explain the pain, there is another surprising cause for your back pains!
Stress.
Our muscles tense up unconsciously when we are under pressure.
This can cause muscle inflammation and soreness in various parts of our bodies, such as the neck, shoulders, and back. If left unattended over time, this condition can worsen into an endless cycle of pain.
So, if you're dealing with back pain, it's time to examine your stress levels more closely and discover ways to manage them effectively.
Let's explore some strategies to help you break the stress and back pain cycle.
It can disrupt various systems within our body, resulting in discomfort and prolonged health issues.
The following are some ways that stress may impact our bodies:
'Stress-related' back pain is the idea that psychological and emotional factors significantly impact the condition.
A well-known physician and professor of physical medicine and rehabilitation at New York University have also introduced a widely-accepted concept regarding stress-induced back pain called 'Tension Myositis Syndrome (TMS).'
He believes that psychological and emotional elements could be the sole contributing factors to back pain.
There are a bunch of studies that support this theory. Let’s have a look at some:
There are several theories on why stress can cause or worsen back pain. For example, stress can cause muscle tension, leading to pain and discomfort in the back. Additionally, stress can affect the body's inflammatory response, which may contribute to pain.
While, in some instances, physical health conditions could be responsible for chronic back pain, it is evident from these studies that any kind of emotional distress, including stress, is a significant risk factor for back pain.
However, at this point, it may be interesting to note that the relationship between stress and lower back pain may vary among individuals due to various factors, including the person’s genetic makeup.
For example, COMT is a gene that influences how people react to stress. This gene comes in 3 variants:
So, depending on their genetic makeup, even if two people are under the same stressful conditions, they may respond differently to stress.
Gene changes or variations can also affect an individual's pain perception and the response to and effectiveness of pain medication.
Therefore, incorporating genetic information can lead to personalized treatment plans and better management of this condition.
Stress-related back pain is increasingly recognized with different symptoms and treatment considerations.
The overall characteristics of stress-related back pain include symptoms such as:
In many stress-related back pain cases, patients complain of the pain 'moving around.'
Pain connected to stress can differ in duration based on numerous elements, including discomfort and the person's reaction to strain.
Unaddressed stress-related back pain can result in enduring distress, thus making it paramount to secure medicinal attention if you think your back ache is due to strain.
Stress-induced back pain can be relieved through various methods.
Here are some tips that can help:
Stress-related back pain is a growing concern for many individuals today.
However, it can be relieved through various methods, including stress reduction techniques, regular exercise, stretching, good posture, and ergonomic workstations.
If you suspect your back pain is stress-related, seeking medical advice to rule out other possible causes is recommended.
A healthcare professional can create a treatment plan considering physical and emotional pain. This may include exercises, physical therapy, and stress management techniques.