Is Epilepsy Hereditary? It is estimated that 1 in 26 people will develop epilepsy in their lifetime. While the cause of epilepsy is unknown in the majority of cases, researchers have identified certain genes that may be associated with the disorder. In this article, we will discuss what is known about the genetics of epilepsy and whether there is a single “epilepsy gene.”
Researchers have identified several genes associated with epilepsy.
In the sample report below, we've attempted to analyze some important genes that increase the risk of epilepsy.
You can identify your genetic risk of epilepsy by using your 23andMe DNA data and placing an order for the Gene Health Report.
Epilepsy is a chronic neurological disorder that affects people of all ages.
It is characterized by recurrent seizures ranging from brief and nearly undetectable to long and debilitating.
Epilepsy can be caused by many factors, including head injuries, genetic predisposition, and infections.
There is no cure for epilepsy, but certain medications and treatments can help manage it effectively.
Epilepsy is genetic if the seizures occur due to a genetic defect.
However, not all cases of genetic epilepsy are inherited.
Some genetic defects can occur spontaneously in people even if they are not present in either biological parent.
Most cases of idiopathic (cause unknown) epilepsy are due to abnormal changes in several genes.
Each of these genes contributes to a small percentage of epilepsy risk; when someone inherits a combination of these genes, they can be at high risk for epilepsy.
Genetic variants underlie about 30-40% of epilepsy cases.
However, analyzing a person’s chance of inheriting epilepsy is complicated.
For instance, two siblings with epilepsy may have inherited mutations in different genes.
On the other hand, two family members with the same genetic mutation for epilepsy may manifest symptoms in different ways.
Furthermore, inheritance pattern varies depending on the type of epilepsy - like focal, idiopathic, or generalized epilepsy.
What are the chances of your inheriting epilepsy?
With the advancements in genetic technologies, research studies are discovering more and more genes associated with epilepsy.
According to a study based on search results from the OMIM database, 84 genes were classified as epilepsy genes.
Some are directly associated with epilepsy, some are associated with conditions whose core symptom is epilepsy, and some are associated with epilepsy and multiple other phenotypes.
| Phenotype (in order of the onset age) | Gene |
| Neonatal | |
| Pyridoxamine 5'-phosphate oxidase deficiency (PNPOD) | PNPO |
| Pyridoxine-dependent epilepsy (EPD) | ALDH7A1 |
| Benign familial neonatal seizures (BFNS) | KCNQ2, KCNQ3 |
| Infantile and childhood | |
| Familial infantile myoclonic epilepsy (FIME) | TBC1D24 |
| Benign familial infantile seizures (BFIS) | PRRT2, SCN2A, SCN8A |
| Amish infantile epilepsy syndrome (AIES) | ST3GAL5 |
| Early infantile epileptic encephalopathy (EIEE) | CACNA1A, GABRA1, GABRB3, KCNQ2, KCNT1, SCN2A, SCN8A |
| AARS, ARV1, DOCK7, FRRS1L, GUF1, ITPA, NECAP1, PLCB1, SLC12A5, SLC13A5, SLC25A12, SLC25A22, ST3GAL3, SZT2, TBC1D24, WWOX | |
| CDKL5 | |
| ARHGEF9 | |
| ALG13, PCDH19 | |
| DNM1, EEF1A2, FGF12, GABRB1, GNAO1, GRIN2B, GRIN2D, HCN1, KCNA2, KCNB1, SIK1, SLC1A2, SPTAN1, STXBP1, UBA5 | |
| Dravet syndrome (DS) | SCN1A, SCN9A |
| Familial febrile seizures (FFS) | GABRG2, GPR98, SCN1A, SCN9A |
| CPA6 | |
| Generalized epilepsy with febrile seizures plus (GEFS + ) | GABRD, GABRG2, SCN1A, SCN1B, SCN9A, STX1B |
| Generalized epilepsy and paroxysmal dyskinesia (GEPD) | KCNMA1 |
| Myoclonic-atonic epilepsy (MAE) | SLC6A1 |
| Childhood-onset epileptic encephalopathy (COEE) | CHD2 |
| Focal epilepsy and speech disorder (FESD) with or without mental retardation | GRIN2A |
| Childhood absence epilepsy (CAE) | GABRG2 |
| CACNA1H, GABRA1, GABRB3 | |
| Juvenile and later | |
| Juvenile absence epilepsy (JAE) | CLCN2, EFHC1 |
| Juvenile myoclonic epilepsy (JME) | CACNB4, CLCN2, EFHC1, GABRD |
| GABRA1 | |
| Idiopathic generalized epilepsy (IGE) | CACNB4, CLCN2, GABRD, SLC12A5, SLC2A1 |
| CACNA1H, CASR | |
| Familial adult myoclonic epilepsy (FAME) | ADRA2B |
| CNTN2 | |
| Familial temporal lobe epilepsy (FTLE) | CPA6, GAL, LGI1 |
| Not specific | |
| Progressive myoclonic epilepsy (PME) | KCNC1 |
| CERS1, CSTB, EPM2A, GOSR2, KCTD7, LMNB2, NHLRC1, PRDM8, PRICKLE1, SCARB2 | |
| Nocturnal frontal lobe epilepsy (NFLE) | CHRNA2, CHRNA4, KCNT1 |
| CHRNB2 | |
| Familial focal epilepsy with variable foci (FFEVF) | DEPDC5 |
Epilepsy trigger is not the same as epilepsy cause.
Triggers are discussed in a person who already has epilepsy.
Triggers result in seizures in a person with epilepsy.
Some common triggers are:
Used to identify any changes in the number of chromosomes and large deletions, duplications, and inversions of the genetic material.
A very common choice for epilepsy genetic tests.
Around 10% of people with epilepsy have abnormal CMA results.
Used to visualize missing or extra pieces of genetic material.
Uses next-generation sequencing (NGS) technologies to visualize multiple genes associated with epilepsy simultaneously.
Analyzes all the portions of the DNA that make protein.
Can explain the genetic cause of 30% of epilepsy cases.
Analyze the entire DNA content (the genome) of an individual.
Currently employed majorly for research purposes and not so much in clinical settings.
Analyzes genetic changes called single nucleotide polymorphisms associated with epilepsy.
Not used for diagnosis; provide a genetic risk landscape for epilepsy.
Epilepsy is a neurological condition characterized by recurrent seizures.
Most idiopathic epilepsy cases have a genetic background do it.
Epilepsy in biological parents increases the risk of their children developing it; the risk increases when the biological mother is affected.
Most genes implicated in epilepsy play a role in regulating the entry of ions like sodium and calcium into the cell.
Some diagnostic genetic tests for epilepsy include karyotyping, chromosomal microarray, and whole-exome and whole-genome sequencing.
Genotyping analyzes small changes in genes (called single nucleotide polymorphisms) to provide a genetic risk landscape for epilepsy.
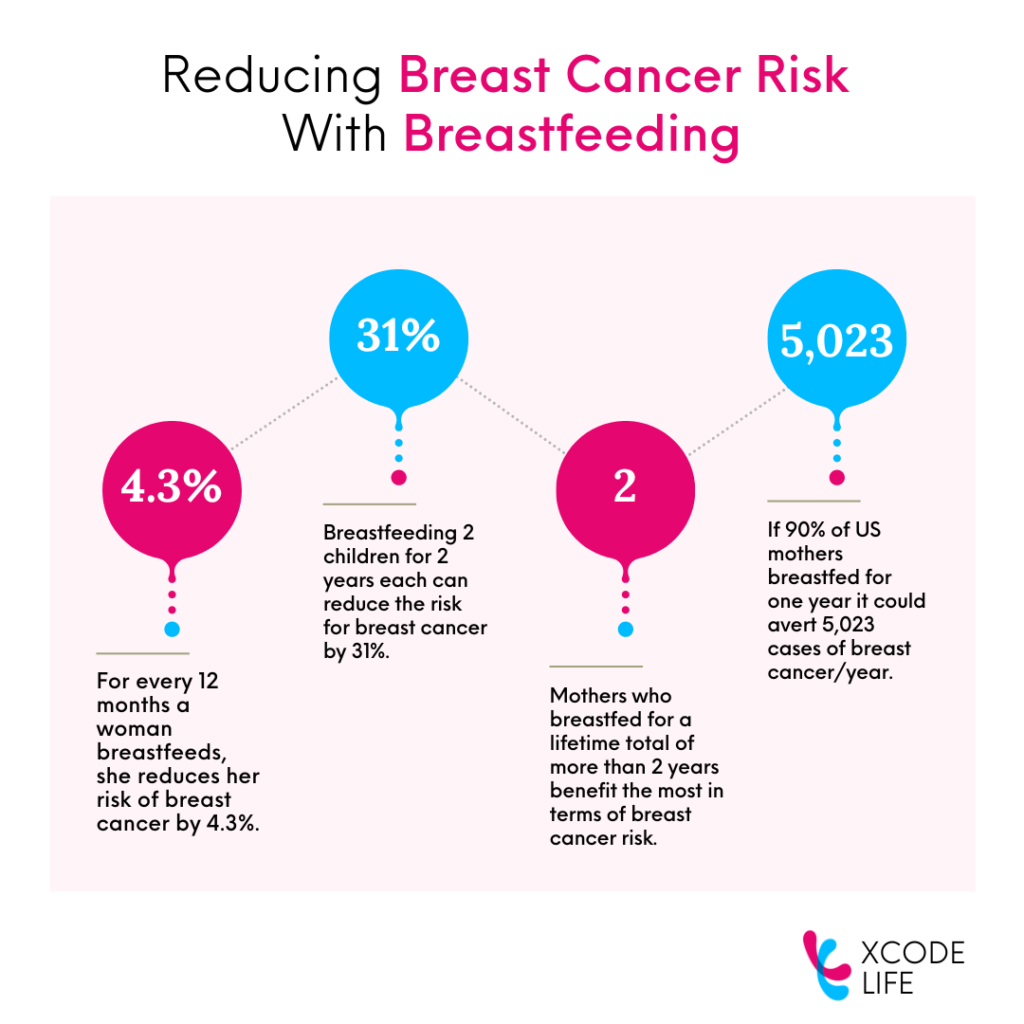
It is widely known that breastfeeding has many benefits for both mother and child. However, one potential benefit that is not as well known is that breastfeeding may also reduce a woman’s risk of developing breast cancer later in life. In fact, according to a 2018 study, “breastfeeding for 12 months or longer can lower a woman’s risk of breast cancer by up to 28% compared to women who never breastfed.
According to the American Academy of Pediatrics (AAP), exclusive breastfeeding of infants for about the first six months and continued breastfeeding for a year or longer after introducing solid foods is recommended.
The World Health Organization(WHO) also recommends exclusive breastfeeding for the first six months of an infant’s life.
Exclusive breastfeeding refers to giving infants only breast milk and no other solid or liquid foods.
According to the Centre for Disease Control and Prevention(CDC), only one in four infants are exclusively breastfed for the first six months.
Breastfeeding is beneficial for both the infant and the mother. Benefits of breastfeeding include:
Research shows that breastfeeding mothers have a lower risk of developing pre and postmenopausal breast cancer.
This benefit increases with an increase in the duration of breastfeeding for more than 6 months.
Researchers have put forth several possible explanations to address the link between breastfeeding duration and breast cancer risk.
All these explanations revolve around exposure to one of the female sex hormones, estrogen.
Estrogen stimulates breast cell growth.
Prolonged exposure to estrogen can increase the risk of breast cancer.
Women have lower levels of estrogen during breastfeeding periods.
This is because breastfeeding delays menstrual periods.
The lifetime exposure to estrogen decreases with longer breastfeeding durations, decreasing the risk of breast cancer.
Another reason is that the breast sheds a lot of tissue after lactation.
During this process, it may also eliminate cells with damaged DNA that may lead to cancerous growth.
Lactation may also lead to changes in gene expression in breast cells.
This can decrease the risk of cancer development.
A meta-analysis study showed that breastfeeding contributed to a 20% reduced risk for triple-negative breast cancer and a 10% reduced risk for estrogen receptor-negative breast cancer.
Studies have estimated that the heritability of breastfeeding duration ranges from 44 to 54%. People with certain genetic types may tend to breastfeed their children for a longer duration than others.
The XRCC2 gene contains instructions for producing a DNA repair protein.
This protein also helps maintain chromosomal stability.
Changes in this gene are associated with an increased risk of breast cancer and Fanconi anemia.
Fanconi anemia is a rare but serious blood disorder that prevents your bone marrow from making enough new blood cells for your body.
It is passed down through families.
rs3218536
rs3218536 is a single nucleotide polymorphism or SNP in the DNA-repair gene XRCC2.
A 2010 study examined the role of DNA repair deficiencies in cancer development, especially in breast cancer.
The study population was divided into women who breastfed and women who had never breastfed.
It was observed that among women who had never breastfed, those who carried the AG genotype of rs3218536 had a lower risk of breast cancer than those with the other genotypes.
After classifying this group according to their menopausal status, it was observed that postmenopausal women with the A allele had a lower risk of breast cancer than those with the G allele.
The MDM2 gene contains instructions for producing Mouse double minute 2 homolog (MDM2) protein. It is also known as E3 ubiquitin-protein ligase Mdm2 protein.
This protein acts as a negative regulator (suppresses the activity) of the p53 tumor suppressor protein.
A study has reported that the activity of the MDM2 gene seems to be amplified in breast cancer cells.
rs2279744
rs2279744, also known as 410T-G, has been studied for several years to determine its role in cancer.
This SNP influences the ability of the MDM2 protein to bind to the p53 tumor suppressor protein.
The G allele of this SNP is associated with an increased risk for breast cancer, especially in women who have breastfed for less than 6 months and women who are obese.
Some factors that influence breastfeeding duration include:
Is cleft lip genetic? A cleft lip is a congenital disability where the upper lip and nose do not form properly. It is one of the most common congenital disabilities in the world. Cleft lip is usually due to a combination of genetic and prenatal factors. Most people with cleft lip have no family history of the condition. However, certain genes may increase the risk of cleft lip.
Source: Cleft Collective Study
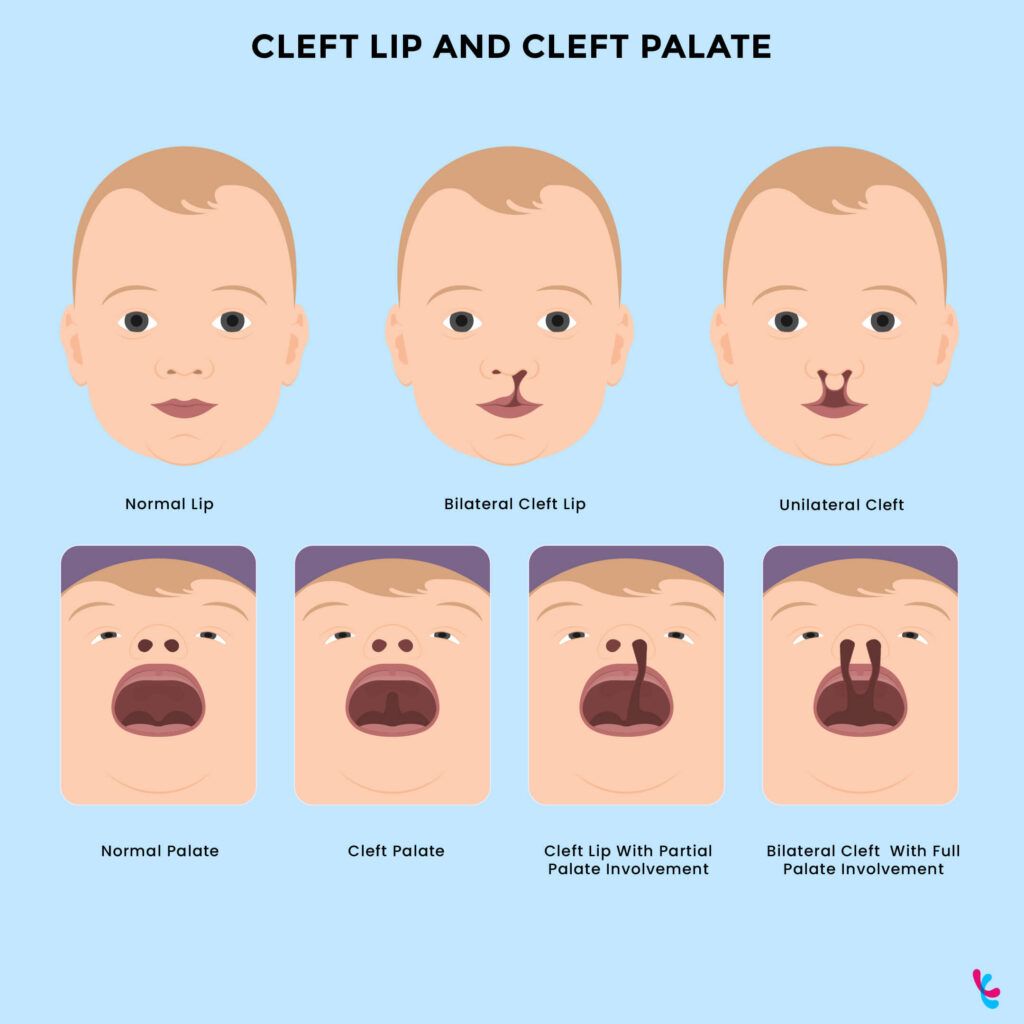
Cleft lip and cleft palate (CLCP) are common congenital disabilities that occur when the baby’s lip and mouth parts do not develop well during pregnancy.
Together, these defects are called orofacial (relating to mouth and face) defects.
They can be isolated or associated with other inherited conditions and genetic syndromes.
In cleft palate, the two halves of the roof of the mouth don’t join completely.
With cleft lip, the tissue forming the lip does not join completely before birth.
This can occur on one side of the face (unilateral CLCP) or both sides (bilateral CLCP).
The cause of CLCP is unknown.
Research suggests that certain genetic factors and prenatal environment play a role.
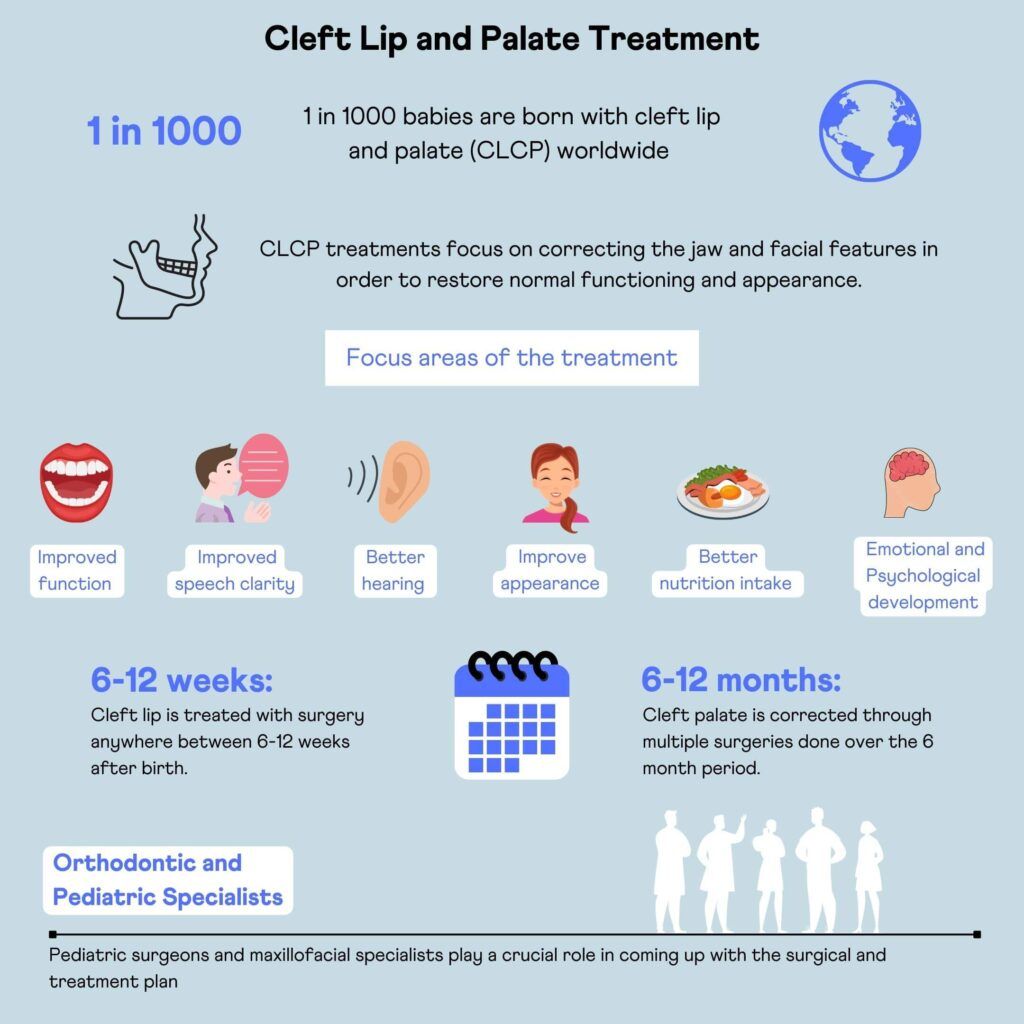
The most common treatment option for CLCP is surgery.
Those treated for cleft lip or palate typically have normal lives.
Around the end of the first month or beginning of the second month of pregnancy, the baby’s mouth develops as two halves which grow closer together and fuses by the 6th or 8th week of pregnancy.
This fused part moves forward and backward to form the lips and uvula, forming the full mouth by the 10th week of pregnancy.
With cleft palate or cleft lip (or both), the two halves of the palate do not fuse.
Around 1 in 1000 babies are born with CLCP worldwide.
In the United States, 1 in 1600 babies are born with CLCP, 1 in 2800 babies are born with cleft lip, and 1 in 1700 babies are born with cleft palate.
There’s no single “cleft lip gene.”
However, research points to combinations of different genes as a risk factor for cleft lip.
According to a study, the risk for cleft lip in first-degree relatives with a family history of this condition is 32 times higher than those without.
To date, 13 genome-wide linkage scans have been performed for CLCP.
They have identified several candidate genes for cleft lip, some of which are:
A 2014 study reviewed the plausible biological role of a few of these genes in cleft lip and cleft palate.
Determining the inheritance of cleft lip is tricky, as it is associated with several conditions.
If a parent has cleft, the child has a 2-8% chance of inheriting it (if cleft lip is seen as a condition by itself).
If the parent’s parents or siblings also have cleft lip, the inheritance chances raise to 10-20%
However, if it’s associated with other genetic conditions, the inheritance can be as high as 50%.
A family history of cleft lip, with the parents unaffected, gives rise to an inheritance rate of <1%.
With no family history at all, the likelihood of having a child with cleft is 0.14%.
When a child with cleft lip is born to unaffected parents, their chances of having another child with cleft lip is 2-8%.
The prevalence of CLCP is the highest in those of Asian or Amerindian descent (1/500) and least in those of African descent(1/2500).
Caucasian populations have an intermediate prevalence rate (1/1000).
According to the CDC, those who smoke during pregnancy are at an increased risk of having a baby with an orofacial cleft than those who don’t smoke.
Studies hypothesize an association between clefting and errors in the alcohol-metabolizing gene ADH1C.
A study reported that errors in alcohol metabolism combined with heavy maternal alcohol consumption increase the risk for orofacial clefts.
Some evidence supports that women with diabetes before pregnancy are at increased risk of having a baby with cleft lip.
Medications that treat seizures (like topiramate or valproic acid) taken during pregnancy (first trimester) can increase cleft lip risk in the baby.
Ultrasound can pick up cleft lip anywhere between 18-21 weeks of pregnancy.
However, it can be difficult to diagnose some cases of clefting through routine ultrasounds.
In this case, it can be diagnosed immediately after birth or within 72 hours.
Surgery is the most common treatment option for cleft lip.
It is done within the first 12 months of life.
Surgical repair not only improves the appearance but also breathing, hearing, and speech clarity.
Speech and language therapy can help manage speech clarity problems.
Orthodontist support may be helpful in looking after the child’s dental health.
Children treated for cleft lip tend to have normal lives.
If the cleft lip is a manifestation of another genetic condition, their outlook will depend on the nature of the underlying condition.
Surgery for cleft correction doesn’t have major side effects except for a small scar that fades over time.
A cleft lip is a congenital disability resulting in improper lip or mouth palette closure.
Cleft lip develops during the 10th week of pregnancy and is a condition by itself or associated with other genetic conditions.
Cleft lip in parents, siblings, or second and third-degree relatives can increase the risk of a child being born with this condition.
Genes implicated in cleft lip play a role in the development of craniofacial features.
Routine ultrasound typically picks up cleft lip, and this condition can be treated within a year of birth.
Once treated, it is possible to live a full and normal life.
https://pubmed.ncbi.nlm.nih.gov/18250102/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3925974/
https://www.nhs.uk/conditions/cleft-lip-and-palate/
https://www.news-medical.net/health/Causes-of-cleft-lip-and-palate.aspx
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3925974/#R25
In the past, if a woman wanted to know her risk for developing breast cancer, she would simply look at her family history. However, thanks to advances in genetic testing, women can now get a more accurate assessment of their risk by testing for the BRCA genes. While this test is not foolproof, it can give women a better idea of their chances of developing breast cancer and help them make more informed decisions about their health.
Getting a BRCA genetic report for breast cancer can help you in numerous ways.
Some of them include:
The benefits of genetic testing are that it can be used for unique screening protocols, which will aid in the early detection of breast cancer or help identify breast cancer risk.
It is important to note that only 5 to 10% of breast cancer incidences are due to inherited mutations.
According to The National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology (NCCN Guidelines) for Genetic/Familial High-Risk Assessment (version 2017): Breast and Ovarian cancer were developed with the intent to
You should consider genetic testing if you meet any of the following criteria.
Genetic surveillance of women, with the accent on the ethnic background, age, family history and in another appropriate clinical context, will help in stratifying women into high-risk groups so that there is increased surveillance, an extension of chemoprevention or the utilization of risk reduction surgery.
You can now find out if you carry the variants that increase breast cancer risk from Xcode’s Breast Cancer report by uploading your 23andme or any other ancestry DNA raw data.
You can read more about the Xcode Breast Cancer report here.
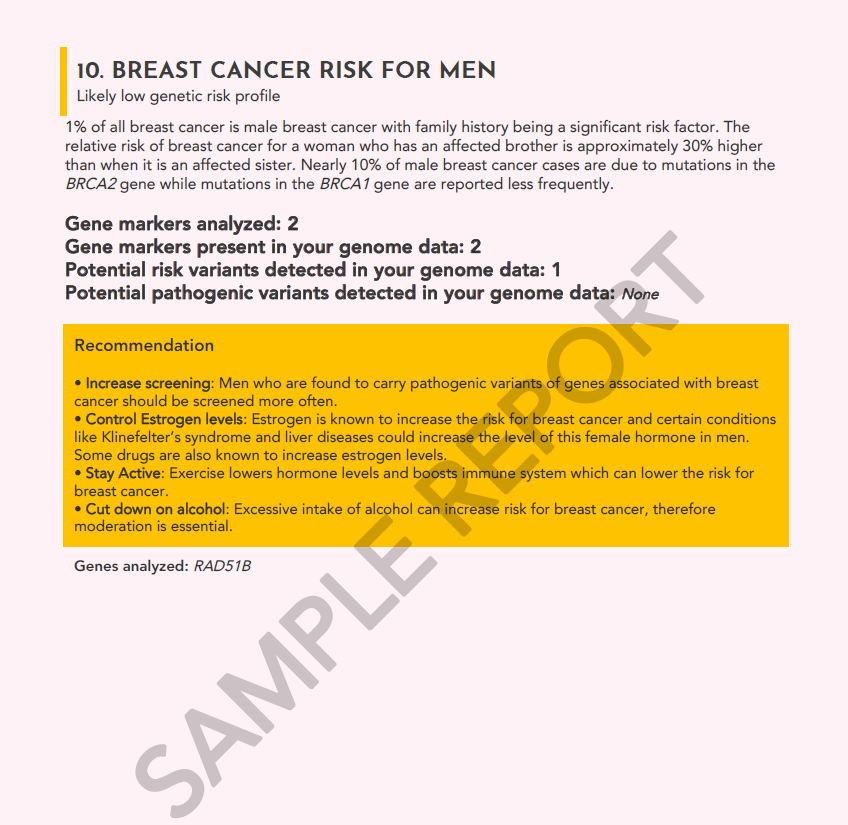
Can men get breast cancer? Breast cancer is not just a woman's disease. It can also affect men. In fact, male breast cancer makes up about 1% of all breast cancers diagnosed each year. Although the number of cases is small, it's important for men to be aware of the signs and symptoms of breast cancer so they can seek treatment early. With early detection, the chances of survival are much higher.
Breast cancer in men is a rare condition.
<1% of all breast cancer cases occur in men.
According to the Centre for Disease Control, 1 in every 100 breast cancer cases in the United States occurs in men.
Early diagnosis can lead to a better outcome for the disease.
There is a lack of awareness about breast cancer in men, which leads to late diagnosis.
Around 40% of breast cancer cases in men are diagnosed in the third or fourth stage.
This condition affects men and women differently.
Men have a lesser and smaller amount of breast tissue compared to women.
The cancerous lumps are smaller, but there is a higher chance of cancer spreading to other tissues in the body.
Common symptoms include
A family history of breast cancer increases the risk of developing breast cancer in men.
About 1 in 5 breast cancer cases in men is hereditary.
The relative risk of breast cancer for a woman who has an affected brother is approximately 30% higher than for a woman with an affected sister.
Abnormal changes or mutations in certain genes result in an increased risk of breast cancer. BRCA1, BRCA2, CHEK2, PTEN, and PALB2 are few genes associated with breast cancer risk in men.
Men with a mutation in the BRCA2 gene have a 7 in 100 chance of developing breast cancer.
Men with a mutation in the BRCA1 gene have a 1 in 100 chance of developing breast cancer.
Other than genetics, factors that influence breast cancer risk include:
The risk of breast cancer increases with age. According to the CDC, the average age of men diagnosed with breast cancer is 65 years.
Elevated levels of estrogen, one of the two main female sex hormones, contribute to the development of breast cancer.
Certain conditions or treatments can lead to an increase in estrogen levels. These include:
Being overweight or obese and engaging in low levels of physical activity contribute to the risk of breast cancer. Heavy drinking may also increase breast cancer risk.
Men who have undergone radiation treatment to the chest area may be at higher risk of developing breast cancer.
Injury or swelling in the testicles, an undescended testicle, or surgery can increase the risk of breast cancer.
Early detection of breast cancer favors early treatment and a better outlook.
This helps prevent the spread of breast cancer to other tissues in the body.
Men with a family history of this condition should undergo regular screening.
Those at a higher risk of developing breast cancer can opt for genetic testing to see if they carry pathogenic variants.
A healthcare provider and a genetic counselor can help you understand risk assessment and the implications of the test.
They can tell you about the pros and cons of the test, your testing options, and further interpret the results and their significance.
There are several health conditions like hypogonadism that can increase estrogen levels.
Even certain antibiotics can increase estrogen levels.
It is important to consult your doctor for advice regarding lowering your estrogen levels in these cases.
Staying active, eating healthy, quitting smoking, and cutting down on alcohol can help keep your hormones in check and lower the risk of breast cancer.
Treatment options include chemotherapy, radiation, hormone therapy, targeted therapy, and surgery.
Based on the diagnosis, the doctor will prescribe the necessary treatment.
When it comes to treating breast cancer, hormone therapy is one option that doctors may prescribe. This treatment works by either stopping the production of hormones or blocking the effects of hormones on cancer cells. While hormone therapy can effectively treat breast cancer, there are also some potential risks and side effects associated with this type of treatment. In this article, we will look at some of the pros and cons of hormone therapy for breast cancer.
Hormone therapy for cancers works by blocking the hormones from attaching to their receptors on the cancer cells and preventing their growth.
It also decreases the production of specific hormones in the body.
Hormone therapy for breast cancer is effective only if it has receptors for estrogen or progesterone.
They are called ER-positive and PR-positive breast cancer, respectively.
These types of breast cancers rely on hormones for their growth.
Thus, lowering the production or preventing the attachment of hormones can help treat cancer.
Hormone therapy can be done before surgery to shrink the tumor for easy removal.
It can also be done after surgery to reduce the chances of recurrence.
Hormone therapy is available via pills, injections or surgery that removes hormone-producing organs, namely the ovaries in women and the testicles in men.
Aromatase inhibitors block the aromatase enzyme activity.
This enzyme helps produce estrogen in the body.
Aromatase inhibitor medications are typically given to postmenopausal women.
Premenopausal women have too much estrogen for aromatase inhibitors to be effective.
In this case, aromatase inhibitors may be used in combination with another drug that can suppress ovarian function.
Examples of aromatase inhibitors approved by the FDA are anastrozole (Arimidex) and letrozole (Femara), both of which temporarily inactivate aromatase, and exemestane (Aromasin), which permanently inactivates aromatase.
Before menopause, ovaries produce the majority of estrogen.
Breast cancer in these women can be treated by suppressing (or eliminating, if required) the ovarian function.
Surgery (removal of ovaries - oophorectomy) and radiation therapy are two options for this.
They both are permanent treatment options.
Ovarian function can also be temporarily suppressed with gonadotropin-releasing hormone (GnRH) agonists, also known as luteinizing hormone-releasing hormone (LHRH) agonists.
These medicines block and interfere with the signals that instruct the ovaries to produce estrogen.
ER+ breast cancers depend on estrogen’s attachment to cancer cells for growth.
Several drugs interfere with estrogen binding to stop or slow breast cancer growth.
Some of them are
Pros
Cons
Pros
Cons
Pros
Cons
Breast cancer treatment depends on a lot of factors like the stage of cancer, the type, how fast the tumor is growing, the tumor’s recurrence rate, and the age, health, and menopausal stage of the woman.
Other than hormone therapy, a few options for breast cancer treatment are:
Hormone therapy works by lowering the levels or blocking the effects of hormones that help cancer cells thrive.
In breast cancer, hormone therapies can block estrogen production or prevent it from binding to the cancer cells.
Common side effects of hormone therapy include hot flashes, changes to the menstrual cycle, mood swings, night sweats, and lowered sexual drive.
Rarely, bone loss, blood clots, heart failure, and cataracts may occur.
Other treatment options for breast cancer include chemotherapy, radiation, immune therapy, and surgery.