While for some, not going a day without coffee can cause headaches and dizziness, for a few others, ironically, consuming coffee can cause dizziness. Interesting right? Among other things, our genes play an important role in how our body responds to caffeine - whether it may benefit or harm your health. This article discusses how caffeine may cause dizziness and offers an in-depth guide to how you can moderate your caffeine intake according to your genetic type.
Caffeine is a CNS (central nervous system) stimulant, making us feel energetic and less sleepy upon consumption.
To facilitate this, caffeine does several things to the body:
Here are a few ways by which caffeine might lead to dizziness:
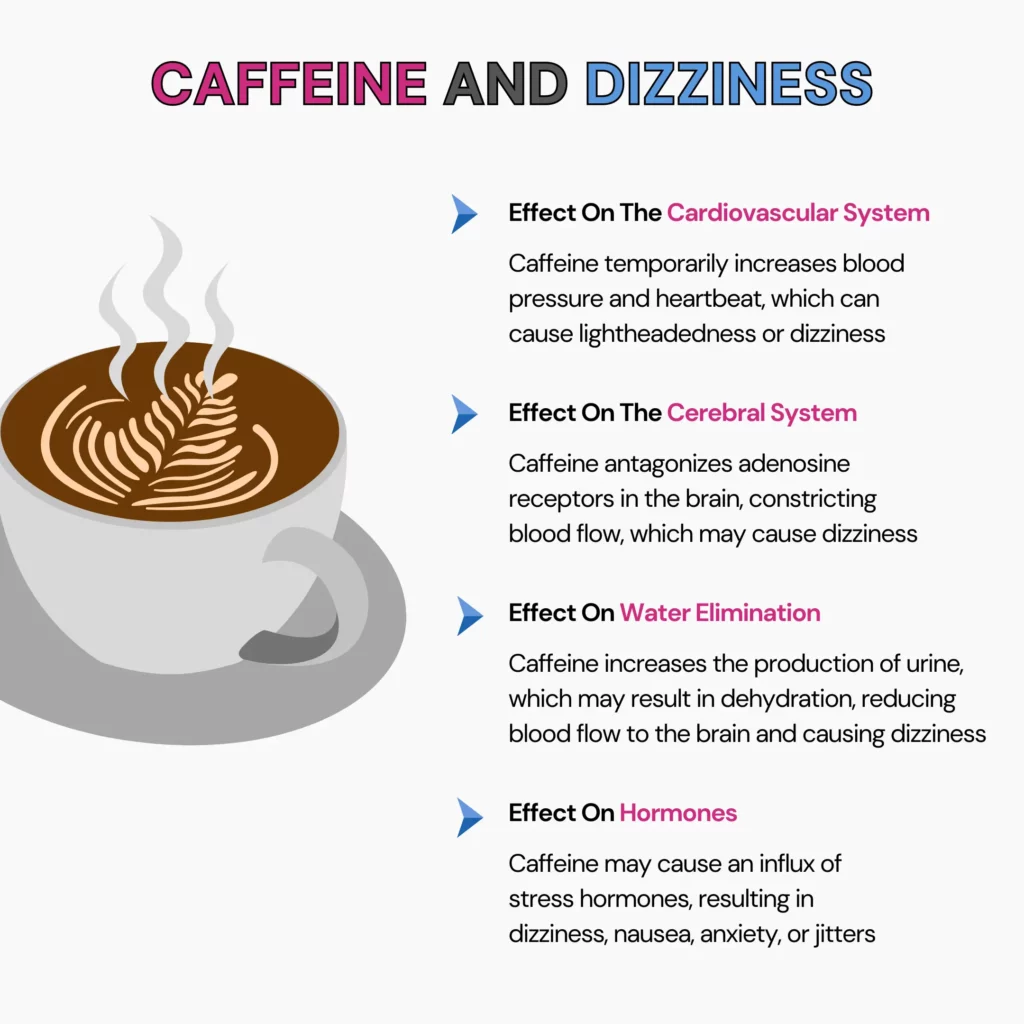
One major pathway by which caffeine can mediate the dizziness effect includes its effect on the cardiovascular system.
Caffeine intake increases blood pressure and heartbeat.
This causes changes in blood flow throughout the body, especially to the brain, which can cause lightheadedness or dizziness.
Caffeine antagonizes adenosine receptors in the brain, constricting blood flow.
This may cause some people to experience dizziness when caffeine is consumed.
Caffeine has a diuretic effect, which increases the production of urine.
Dehydration causes a pressure drop in the body, which reduces blood flow to the brain and may cause dizziness.
Caffeine intake may cause hormonal influx for stress responses, resulting in undesirable side effects like dizziness, nausea, anxiety, and jitters.
Caffeine can affect the cardiovascular system, cerebral blood flow, water elimination, and stress hormone levels. These factors can lead to increased heart rate, blood pressure changes, and reduced brain blood flow, triggering lightheadedness or dizziness.
Caffeine can make us awake and alert as a stimulant, but it can either narrow or swell blood vessels in the brain.
The latter might result in inflammation, which can also expand to nearby tissues, triggering headaches.
Caffeine can also lead to dehydration, which can also be a reason for lightheadedness.
People addicted to caffeine find it challenging to cut down on caffeine.
When a person stops or cuts consuming caffeine then, the very first symptom of caffeine withdrawal is a headache.
Other symptoms, such as tiredness, irritability, and difficulty concentrating, usually accompany caffeine withdrawal headaches.
The FDA has recommended 400 milligrams per day for healthy adults, and it is not associated with any dangerous or adverse effects.
However, this varies with people and how fast they metabolize it when consumed.
Pregnant women should limit their daily caffeine intake to 200 milligrams or less.
Caffeine sensitivity is the degree to which an individual reacts upon caffeine intake.
It varies with person and is influenced by factors like genes, metabolism, age, sex, and the frequency of consumption.
| Metabolizer Types | Recommended Caffeine Intake Per Day |
| Slow metabolizer | 100 mg or up to 1 cup of coffee |
| Moderate metabolizer | 200 mg or up to 2 cups of coffee |
| Fast metabolizer | 400 mg or up to 4 cups of coffee |
People with caffeine sensitivity can metabolize caffeine more slowly than normal people as the adrenaline rushes immediately when they consume it.
Symptoms of consuming higher amounts of caffeine may include:
Consuming too much caffeine can result in
Genes And Caffeine Report
A personalized guide on your body’s relationship with caffeine. Learn if your risk for various health and wellness traits directly linked to caffeine.
Accepted raw data formats: 23andMe, Ancestry DNA, Family Tree DNA, Living DNA, MyHeritage DNA and more.
Stay hydrated: Drinking plenty of water can flush out caffeine and neutralize the diuretic effect of caffeine.
Reduce your caffeine intake: Gradually reduce caffeine intake without an immediate stop.
Try alternatives: Caffeine-containing foods can be replaced with noncaffeinated foods, or if they can’t be avoided, try a darker roast, which contains less caffeine.
Physical movements: Exercising can improve caffeine-induced dizziness. Involving HIIT workouts is not necessary. However, slow movements like yoga or breathing exercises may also help with dizziness.
Eat fiber-rich foods: Fibres can slow down your caffeine absorption. Including fiber-rich foods can help reduce caffeine-induced dizziness.
Caffeine can cause dizziness either by blocking adenosine receptors, or by increasing heart rate, or as a diuretic agent, which leads to dehydration
In addition to its effects on the cardiovascular and cerebral systems, sensation also includes an individual’s sensitivity and hormonal fluctuations
Caffeine can make your head feel weird due to its potential to cause dehydration and withdrawal symptoms
The FDA has recommended a maximum of 400 milligrams of caffeine per day for healthy adults, which also reduces slow metabolizers and pregnant women
Managing caffeine dizziness involves staying hydrated, reducing intake, choosing alternatives, engaging in physical activity, and eating fiber-rich foods

Can Lack Of Sleep Cause Nausea? Know How To Prevent It

How Much Caffeine Is Safe During Pregnancy?

The Coffee Nap Phenomenon: Fad or Fact
https://www.livestrong.com/article/443182-does-caffeine-cause-dizziness
https://www.medsafe.govt.nz/profs/puarticles/caffeine.htm
https://www.fda.gov/consumers/consumer-updates/spilling-beans-how-much-caffeine-too-much
https://www.healthline.com/health/caffeine-sensitivity#hyposensitivity
Marine life holds many secrets to health and wellness. It is, therefore, no surprise that algae and seaweed are being increasingly consumed worldwide today. Another sea vegetable that is harvested for use as a health supplement and as a thickening agent is sea moss. If you’ve heard about sea moss gummies and are wondering how to use them or if you should try them, we’re here to help you! Let’s explore all about sea moss gummies– nutrients, health benefits, and more in this blog!
Sea moss, or Chondrus crispus, is also known by many names, including Irish sea moss and red seaweed.
It grows on the Atlantic coasts between Europe and North America and in many different colors.
It can be consumed in various ways. While sea moss is also available in powder, gel, and pill form, the gummy has taken off!
Like many marine vegetables, sea moss contains several vitamins and minerals.
They are naturally low in fat, calories, and sugar.
They also have a small amount of plant protein.
According to the US FDA, 10 g of sea moss contains the following nutrients:
| Nutrient | Quantity |
| Calories | 4.9 |
| Protein | 0.2 g |
| Fat | 0 g |
| Carbohydrates | 1.2 g |
| Minerals | |
| Calcium | 7.2 mg |
| Magnesium | 14.4 mg |
| Phosphorous | 15.7 mg |
| Potassium | 6.3 mg |
| Iron | 0.9 mg |
| Zinc | 0.2 mg |
Due to the nutrients in sea moss gummies, they are used in health supplements and offer many benefits.
Let’s take a look!
Preliminary research suggests that seaweed and sea moss improves immunomodulation and immune response.
However, more research is required in humans to prove this.
Plant compounds present in some marine vegetation may help fight cancer.
Research published in Cancers reports that fucoxanthin, which is abundantly found in some algae, helps fight specific markers of colorectal cancer or reduce risk factors.
Seaweeds and sea moss are good sources of probiotic bacteria and fiber, which ensure a healthy gut microbiome.
Sea moss is rich in fiber and probiotics, which help maintain a healthy gut.
These create a favorable environment for digestion, relieve constipation, and help cleanse the gut easily.
Seaweed, including sea moss, is rich in dietary fiber, minerals, and vitamins.
These nutrients reduce blood pressure, serum lipids, fatty acids, and blood glucose– all known risk factors for cardiovascular diseases.
Consuming sea moss may help lower your risk for cardiovascular diseases.
Seaweed contains iodine, which is required for thyroid health and function.
So, consuming sea moss may help regulate your thyroid hormones.
*Many of these benefits are still under research and have not been proven conclusively. Please talk to your healthcare practitioner for more information on this and whether it is the right option for you.
There’s a lot of discussion about using sea moss gummies for weight loss.
In a 12-week study, 78 adult volunteers took 1 g (1000 mg) of red seaweed extract daily.
They noticed a significant reduction in total body fat mass and body weight compared to the placebo group.
Another study published in 2015 noted that fucoxanthin, present in seaweed, can break down fat and cause weight loss.
While these studies show the promising effects of sea moss on weight loss, more research is needed to prove this conclusively.
While the potential benefits of sea moss gummies seem exciting, eating them has a few side effects. Let’s take a look!
A component found in seaweed, called poligeenan, may cause the following side effects:
Consuming sea moss in excessive quantities may increase the risk of side effects.
People who should avoid sea moss are:
Here are a few things to remember when taking sea moss gummies:
You may take sea moss gummies daily, but only after consulting your doctor.
Excessive consumption of sea moss can result in gastrointestinal disturbances, increased iodine intake, and, subsequently, thyroid disorders.
You may begin to feel the benefits of sea moss in as little as two weeks after taking it.
However, it may take 3 to 4 weeks before you begin to see the full effects of the supplements.
There is no prescribed time when you should take sea moss supplements.
Ask your doctor about what suits you best.
With the growing popularity of sea moss gummies, there are many brands to choose from.
However, if you choose to prepare your own, here’s how to do that:

Should You Take DGL Supplements For Treating Acid Reflux?
Are Postbiotics Better Than Probiotics For Gut Health?

Is BRAT Diet With Peanut Butter Good For Diarrhea?
Nicotinamide mononucleotide (NMN) is a naturally occurring fountain of youth. It is rapidly gaining popularity as a quick fix for conditions associated with aging, like slower metabolism and poorer skin health. In this article, we investigate this wonder molecule. Is it a magical anti-aging solution? Is there sufficient evidence to support this claim? Read on to find out what NMN is, whether it’s okay to consume, and what NMN benefits could look like.
Nicotinamide mononucleotide (NMN) is a popularly researched nucleotide naturally occurring in the body.
Nucleotides are molecules that play many roles in the body, such as being part of the DNA.
It is a precursor to nicotinamide adenine dinucleotide (NAD), an essential molecule found in every cell in the body, which is known to slow down aging.
Many enzymes and proteins require NAD to perform their functions, including repairing and maintaining DNA. NAD provides energy in the body, helps growth and repair, and may be critical in slowing down the aging process.
Reduced energy levels are one of the many factors responsible for aging.
Increasing NMN intake increases the production of NAD, providing body cells with increased energy production. Taking NMN supplements to raise blood NAD levels naturally has several benefits:
The brain requires an adequate supply of oxygen and nutrients to function.
Studies suggest that NMN supplementation increases blood flow to the brain, improving cognition.
Restoring adequate circulation to the brain can help combat the onset of neurodegenerative conditions like dementia or Alzheimer’s disease.
Muscles lose their ability to regenerate and grow as a result of aging.
A study identified a transport molecule in the brain responsible for muscle health and studied its workings.
The study reported that this transporter could be modulated by reducing or administering nicotinamide mononucleotide.
Thus, NMN may reverse conditions like sarcopenia and improve muscle strength and endurance.
Mitochondria are cell organelles that convert food into energy.
They’re important for energy metabolism and the prevention of metabolic diseases.
Several studies have shown that increased NMN levels in the blood strongly correlate to healthy mitochondria.
Healthy hearts need a constant supply of energy, which comes mostly from mitochondria.
Problems with mitochondria are often seen in failing hearts.
NAD+ is an important molecule for mitochondrial function.
Since NMN is a precursor to NAD+ and can thus support heart health.
This was validated by a study where scientists induced mitochondrial failure to stress the hearts of mice.
Upon injecting NMN, they found that the body quickly converted it to NAD+.
NAD increased the ability of heart cells to work under pressure and slowed the rate of heart cell death.
It was also able to reduce scarring, another contributor to heart dysfunction.
Scientists have extensively studied the benefit of NMN in cancer therapy in rodents.
NMN immunotherapy has increased the efficacy of different therapies used in cancer treatment.
NMN has also been able to reduce the side effects of chemotherapy, such as heart damage and cognitive impairment.
A loss of NAD results in rapid degeneration of the eye's nerves. This may increase the risk of vision loss.
When NMN is replenished in the body, it prevents degeneration of the eye nerves.
A study showed that NMN could protect cells in the eye and reduce inflammation in people with dry eye disease.
Increased age may cause fertility issues in women, like irregular ovulation or implantation failures.
NMN has been shown to improve age-related decline in egg quality and number in female mice.
DNA codes accumulate damage as we age. Repairing DNA damage can prevent age-related diseases and impart an anti-aging quality.
NAD supports enzymes called sirtuins, the guardians of our healthspan.
Sirtuins play an important role in DNA repair by stabilizing telomere length, a sign of aging.
Studies have shown that feeding mice NMN activates sirtuins.
NMN also repairs DNA damage that occurs due to radiation and old age.
Hand-picked Article For You: The Ultimate Guide To Anti-inflammatory Diet + Food List PDF
NMN is the precursor of NAD.
The amount of NAD depends upon the NMN available in the body.
The major differences between NAD and NMN include:
| NMN | NAD | |
| Type | Nucleotide | Coenzyme |
| Function | Increases NAD levels | Regulates metabolism, cell health, circadian rhythm, and organ functioning. |
| Blood absorption | Better | Poorer |
| Effect on mental health | Less effective | More effective |
| Effect on physical health | More effective | Less effective |
NAD is involved in repairing, rebuilding, and protecting DNA from damage.
It has several health benefits, such as:
NAD levels decrease with age or stress, triggering the aging process.
Low NAD levels increase your risk for health conditions like type 2 diabetes, Alzheimer’s, and heart disease.
NAD is sometimes called the ‘fountain of youth’ as it can potentially reverse the effects of aging at a cellular level.
The best way to increase NAD levels is to increase the intake of NMN.
Supplements are popular ways to increase NMN levels in the blood.
NMN occurs naturally in a few dietary sources, such as
Small amounts of NMN also occur in cucumbers, cow milk, and edamame.
The gut readily absorbs NMN. However, more research can help understand how increased NMN intake increases NAD levels in the blood.
If you’re considering NMN supplementation, please consult a medical professional to help make an informed decision.
Nicotinamide mononucleotide is safe. No side effects of NMN supplements have been reported in humans so far.
A long-term study of NMN effects on rodents shows no side effects or toxicity.
A study of NMN in humans shows no safety concerns after administering oral doses of 100, 200, and 500 mg.
There were no changes in heart rate, blood pressure, blood oxygen levels, blood composition, or body temperature.
Hand-picked Article For You: Should You Consider Luteolin Supplementation?
NMN has practically no side effects in humans or animals.
Scientists generally agree that a daily dose of up to 1200mg is safe for human consumption.
NMN helps reduce harmful inflammatory molecules in your body.
Thus, over time, it could smoothen your skin, even out pigmentations, and help your face glow.
Different people will react at different speeds to NMN.
Noticeable changes like better endurance and skin health will only manifest after a month.
You can enjoy its long-term benefits, like DNA repair and cell rejuvenation over the months and years.
Nearly 70 million Americans aren’t getting the sleep they need. Irritability, fatigue, and a foggy mind are the most recognizable symptoms of sleep deprivation, but their effect on our digestive health is equally impactful. A persistent lack of sleep can cause nausea. This fact underscores the importance of quality sleep beyond our mood and emotions for our general well-being. This article will investigate the link between inadequate sleep and the sensation of nausea and practical tips to combat and prevent it. Read on to learn how a good night’s sleep can be crucial for your overall health.
Getting a good night’s sleep benefits your gut health.
A lack of sleep or insomnia can have severe effects on your gut, including nausea.
Nausea is the feeling of being sick to your stomach and having the urge to vomit.
Here are a few ways in which sleep disorders like insomnia affect your gut health:
Sleep deprivation is when a person has trouble falling or staying asleep.
While it is usually temporary, having trouble sleeping could become a long-lasting chronic problem.
Some common causes of poor sleep are:
Genes And Sleep Health
Some people feel refreshed with just 6 hours of sleep, while others feel drowsy even after sleeping for 9 hours. While you may be all about the morning jog, your friend’s day might not even start till noon! Like hair or eye color, sleep traits may also be associated with genetics. Understanding the genetic basis of sleep helps highlight certain factors that could affect the quality and quantity of sleep. Using your ancestry test DNA data, you can unlock more than 15+ important aspects of health. Learn more.
Nausea can result from stress, current health conditions, or medications you currently take.
Recent studies have found a connection between sleep deprivation and nausea.
Lack of sleep directly affects the digestive system and the body’s immune response, leading to hormonal imbalances.
All these factors collectively make you feel nauseous.
When you are sleep-deprived, your body’s immune system starts to work overtime, releasing proteins called cytokines.
Cytokines cause tissue inflammation all over the body, including your digestive organs, leading to nausea.
Another effect of sleep deprivation is a changed appetite.
You start to crave oily foods or caffeinated drinks to counter the exhaustion from a poor night’s sleep.
These foods can inhibit digestive enzyme production, deplete beneficial gut bacteria, and inflame your stomach lining further.
These gastrointestinal issues can make you feel nauseous.
Lack of sleep causes problems with regular hormone release.
When you are short on sleep, you feel exhausted and stressed.
Stress stimulates the hypothalamus in your brain to release a corticotropin-stimulating hormone (CRF).
Too much CRF in the body can cause gastrointestinal issues.
It can cause spasms in the upper stomach muscles, making you nauseous.
Thus, nausea tends to occur with insomnia.
The constraints of sleep deprivation are subjective.
Most definitions of sleep deprivation vary:
Hand-picked Article For You: Sleep Issues - Why Do I Keep Waking Up At 4 AM?
Long-term or chronic lack of sleep can cause problems with your overall health.
Some of these include:
Here are a few simple ways to deal with lack of sleep-induced nausea:
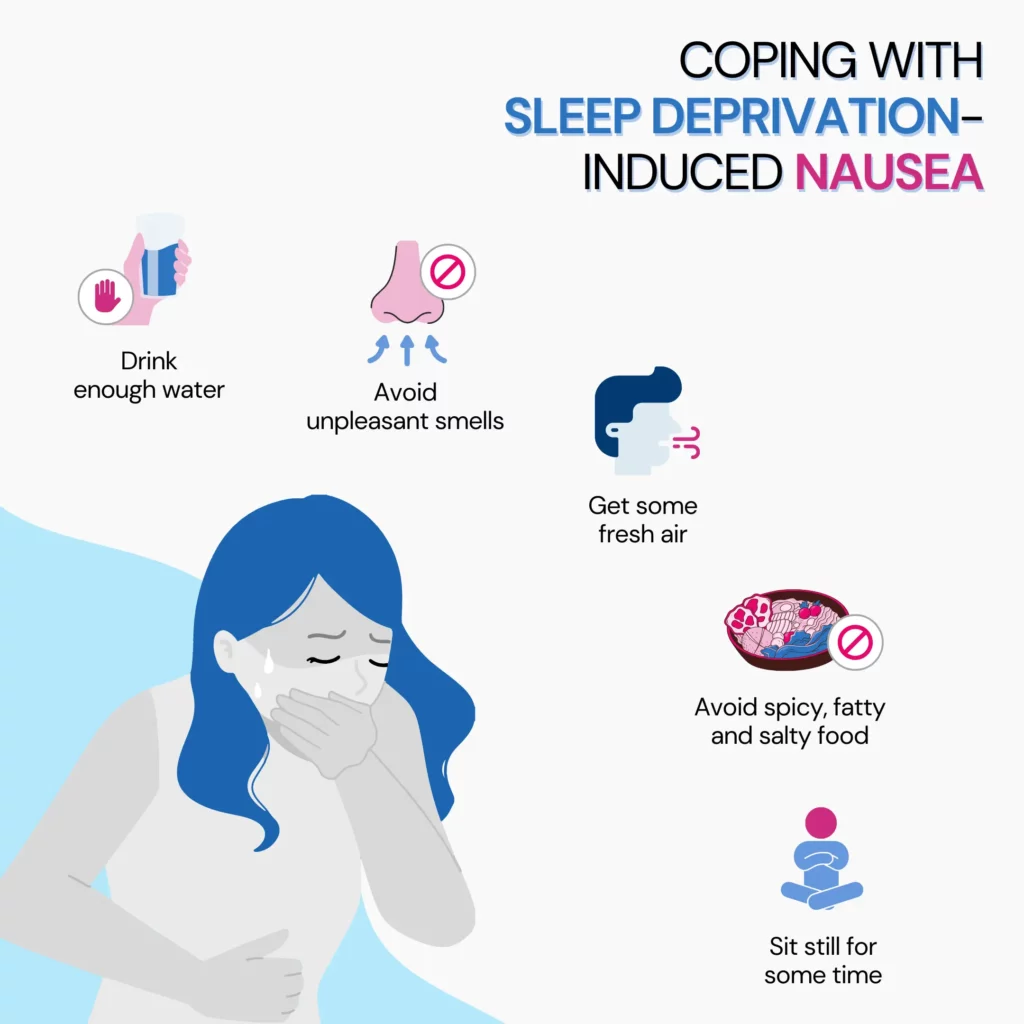
Better sleep hygiene can improve sleep quality and help counter sleep deprivation.
Here are some steps to get more quality sleep:
People Are Reading The Top 3 Methods To Fall Asleep Faster
Although no clear limit has been discovered yet, the longest a human has stayed awake continuously is around 264 hours, roughly 11 days. Most people start experiencing adverse symptoms within just two or three days without sleep.
In a sleep deprivation study performed on animals, a significant accumulation of harmful molecules in their gut eventually proved fatal.
Since we know that sleep deprivation tends to affect the gut in humans as well, this could explain the link between sleep disorders and several diseases that result from it.
Due to its sugary nature, Sprite is better received by people with nausea.
It can sometimes help settle a nauseous stomach, but its sugar content can affect your gut bacteria.
It’s better to consume less sugary drinks like coconut water, chamomile tea, or cooking broths.
https://www.sleepfoundation.org/physical-health/can-lack-of-sleep-cause-nausea
https://www.health.com/sleep-deprivation-8364530
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5385214
https://www.nhlbi.nih.gov/health/sleep-deprivation
https://www.sleepfoundation.org/physical-health/lack-of-sleep-and-diabetes
https://pubmed.ncbi.nlm.nih.gov/18564298
https://www.healthline.com/nutrition/what-happens-if-you-eat-too-much-salt
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8950745
https://www.healthline.com/health/healthy-sleep/how-long-can-you-go-without-sleep
https://brain.harvard.edu/hbi_news/why-severe-sleep-deprivation-can-be-lethal/
https://www.medicalnewstoday.com/articles/is-sprite-good-for-stomach-flu
One remedy for PCOS that is increasingly gaining attention is spearmint tea. Renowned for its refreshing flavor and health benefits, spearmint tea is being studied for its anti-androgenic properties, which could benefit women with PCOS. Could this common herbal tea be a game-changer in managing PCOS symptoms? This article delves into the scientific research, potential benefits, and practical considerations of incorporating spearmint tea into your daily routine.
PCOS (polycystic ovary syndrome) is a prevalent condition affecting women of reproductive age.
It usually starts in adolescence, with symptoms that can change over time.
Although PCOS is a chronic condition with no known cure, various treatments can help manage and alleviate its symptoms.
Lifestyle changes like regular exercise and a healthy diet can be helpful.
The exact cause of PCOS remains unknown, but a family history of PCOS or type 2 diabetes can increase a woman's risk, suggesting a potential genetic or metabolic link.
Spearmint tea demonstrates potential efficacy in managing PCOS symptoms, possibly due to its anti-androgenic properties.
These properties could help reduce elevated levels of androgens commonly associated with the condition.
Research indicates that spearmint has promising effects on managing PCOS symptoms. Here's what various studies have shown:
In a 2010 study, the effects of spearmint oil on PCOS were evaluated in rats.
The rats were divided into eight groups:
Rats in groups II, III, IV, and V were induced with PCOS using letrozole.
The results showed that spearmint oil reduced body weight, testosterone levels, ovarian cysts, and atretic follicles in PCOS rats.
Additionally, it increased the number of Graafian follicles, indicating a restoration of ovarian follicles.
Another recent study in 2020 assessed the impact of a combination of spearmint and flaxseed extracts on PCOS-induced rats.
24 rats were randomly divided into four groups:
Results
The treatment group witnessed:
A 2010 study in Turkey investigated the anti-androgenic properties of spearmint tea in women with PCOS and hirsutism.
42 volunteers were randomized to drink spearmint tea or a placebo twice daily for a duration of 30 days.
Study Design and Methodology
Study Results
The preliminary findings are encouraging, suggesting spearmint tea could be a helpful and natural treatment for hirsutism in PCOS.
The time it takes for spearmint tea to balance hormones can vary.
Some studies have shown that drinking spearmint tea twice daily for a month can lower testosterone levels in individuals with PCOS.
At the same time, LH and FSH levels increased compared to those who consumed a placebo.
Other research indicates that improvements can be seen as soon as five days. The effectiveness often depends on initial hormone levels.
Those with slightly elevated testosterone might see quicker results, while significantly higher levels may require additional treatments.
Hand-picked Article For You: Is PCOS An Autoimmune Disease?
Spearmint tea offers various health benefits beyond its minty flavor. Here are some key advantages:
Research shows that drinking 2-3 cups of spearmint tea daily can alleviate some symptoms of PCOS.
It is particularly effective in reducing elevated androgen levels and the severity of hirsutism (excessive hair growth).
While it holds promise for balancing hormones, individual responses may vary.
While spearmint tea is popular for its refreshing flavor and certain health advantages, excessive use can have several side effects. These include:
Others Are Reading: Top Five Teas For Better Gut Health In 2024
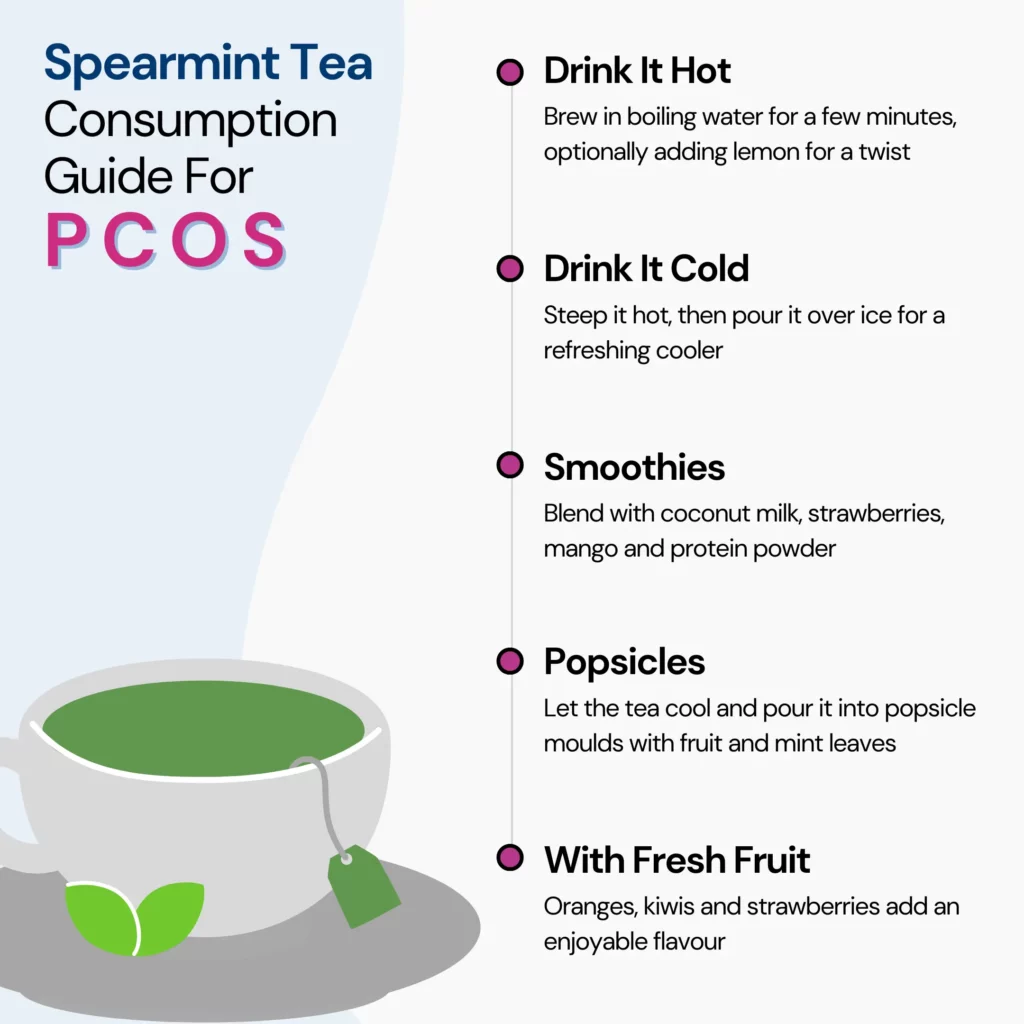
Here are some easy ways to enjoy spearmint tea for PCOS:
Daily consumption of spearmint tea is generally safe for most people, with minimal risks reported by experts.
However, those who are pregnant, breastfeeding, or have certain health conditions should consult their healthcare professionals. This is important to ensure spearmint tea won't adversely affect their condition.
As always, moderation is key; starting with small amounts is wise if in doubt.
Spearmint tea could potentially benefit fertility by aiding in the balance of FSH and LH levels.
In a study where women drank 2 cups daily for 5 days, there was a notable increase in LH, FSH, and estradiol.
Nevertheless, the current evidence is limited, and more research is required to fully assess spearmint tea’s effectiveness in improving fertility, especially among those with PCOS.
Spearmint tea has been consumed on an empty stomach for centuries, particularly for its potential digestive benefits.
Traditional practices often involve drinking herbal teas, including spearmint, first thing in the morning to stimulate digestive processes. Many people also enjoy the refreshing taste it leaves in the mouth.
Spearmint tea shows the potential to lower androgen levels and ease PCOS symptoms like hirsutism due to its anti-androgenic effects.
Both animal and human studies suggest spearmint tea can lower testosterone levels and improve hormonal balance, but more research is needed for definitive conclusions.
Drinking 2 cups of spearmint tea daily may be effective in managing PCOS symptoms, but individual responses can vary.
Spearmint tea also offers other health benefits, including hydration, antioxidant support, improved digestion, and potential memory enhancement.
It is generally safe for most people, but those who are pregnant, breastfeeding, or have specific health conditions should consult with a doctor before regular consumption.
Spearmint tea should be considered as part of a broader lifestyle and treatment plan for PCOS rather than a standalone solution.
https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5788221
https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-020-00633-8
https://pubmed.ncbi.nlm.nih.gov/19585478
https://pubmed.ncbi.nlm.nih.gov/17310494
https://www.webmd.com/diet/spearmint-tea-health-benefits
https://medlineplus.gov/druginfo/natural/845.html
https://health.clevelandclinic.org/spearmint-tea-benefits
https://onlinelibrary.wiley.com/doi/10.1002/ptr.2074
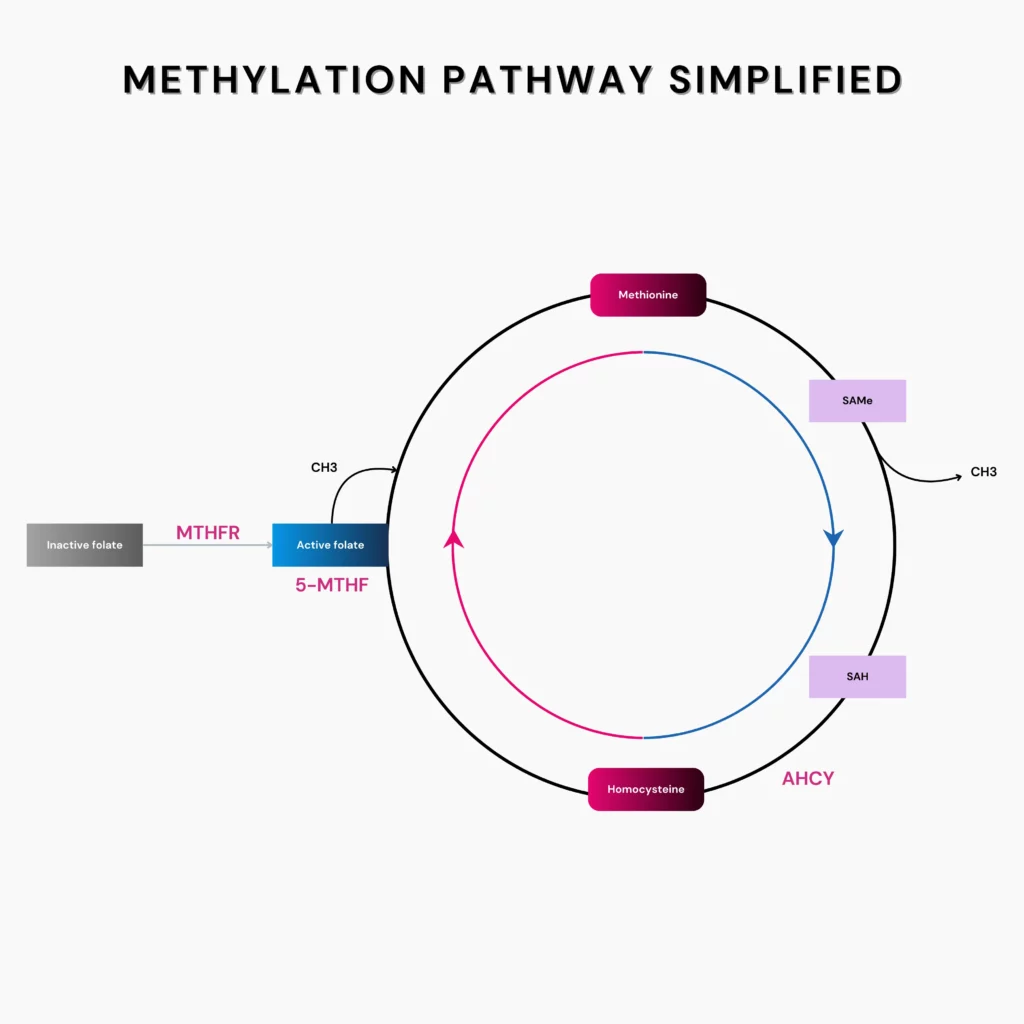
Methylation, simply put, is the addition of methyl (CH3) group to a molecule - it can be an enzyme, a hormone, or the DNA itself.
The methylation cycle encompasses a bunch of biochemical reactions that transfer methyl groups from one molecule to another - essentially like a game of passing the parcel.
Methylation is important for several functions in the body, including:
An important reaction in the methylation cycle is the conversion of an amino acid called homocysteine to another amino acid called methionine.
The buildup of homocysteine in the body has been associated with several health conditions like:
Use your ancestry test raw DNA data to get Xcode Life's Updated MTHFR and Methylation Report
$50 $30
| Gene | Description |
| MTHFR | The MTHFR gene produces the methylenetetrahydrofolate reductase enzyme. It converts folate into its active form. This is crucial for converting the harmful amino acid homocysteine to methionine, which is safe for the body. Two common variants in this gene are C677T and A1298C, which can lead to MTHFR enzyme activity and increased homocysteine levels. |
| MTRR | The MTRR gene produces the methionine synthase reductase enzyme. It plays a role in activating another enzyme, methionine synthase (MTR). The MTR enzyme directly converts homocysteine to methionine. Variants in the MTRR gene can result in impaired reactivation of MTR, leading to a buildup of homocysteine and reduced methionine levels. |
| MTR | The MTR gene produces the methionine synthase enzyme. This enzyme is responsible for the final step in the conversion of the amino acid homocysteine to methionine. Variants in the MTR gene can result in a buildup of homocysteine in the blood and decreased availability of methionine and SAM, which can disrupt DNA methylation and gene expression. |
| MTHFD1 | The MTHFD1 gene produces the methylenetetrahydrofolate dehydrogenase 1 enzyme that catalyzes the 3-step folate metabolism pathway. This is an important step in generating methyl donors for the methylation cycle. Variants in this gene can alter the levels or activity of the enzyme produced, and can lead to disturbances in the methylation cycle. |
| CBS | The CBS gene produces the cystathionine beta-synthase enzyme. It is crucial in the transsulfuration pathway, a branch of the methylation cycle. The CBS enzyme catalyzes the first step of converting homocysteine into another amino acid called cysteine. Variants in the CBS gene can impair this conversion, leading to increased homocysteine levels. |
| AHCY | The CPS1 gene produces the carbomyl phosphate synthetase enzyme. It plays an important role in the urea cycle which converts excess ammonia in the body to urea. This cycle regulates neuronal health and oxidative stress. Variants in the CPS1 gene have been associated with higher homocysteine levels. However, the mechanism behind this is unclear. |
| CPS1 | The CPS1 gene produces the carbomyl phosphate synthetase enzyme. It plays an important role in the urea cycle which converts excess ammonia in the body to urea. This cycle regulates the neuronal health and oxidative stress. Variants in the CPS1 gene have been associated with higher homocysteine levels. However, the mechanism behind this is unclear. |
| BHMT | The BHMT gene produces the betaine-homocysteine S-methyltransferase enzyme. It transfers a methyl group from a compound called betaine to homocysteine to convert it into methionine. Methionine is then converted into SAMe. Variants in the BHMT gene can affect the enzyme levels or activity and may result in higher levels of homocysteine. |
| NOS3 | The NOS3 gene produces the endothelial nitric oxide synthase (eNOS) enzyme. It is responsible for the production of nitric oxide in the endothelial cells. Variations in the NOS3 gene have been associated with higher homocysteine levels. The hypothesis is that nitric oxide modulates homocysteine levels through an effect on folate catabolism. |
| SHMT | The MAT1A gene produces the methionine adenosyltransferase enzyme. The two forms of the enzyme, MATI and MATII, help break down methionine into S-adenosylmethionine, a main methyl donor. Variants in the MAT1A gene influence homocysteine levels. Some studies report increased levels in resposne to dietary fat intake in those who have a MAT1A variant. |
| CTH | The CTH gene produces the cystathionine-gamma-lyase enzyme. It catalyzes the conversion of cystathionine to cysteine in the last step of the transsulfuration pathway. Variations in the CTH gene can lead to plasma elevation of total homocysteine levels. This can lead to a condition called cystathioninuria, an inborn error of metabolism. |
| MAT1A | The MAT1A gene produces the methionine adenosyltransferase enzyme. The two forms of the enzyme, MATI and MATII, help break down methionine into S-adenosylmethionine, a main methyl donor. Variants in the MAT1A gene influences homocysteine levels. Some studies report increased levels in resposne to dietary fat intake in those who have a MAT1A variant. |
| GNMT | The GNMT gene produces the glycine N-methyltransferase enzyme. It transfers a methyl group from SAM to glycine to generate S-adenosylhomocysteine (SAH) and sarcosine. Variations in the GNMT gene can result in lower levels of the enzyme, which may cause homocysteine levels to build up. However, this effect can be countered with folate intake. |
| MAOA | The MAO-A gene produces the monoamine oxidase A enzyme. It is an integral enzyme in the regulation of brain chemicals like dopamine, norepinephrine, and serotonin. For MAO-A to function well, it needs to undergo optimal methylation. Undermethylation of MAO-A can result in dysregulation of brain chemicals and has been associated with panic disorder. |
| COMT | The COMT gene produces the catechol-o-methyltransferase enzyme. This enzyme transfers a methyl group from SAMe (a by-product of homocysteine to methionine conversion) to brain chemicals like dopamine and norepinephrine. Variants in the COMT gene may lead to imbalances in the brain chemicals, increasing the risk of certain psychiatric disorders. |
Here, we will break down the key sections of your report and provide answers to common questions.
The MTHFR report includes:
The report focuses on the following SNPs within the MTHFR gene:
Depending on the genotype for these SNPs, your overall results are calculated. If the bar graph points to green, you likely have normal MTHFR enzyme levels.
If it’s in orange, you may need to up your dietary vitamin B9 intake.
If it’s in red, you may require a methylfolate supplement (which should be taken only after consulting your doctor).
Other than MTHFR, several important genes regulate the methylation process in the body. This section provides information on their activity.
The colored circles around the genes denote how well they function.
Red and orange indicate the presence of risk alleles that interfere with the gene functioning and are associated with lower levels or activity of the enzyme produced by that particular gene.
Green denotes a normal functioning gene and hence is associated with normal enzyme levels/activity.
“SNPs ANALYZED" provides a comprehensive overview of the specific Single Nucleotide Polymorphisms(SNPs) present in the important methylation genes, which could affect the level/activity of the enzymes produced.
Sometimes, one copy of the variant allele may be shaded in green; this is because, in some SNPs, only two copies of the variant allele will likely have a negative effect. Single copy is still considered normal.
The * symbol indicates that the original SNP we analyzed was not found in your data, so a proxy SNP was used. Proxy SNPs are variants present very close to the original SNP and, hence likely will have the same effect on the gene activity.
"I've tried other websites when it comes to getting DNA and Xcode's reports and recommendations are way on point. I got the MTHFR and Caffeine report. My smartwatch has been telling me my energy level have been at an average of 15% with stress levels of 99%. After following my reports recommendation from Xcode, my energy levels went up to 63% and my stress levels went down to 50%. Definitely going to get all of the reports as soon as possible, in order to be the healthiest version of me possible. What a find this website was."
Based on your genetic variants, the following supplements may be beneficial:
Disclaimer
Before starting any new supplement regimen, it is crucial to consult with a healthcare provider. These recommendations are based on genetic predispositions and should be tailored to your individual health needs and circumstances. Your healthcare provider can help determine the appropriate dosages and monitor for any potential interactions with medications or other supplements you may be taking.
It is good practice to review your genetic information annually or when you experience significant health changes.
Absolutely. Sharing your report with your healthcare provider can help tailor medical advice and interventions to your genetic profile. In fact, we recommend taking the help of your doctor to interpret all our reports.
Genetic testing is highly accurate, but it is one piece of your overall health picture. It is essential to consider these results alongside other medical evaluations.
Your MTHFR report is a powerful tool for understanding your genetic predispositions and taking proactive steps toward better health. Use this guide to navigate your results and make informed decisions about your lifestyle and healthcare. If you have further questions or need assistance, don't hesitate to reach out to a healthcare professional.