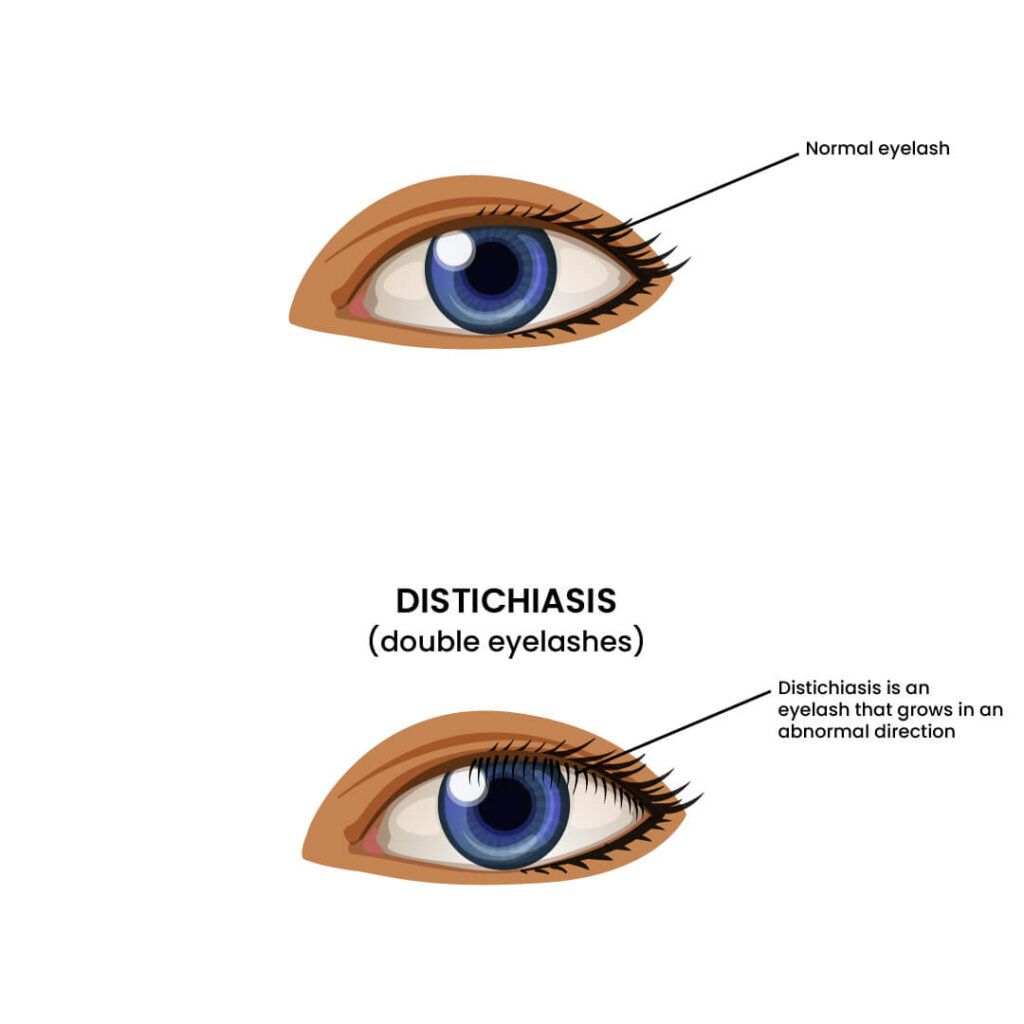
Double eyelash is a rare condition of having two rows of eyelashes in an eyelid.
It is medically termed Distichiasis and can affect both eyes.
An extra row of eyelashes is present on either the upper or lower eyelids (or both).
The meibomian gland is where the double eyelashes arise on each eyelid.
They are oil-producing glands that help lubricate your eyes.
It coats tears, which stops the eyes from drying up too quickly.
Common signs and symptoms of double eyelashes include:
The second row of lashes is typically lighter, shorter, and thinner than the first.
They can be either a whole set of eyelashes or one or two lashes on each eyelid.
Usually, lashes grow at the dry outer edge of the eyelid, but the extra lashes grow from the wet inner edge of the eyelid.
Estimates suggest that about 1 in 10,000 people have double eyelashes.
In distichiasis, an extra row of eyelashes is present.
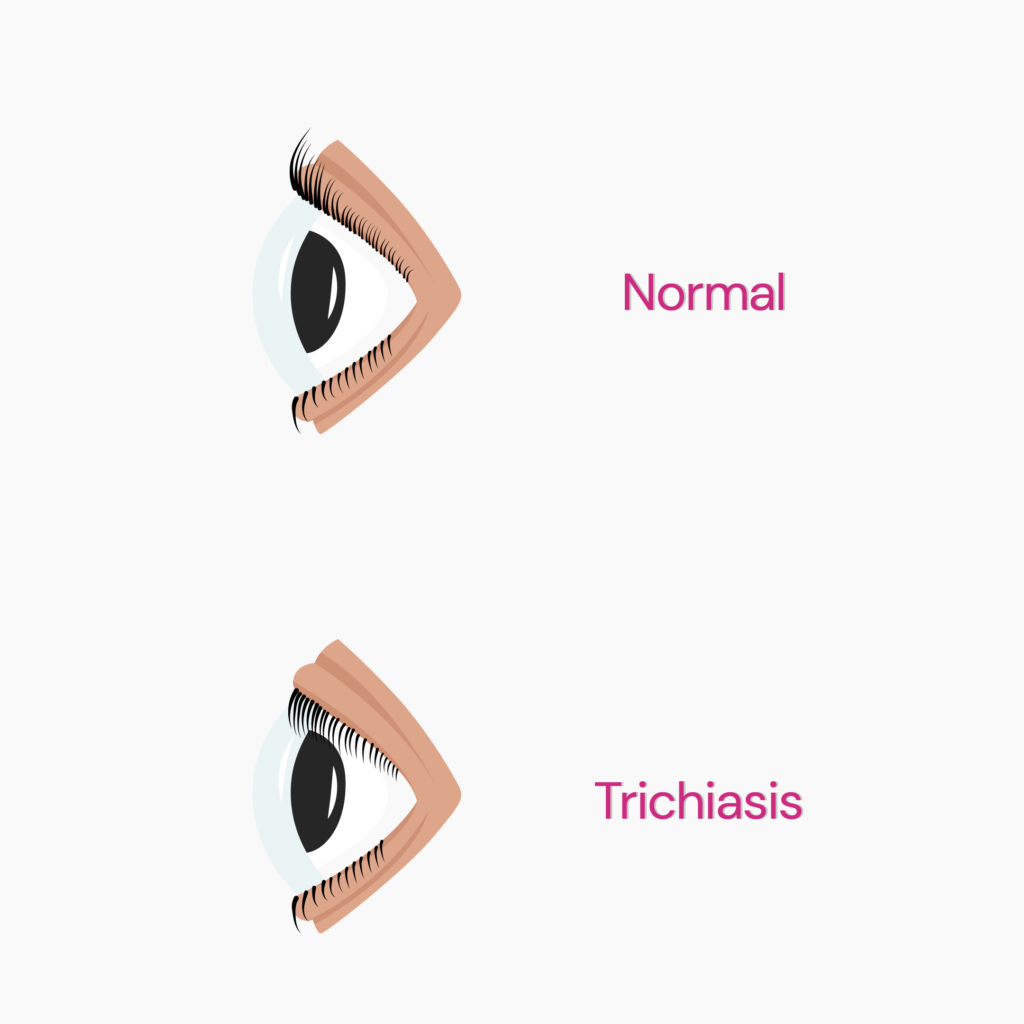
In trichiasis, there’s only one row of eyelashes, but instead of curving upwards, they curve downwards toward the cornea.
Unlike distichiasis, it is only acquired - in some cases, the cause is unknown, while in other it occurs secondary to conditions like Stevens-Johnson syndrome (SJS) or chemical burns.
| Distichiasis | Trichiasis | |
| What it is | Extra row of eyelashes | Only one row - lashes curve inward |
| Acquired or inherited | Both | Acquired |
| Causes | FOX gene mutations, certain medications, contact lenses | Secondary to other inflammatory conditions |
| Treatment | Epilation, electrolysis, and cryotherapy | Epilation, electrolysis, and cryotherapy |
The two main ways distichiasis can happen are:
Congenital distichiasis is when the disorder is present at birth.
Acquired distichiasis can be developed later in life.
Congenital distichiasis happens if epithelial cells of your eyes develop incorrectly or modify into a pilosebaceous unit.
The pilosebaceous unit, comprising the hair follicle, hair shaft, and sebaceous gland, makes the extra row of eyelashes.
Congenital distichiasis occurs when there is a gene mutation in FOXC2 (forkhead box protein C2) during conception.
The FOXC2 gene is involved in other inherited conditions besides distichiasis.
Acquired distichiasis develops when eyelids get injured or inflamed.
Here are some factors or conditions causing acquired distichiasis:
Lymphedema is a condition characterized by swelling of the legs due to the accumulation of fluid between the skin and muscles.
When a person has both lymphedema and distichiasis, it is called lymphedema distichiasis syndrome.
Some conditions that can co-occur with this syndrome include:
Double eyelashes can occur due to FOXC2 gene mutation.
The FOX (forkhead box) gene family consists of 21,418 protein-coding genes.
The FOX genome produces proteins called transcription factors that control how genes work.
Some transcription factors of the fox gene family are A1, A2, B1, C1, C2, D1, etc.
They play a role in cell aging, growth, and death, maintaining metabolism, and the development of different organs. The FOXC2 gene turns on and off many other genes during fetal development.
A rare genetic mutation of the FOXC2 gene on chromosome 16 causes distichiasis.
This mutation turns on excess transcription to cause a double row of lashes during prenatal development.
It can lead to droopy eyelids and yellowish nails.
Family History
Genetics is a prominent risk factor in developing congenital distichiasis.
You are more likely to inherit the condition if any of your parents have double eyelashes.
Age
Older people are more likely to develop eyelid disorders like ocular cicatricial pemphigoid (OCP) and meibomian gland dysfunction (MGD).
Sex At Birth
Females are more susceptible than males since they develop OCP quickly.
Eyelid Inflammation
Seborrheic dermatitis or dandruff on the scalp and brows increase the chance of developing swollen eyelids.
Other risk factors include allergies, bacterial infections, clogged oil glands on your eyelids, and eyelash mites or lice.
Certain Medications
Meibomian gland dysfunction (MGD) is more likely to occur in people who take glaucoma medication.
Stevens-Johnson syndrome (SJS) can affect people who take painkillers for gout, seizures, infections, and mental illness.
Lack Of Immunity
Immune-compromised people are at higher risk of developing eyelid disorders.
Use Of Contact Lenses
Contact lenses can irritate your eyes, which can lead to inflammation of the eyelids.
Double eyelashes associated with FOXC2 gene mutation can be dangerous as it is associated with other inherited conditions like lymphedema distichiasis syndrome (LDS).
A mutation in the FOXC2 gene causes an increased risk of congestive heart failure (supply of fluid to the heart instead of blood).
Congestive heart failure causes shortness of breath, leading to sudden death.
This condition is usually confirmed by a genetic test in a clinical setting.
Symptoms that could indicate LDS include:
You do not need medication if you are asymptomatic.
If you experience any symptoms, treatment will emphasize subsiding them.
It could also require removing the excess eyelashes.
The number of extra lashes and your symptoms will determine the best treatment.
Hydrating Eye Drops
Lubricating eye drops hydrate the eyes and can ease acute eye irritation.
It works by shielding the cornea from excessive lashes so as not to irritate.
Smooth Contact Lenses
Soft contact lenses offer a layer of defense similar to lubrication.
Ensure you use contact lenses correctly to avoid any problems.
Epilation
An epilator is used to remove the extra lashes.
It pulls out extra lashes physically from the eyelid.
It is a temporary solution because the lashes often grow back in two to three weeks.
People with few extra lashes can undergo epilation.
Cryotherapy
Cryotherapy detaches eyelash follicles from eyelids using extremely cold temperatures.
Although having few side effects, it has long-lasting results.
Cryotherapy may cause side effects like:
Electrolysis
Electrolysis is preferable to epilation for eliminating a few eyelashes.
A needle with a short-wave frequency is injected into the eyelash follicle.
During this process, the follicle is let loose from the eyelid.
Lid Splitting
One kind of eye surgery is lid splitting.
The eyelash follicles are visible when eyelids are split open.
Individually, the excess eyelashes are taken out.
Lid splitting is occasionally combined with electrolysis or cryotherapy.
Argon Laser Thermoablation
The lash follicles are repeatedly burned with an argon laser, removing the follicles.
During the procedure, you can feel uncomfortable and have an increased tear flow.
Distichiasis is double rows of eyelashes, and districhiasis is three rows of eyelashes.
Ectopic lashes or ectopic cilia are lashes that grow from abnormal places or in abnormal directions.
For example, lashes may grow from the conjunctiva or the pink part of the eye.
Double eyelashes or Distichiasis is a condition where an extra row of eyelashes is present.
It can be congenital distichiasis or acquired distichiasis, depending upon the cause.
A mutation in the FOXC2 gene causes congenital distichiasis.
The FOXC2 gene mutation leads to other inherited conditions like lymphedema-distichiasis syndrome (LDS) and congestive heart failure.
People with a family history of double eyelashes, eyelid inflammation, painkiller medications, and poor immunity are at high risk of developing the condition.
Double eyelashes is treated by argon laser thermoablation, cryotherapy, epilation, lid splitting, etc.
The average person consumes about 152 pounds of added sugar every year. That's about 22 teaspoons or 355 calories worth of sugar every day - way more than the American Heart Association's recommended limit of 6 teaspoons (100 calories) per day for women and 9 teaspoons (150 calories) per day for men. Many people are looking for ways to cut back on sugar, and one way is to use a sugar substitute. When it comes to sugar substitutes, there are many options to choose from. Two of the most popular substitutes are erythritol and xylitol. But which one is the better option? Here's a look at erythritol vs. xylitol to help you make the best decision for your needs.
The common white granulated sugar we see in bags or packets is sucrose.
Sugar substitutes are any sweet-tasting substances used to replace sugar in our diets.
They can be natural or artificial, and they are often sweeter than sugar.
Many people use sugar substitutes to help with weight loss or management, diabetes, and other conditions.
Although they may have some benefits, there are also some risks associated with their use.
Xylitol is a type of natural sugar alcohol found in plants, fruits, and vegetables.
While it is sweet and tastes like sugar, it doesn't damage teeth or cause decay.
It is popularly used in sugar-free gums.
Erythritol is also a sugar alcohol found naturally in plants and is one of the most commonly used artificial sweeteners.
It has been a popular choice for those with diabetes.
Hand-picked Article For You: Improving Glucose Response With Exercise
| Erythritol | Xylitol | |
| Calories/Gram | 0.24 | 2.4 |
| Sweetness (compared to white sugar) | 60-80% | 100% |
| Glycemic Index | 0-1 | 7 |
| Impact on blood sugar levels | None | Very mild |
| Diabetes-friendly? | Yes | Yes |
| Weight-loss friendly? | Yes | Yes |
| Digestive issues? | Rarely/Less | Diarrhea is a common side effect |
| After taste | Better aftertaste | Not as good as erythritol |
| Erythritol | Xylitol | |
| Diabetes | Diabetes-friendly as it helps decrease the amount of sugar absorbed whilst altering glucose metabolism. | With a glycemic index of 7, it doesn’t lead to spikes in glucose levels and may even improve glucose tolerance. |
| Weight Loss | Low in calories; replacing white sugar with this can reduce caloric intake and promote weight loss. | 40% lesser calories than white sugar; helps with reducing belly fat |
| Other Benefits | Can help scavenge free radicals and protect cells from oxidative damage | Prevents the growth of bacteria that cause tooth decay, promoting good oral health |
Erythritol: Most people should be able to consume erythritol without any discomfort. However, it can lead to nausea, abdominal distress, and other digestive symptoms in people who are sensitive to it.
Xylitol: High consumption of xylitol can lead to digestive disturbances, including diarrhea, owing to its laxative properties. People who already have digestive issues may face severe discomfort with xylitol. Further, xylitol is extremely toxic to pets, even in small amounts.
Both erythritol and xylitol are low-calorie sugar alcohols often used to replace sugar.
Digestive issues are higher with xylitol; however, this is observed only in larger doses.
Xylitol has better oral health benefits, but erythritol also prevents tooth decay to an extent.
In addition, erythritol has antioxidant properties, which are good for heart health.
In conclusion, erythritol has a small upper leg here with a lower risk for digestive issues and absolutely no impact on glucose levels.
But both these sweeteners are great options for replacing white sugar in your diet.
People often overlook how much their health is impacted by the kind of oil they use. Oils high in unsaturated fats can reduce the risk of heart disease, while those high in saturated or trans fats may increase heart disease risk. This article compares MCT oil vs coconut oil, both made from coconuts but with different health advantages. One provides rapid energy, while the other has several other health advantages. So which one should you be adding to your pantry?
Medium-chain triglyceride (MCT) oil is primarily derived from coconut and palm kernel oils but is also found naturally in dairy products such as cheese, yogurt, and milk.
Triglycerides are the primary type of dietary fat in our bloodstream. They consist of three fatty acids joined to a glycerol molecule.
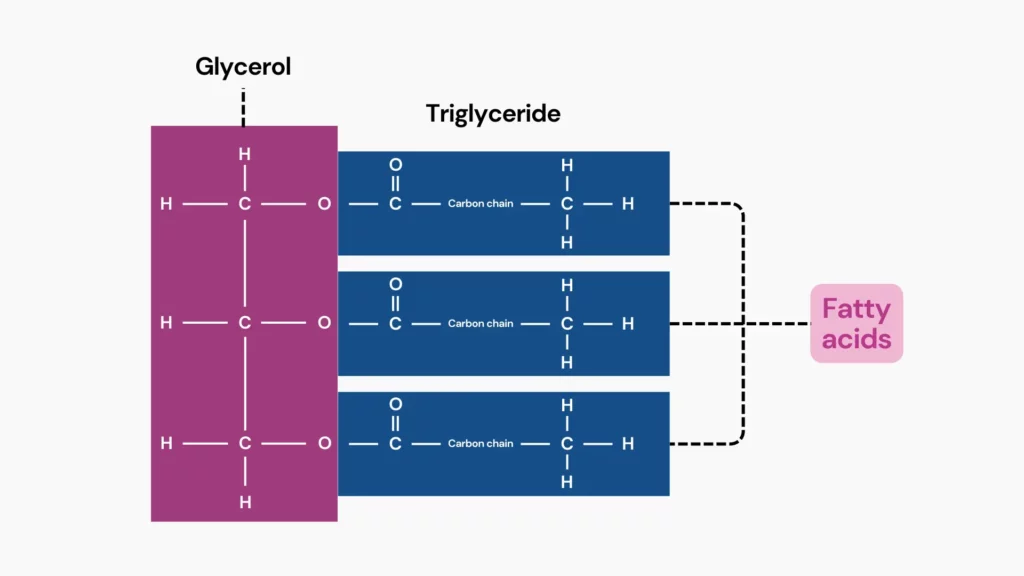
Most dietary fats are long-chain triglycerides (LCTs) with more than 12 carbon atoms. MCTs are medium-chain fatty acids containing 6-12 carbon atoms.
This difference in chain length gives MCT oil unique properties compared to LCTs, found in foods like fish, avocados, nuts, seeds, and olive oil.
Unlike LCTs, MCTs are digested and absorbed quickly in the liver without requiring enzymes or bile acids.
This rapid metabolism sets MCTs apart – they are used immediately for energy or converted into ketones, energy sources derived from fat breakdown.
MCTs are classified into four types based on their carbon chain length:
These attributes make MCT oil a beneficial addition to the diet, especially for those seeking a quick energy source or following a ketogenic diet.
MCT oil is a favorite among those trying to get healthier overall and in terms of nutrition since it provides several health advantages.
MCT oil, which contains fatty acids like caprylic, capric, and lauric acids, may help reduce inflammation by fighting microbes.
Studies show that MCT-rich coconut oil can inhibit the growth of Candida albicans, which causes infections like thrush, and reduce Candida infections in premature babies.
Additionally, virgin coconut oil has been found to slow the growth of Staphylococcus aureus and enhance immune response, potentially helping control inflammation.
However, current evidence is primarily from lab and animal studies, which may not directly apply to humans. More clinical trials are needed to verify these effects in people.
Hand-picked Article For You: How Genes Influence Your Preference of Fatty Foods
Coconut oil, extracted from copra (dried coconut kernel), is a natural leader in medium-chain triglyceride levels. Its fat composition contains an MCT concentration of approximately 54%.
This oil consists of lauric acid (42%), caprylic acid (7%), and capric acid (5%). However, coconut oil also contains long-chain triglycerides and unsaturated fats.
Even though lauric acid is technically considered a medium-chain fat, your body breaks it down and absorbs it more slowly, similar to how it handles LCTs.
This delayed processing has led some experts to argue that, despite its MCTs, the high amount of lauric acid keeps coconut oil from being classified as mainly MCT-rich.
While MCTs contribute significantly to coconut oil's health benefits, their unique composition includes other bioactive compounds that offer further advantages, such as:
The following table highlights the key differences between these two popular oils, focusing on their distinct characteristics and health impacts.
| MCT oil | Coconut oil | |
| Source | Extracted from refined coconut or palm oil to isolate MCTs | Derived from coconut flesh |
| Fatty acid | Primarily contains caprylic acid (50%-80%), and caproic acid (20%-50%) | Contains lauric acid (42%), caprylic acid (7%), and capric acid (5%) |
| Nutritional components | High concentration of MCTs | Natural source of MCTs along with other components |
| Uses | Added to coffee, smoothies, and sometimes used as butter substitute | Used in cooking, baking, and for skin and hair care |
| Benefits | Enhances energy levels Supports weight loss, especially for ketogenic diets | Hydrates skin Slows aging Promotes hair health Boosts metabolism |
| Risks | Weight gain High cholesterol Stomach issues ( cramping and bloating) Diarrhea Fat build-up in the liver Vomiting Bloating | Gastrointestinal discomfort Elevated heart disease or stroke risk |
| Digestive tolerance | Easier to digest and absorb | Requires more digestive effort |
| Allergies & sensitivities | MCT oil (refined) lowers coconut allergy risk, but reactions (like coconut allergy) are still possible. | Coconut allergies are relatively uncommon, but they do exist. Some symptoms are hives, rash, anaphylaxis (rare) |
When it comes to weight reduction, MCT oil might be more effective than coconut oil.
The body digests MCT oil and easily converts it into energy rather than storing it as fat.
This unique property can boost metabolism and energy consumption.
Various studies have indicated that MCT oil boosts feelings of fullness, potentially reducing overall calorie intake.
Coconut oil, on the other hand, includes both medium- and long-chain triglycerides.
Although it contains MCTs, a large component is lauric acid, which digests and absorbs like a long-chain fat.
This makes coconut oil less beneficial for weight reduction than pure MCT oil.
Coconut oil is a common pick for healthy skin due to its high concentration of lauric acid.
Lauric acid has powerful antibacterial qualities that are good for beauty and skin health.
Lauric acid can heal acne in human cells, and coconut oil has been proven to alleviate atopic dermatitis (eczema) symptoms such as redness and irritation.
Its fatty acids are excellent for preserving and moisturizing the skin, effectively treating xerosis, a common condition characterized by dry and itchy skin.
These characteristics also make it beneficial against skin diseases.
Even though MCT oil has its own advantages, it lacks some of the additional compounds present in coconut oil that contribute to skin health benefits.
It serves as an effective carrier oil for essential oils while providing moisturizing properties.
Therefore, coconut oil is typically recommended for topical skin care because of its wider range of benefits.
MCT oil and coconut oil both contain triglycerides, but their composition and metabolic effects differ.
MCT oil, with its higher concentration of MCTs, is less likely to raise triglyceride levels in the blood
Coconut oil, due to its LCT content, may cause a greater increase in triglycerides and take longer to digest.
Hand-picked Article For You: How Genes Influence Saturated Fats and Weight Gain Tendency
MCT oil is a flexible component that works well in various dishes and drinks. Here are some practical ways to use it:
Coconut oil, solid at room temperature unless processed, has a high smoke point, making it perfect for high-heat cooking. Here are some ways to use it:
MCT oil shines for those seeking a quick energy boost, weight management support, and potential benefits for neurological conditions. Its rapid conversion into fuel makes it ideal for ketogenic diets and enhancing cognitive function. However, be mindful of potential digestive side effects.
Coconut oil provides broader advantages, such as reducing stress and enhancing skin and hair health. While it boasts some MCTs for energy, its LCT content makes it less suitable for weight loss than MCT oil.
https://www.medicinenet.com/mct_oil_vs_coconut_oil_whats_the_difference/article.htm
https://www.healthline.com/nutrition/mct-oil-benefits
https://pubmed.ncbi.nlm.nih.gov/25636220
https://pubmed.ncbi.nlm.nih.gov/20367215
https://pubmed.ncbi.nlm.nih.gov/19436137
https://www.jomes.org/journal/view.html?doi=10.7570/jomes22028
https://pubmed.ncbi.nlm.nih.gov/31694759
https://www.sciencedirect.com/science/article/abs/pii/S0031938418300507
https://pubmed.ncbi.nlm.nih.gov/17570262
https://www.nmcd-journal.com/article/S0939-4753(21)00454-3/abstract
https://pubmed.ncbi.nlm.nih.gov/27187452
https://pubmed.ncbi.nlm.nih.gov/17651080
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6604858
https://pubmed.ncbi.nlm.nih.gov/31673647
https://www.healthline.com/nutrition/mct-oil-vs-coconut-oil
https://www.medicalnewstoday.com/articles/282857
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4247320
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5551307
https://onlinelibrary.wiley.com/doi/abs/10.1002/jsfa.8650
https://pubmed.ncbi.nlm.nih.gov/28689741
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5654187
https://www.medicalnewstoday.com/articles/coconut-allergy
https://www.sciencedirect.com/science/article/pii/S0022316622003662
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4892314
The benefits of a warm cup of tea on a slow afternoon go further than just relaxation. Each heavenly sip is actively nourishing your gut and simultaneously boosting your metabolism. Teas have helped to combat digestive problems like nausea, constipation, bloating, and indigestion for millennia. This article will go over five of the best teas for your gut. Read on to know why, how, when, and when not to drink these five teas.
Ginger contains compounds known as gingerols and shogaols, which can stimulate stomach contractions and gut cleansing.
It's beneficial for nausea, bloating, and indigestion.
Ginger tea can also reduce the severity of morning sickness and nausea during pregnancy.
Ginger tea bags are readily available at grocery stores.
Making ginger tea at home with a few pieces of sliced ginger root can strengthen the brew's flavor.
Fennel is an herb rich in antioxidants, a set of molecules that control dangerous free radicals in the body.
As such, they are helpful in combatting gut ulcers and preventing their development.
Additionally, they can stimulate bowel movements.
The gas relief it provides can help manage the effects of Irritable Bowel Syndrome (IBS).
Fennel tea can be made by steeping the seeds or the freshly grated root of the herb in a cup of boiling water.
Black tea is jam-packed with healthy compounds like thearubigins and theaflavins.
These compounds help with indigestion and prevent stomach ulcers while promoting gut cleansing.
The polyphenols in black tea help moderate microbial activity in your gut. They effectively weed out harmful bacteria and promote the growth of beneficial bacteria.
Since black tea molecules are too large to be absorbed, they remain in the intestine and promote liver metabolism remotely, boosting endocrine health.
Black tea bags are widely available, although you could also use black tea leaves from the plant Camellia sinensis.
Peppermint tea is renowned for improving digestion by fighting indigestion and IBS.
One of the main compounds in peppermint tea is menthol, an essential oil with a host of digestive benefits against bloating and gas caused by IBS.
Since peppermint oil helps ease nausea in pregnant females, peppermint tea will likely have a similar effect.
Further research into the effects of peppermint tea on human digestion will yield more information.
Spearmint tea contains beneficial minerals and nutrients, including antioxidants, vitamin C, iron, and folate.
S-carvone is a compound that naturally occurs in spearmint tea at high concentrations.
It has a strong ability to inhibit muscle contractions in the gut, providing relief from digestive upsets.
Spearmint tea also stabilizes the gut during episodes of nausea.
Interestingly, spearmint tea is the drink of choice for people with PCOS since it reduces the body's oxidative stress and inflammation.
When drawing up a tea routine, you should be aware of the benefits of each kind of tea.
For instance, caffeinated teas can give you the energy boost you need to start the day.
Some examples of caffeinated teas include:
Hand-picked Article For You: How Much Caffeine Is Too Much?
Before a meal, a cup of tea can stimulate digestion.
The best teas to stimulate digestion are:
At the end of the day, caffeine-free teas can help you wind down.
These could include:
https://www.hopkinsmedicine.org/health/wellness-and-prevention/ginger-benefits
https://www.healthline.com/nutrition/tea-for-digestion
https://www.webmd.com/diet/health-benefits-fennel-tea
https://www.medicalnewstoday.com/articles/319646
https://www.medicalnewstoday.com/articles/319651
https://www.medicalnewstoday.com/articles/325242
https://www.healthline.com/nutrition/peppermint-tea
https://www.healthline.com/nutrition/spearmint
https://www.webmd.com/diet/spearmint-tea-health-benefits
Less than 2% of the global population carries the red hair gene, one of the most intriguing human traits. It may seem like common knowledge that red hair originated in the Viking lands of Scandinavia. However, research points to red hair originating in Central Asia as a mechanism against the harsh sun. Eventually, it spread to remote regions like Ireland, Scotland, and Scandinavia, where it is most abundant today. This article will help you learn more about the red hair gene: why some people have red hair, how the gene travels down generations, how red hair can affect your skin, and how to know if you could be a carrier of the gene.
Melanin, a coloring pigment produced by the melanocyte cells in the hair, determines hair color.
When melanocytes produce an excess of eumelanin, a dark-colored melanin pigment, people get black or brown hair.
Those who don’t produce enough of this pigment have blond hair.
In rare cases, the melanocytes produce another pigment called pheomelanin.
Pheomelanin is a yellow/reddish pigment responsible for the iconic red-colored hair.
The type of melanin pigment the melanocyte cells produce depends on a person’s genes.
Image: Types of Melanin Pigments
The MC1R gene is one of the strongest influencers of red hair.
Thus, it is also called the red hair gene.
It instructs your body to produce the melanocortin-1 receptor that decides which type of melanin the melanocytes produce.
When the receptor is active, it encourages the melanocytes to produce eumelanin, leading to darker hair color.
When the receptor is blocked or inactive due to mutations in the MC1R gene, it produces pheomelanin instead, leading to reddish hair color.
Pheomelanin production causes individuals to grow red hair.
Red hair is a recessive genetic trait.
This means that a person must inherit the genetic change associated with red-colored hair from both biological parents for it to be active.
Many people may be carriers of one copy of the mutated gene and still have darker hair color.
A study reports that up to 40% of people in Scotland carry at least one copy of the mutated gene despite only 13% having red hair.
In some families, a child could mysteriously be born with red hair despite generations of people having darker hair.
The darker hair implies that the previous generations were all silent carriers of the gene.
Genetic testing could predict an interesting turn of events like this.
Genetic testing can identify if the parents are carriers of the MC1R gene mutations and predict whether a child will have red hair.
The effects of carrying the MC1R gene don’t end with the hair alone.
A few conditions seen in such individuals include:
Genetic testing to know whether you carry the red hair gene is thus beneficial for you and your future generations.
The following scenarios will help you understand your likelihood of having a child with red hair.
Each scenario has a different genetic makeup of the biological parents involved.
Both parents have dark hair.
In this case, there is a practically 0% chance that your child will be red-haired.
Both parents have dark hair and carry one copy of the gene each.
In this case, there is a 25% chance that the child will have red hair and a 50% chance that the child may have dark hair but carry the red gene.
One parent has two copies of the gene, and the other has none.
In this case, the children may carry the red hair gene but will not have red hair.
In this case, there is a 50% chance the child will be red-haired and another 50% chance that the child will be dark-haired and a carrier of the red hair gene.
In this case, all the children will also have red hair.
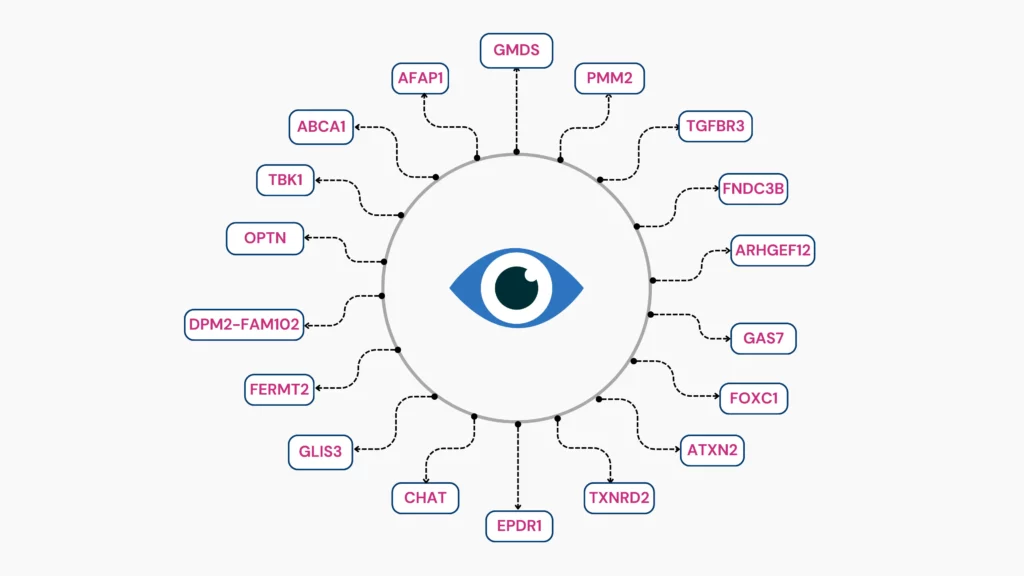
Millions of Americans unwittingly endure glaucoma, an invisible cause of vision problems every year. The early symptoms of glaucoma can be hard to diagnose, so people don’t usually find out until it’s too late. Genetic mutations are one of the leading causes of glaucoma, and regular genetic and eye testing can help diagnose it in time, especially for those with a positive family history of the disease. Read on to learn about glaucoma, its genetic risk factors, its causes, and how to identify if you’re at risk.
Glaucoma is a hereditary condition that damages the optic nerve.
This nerve sends visual signals from the eye to the brain, helping you understand what you see.
Glaucoma progresses slowly. There are no clear early signs of this disease, and most people don’t seek medical attention until they notice a decline in their vision.
People with a genetic risk for the condition may need regular eye exams to monitor their optic nerve health and intraocular pressure (IOP).
High IOP is the main culprit of glaucoma.
A lubricant called aqueous humor circulates within the anterior chamber of the eye. In order to maintain a stable IOP, it is drained out of the eye regularly.
If this drainage system is blocked, the aqueous humor builds up in the eye, increasing the IOP.
Pressure builds on the optic nerve, gradually causing the death of optic nerve fibers, leading to blind spots and poor vision.
Research has shown that some forms of glaucoma are hereditary and can be passed down through generations.
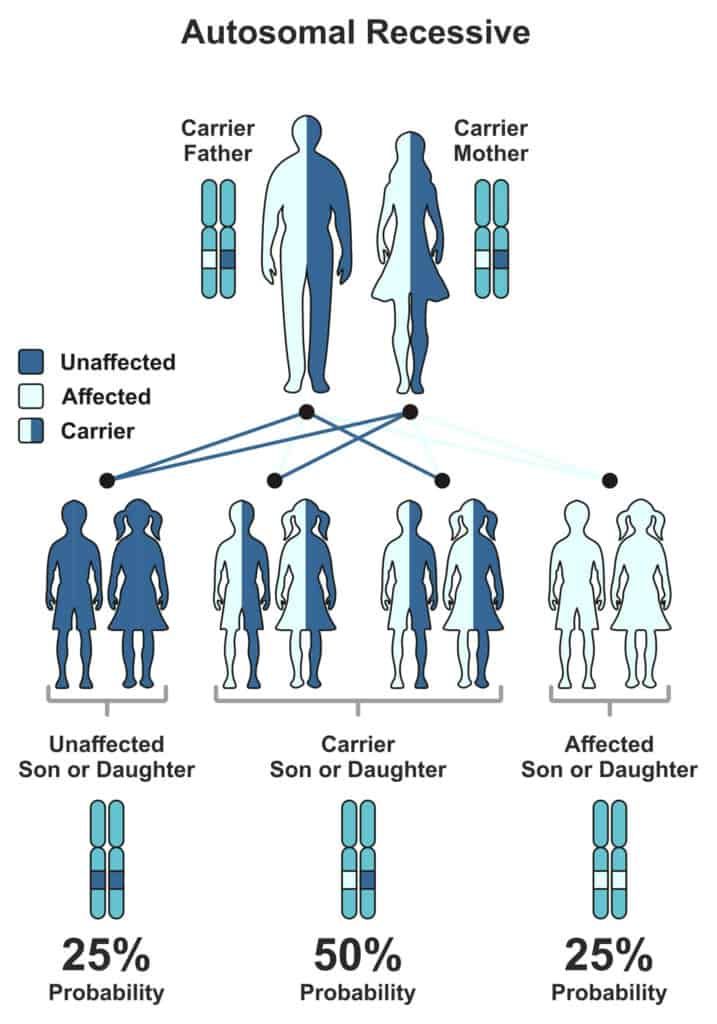
Glaucoma is inherited in either an autosomal dominant or autosomal recessive manner.
In autosomal dominant inheritance, only one copy of the mutated gene from either parent is needed to express itself in both the parent and the offspring. Juvenile glaucoma is inherited in this manner.
In autosomal recessive inheritance, both parents must carry one copy of the mutated gene (in its recessive state), and the child must inherit both copies to be at risk for glaucoma. Congenital glaucoma is inherited in this manner.
Some variants of glaucoma may run in the family. The parents may be carriers of the mutated genes and not develop the condition themselves while passing it on to their children.
Sometimes, existing risk factors like hypertension, hypotension, diabetes, age, or eye injury in families could lead to the development of glaucoma.
A meta-analysis studied 46 published observational research papers to find gender-based risk factors for developing OAG.
The results found that men were 1.4 times more likely to develop glaucoma than women.
The myocilin (MYOC) gene produces the myocilin protein, which is essential for maintaining IOP.
Scientists have identified at least a hundred variations of the MYOC gene.
These variations may lead to the underproduction of myocilin, leading to increased intraocular pressure and glaucoma.
About 4% of all cases of primary OAG and more than 10% of all cases of juvenile OAG are due to MYOC mutations.
The Cytochrome P450 family 1 subfamily B member 1 (CYP1B1) gene produces the CYP1B1 enzyme.
Researchers have studied over 100 variations of this gene.
50% of all cases of primary congenital glaucoma are due to mutations in this gene at the GLC3A locus.
The Latent Transforming Growth Factor Beta Binding Protein 2 (LTBP2) gene produces the LTBP2 protein, which forms the anterior chambers of the eye.
A study found that null mutations in this gene could lead to an increased risk of developing PCG.
While these 3 are the most researched genes for glaucoma, other genes also play a minor role in causing the disease.
Changes in certain genes can increase your risk for many chronic health conditions, including glaucoma. Learn more:
Increased IOP slowly damages the optic nerve over time, leading to open-angle glaucoma (OAG)
Though it doesn’t show early symptoms, it could lead to blurry vision and the gradual loss of both peripheral and central vision.
A 2011 study reports that single-gene mutations cause 5% of all POAG.
For instance, mutations in the MYOC gene can cause juvenile open-angle glaucoma.
Multiple mutations and environmental risk factors can lead to the other 95% of cases.
Early-onset glaucoma is a type diagnosed before the age of 40 in adults.
This type is primarily hereditary and may occur even without related risk factors.
A majority of early-onset glaucoma cases turn out to be primary open-angle glaucoma.
Early-onset glaucoma is generally inherited in an autosomal recessive manner- meaning that while parents may carry one copy of the gene, the disease will not be inherited unless the child carries both copies.
Congenital glaucoma occurs in infants before the age of three, leading to optic nerve damage and vision loss.
Infants with congenital glaucoma generally exhibit red or cloudy eyes, an increased rate of blinking, light sensitivity, and tear production without crying.
Congenital glaucoma could be due to complications affecting the infant’s eye as a fetus.
Studies say that variations in the CYP1B1 or LTBP2 genes could lead to the development of primary congenital glaucoma in infants under the age of three.
Juvenile OAG (JOAG), diagnosed in childhood or early adulthood, is called juvenile open-angle glaucoma.
The cause and prognosis of the disease are the same.
Juvenile OAG is inherited in an autosomal dominant manner, meaning that if even one parent carries a MYOC gene with the specific mutation responsible for JOAG, the child will end up with JOAG.
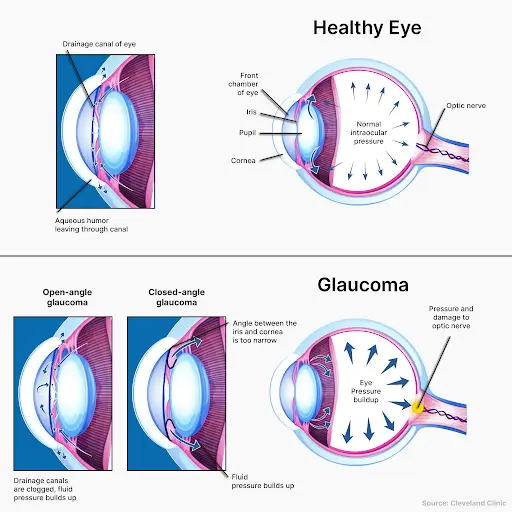
Angle-closure glaucoma (ACG) occurs when the IOP suddenly increases, stopping the movement of the aqueous humor in the eye.
Since this is an acute attack, it presents with headaches, nausea, and eye pain. The vision turns blurry, and halos are visible around light sources.
ACG generally presents in one eye at a time. With timely medical aid, doctors could save the other eye.
Interestingly, normal-tension glaucoma damages the optic nerve without an increase in IOP.
Instead, normal-tension glaucoma could develop due to poor blood flow to the optic nerves or some other inherited trait.
Secondary glaucoma is the development of either open-angle or angle-closure glaucoma due to a separate condition, such as:
Analyzing your genes can also help you understand your risk of developing the disease.
Genetic testing is beneficial in identifying early-onset glaucoma if the condition begins manifesting itself in people under 40 years of age.
Suppose genetic testing reveals a higher risk of developing glaucoma. In that case, you may need regular eye exams done by an eye doctor to diagnose the condition before it worsens.
In fact, a comprehensive eye exam once every two years can be beneficial to anyone whose first-degree relatives are diagnosed with glaucoma.
Water helps lower IOP if consumed in moderation. Drinking too much water in a short time can lead to increased IOP.
Glaucoma is not a fatal condition. It will neither increase your mortality risk nor lead to fatal complications.
Stress does not directly lead to open-angle glaucoma. However, patients who are regularly overwhelmed may neglect their treatment courses, which could worsen their condition.