Have you ever wondered how your body knows when to wake up, when you're hungry, or how it reacts to stress? Well, that’s all thanks to a little teamwork between your genes and hormones. Let's dive into how these two key players interact to keep your body ticking—and how they can shape everything from your mood to your long-term health.
Hormones are like the body's text messages—sent out from different organs to relay important instructions.
For instance, when you’re stressed, the brain sends a signal to release a hormone called cortisol.
Think of cortisol as your body's natural “stress responder.”
It helps you manage a tough situation, whether you're preparing for a big presentation or just stuck in traffic.
But hormones don’t act alone—they’re influenced by your genes, the unique code that makes you, well, you.
Some genes are like the architects behind hormones. They help build them, decide how they’re used, and even determine how quickly they break down.
Why do some people seem to handle stress better than others? Part of the answer lies in their genes.
Take the CRH gene, for example. It produces corticotrophin-releasing hormone, the first step in the cascade that forms cortisol.
Depending on how your version of this gene works, your body might produce more or less cortisol in response to stress.
It's like having a thermostat that’s a little too sensitive—some people's cortisol levels spike at the slightest hint of stress, while others stay cool under pressure.
So, if you tend to feel frazzled often, your genes might be partly to blame!
Just as genes help regulate hormones, hormones can flip the switch on certain genes.
Imagine hormones as tiny light switches—they can turn genes on or off depending on what’s happening in your body.
For instance, during puberty, hormones like testosterone and estrogen surge, activating genes responsible for growth and development.
That’s why you get that sudden growth spurt or might have felt more emotional during your teenage years.
And here’s where it gets fascinating: These hormone-driven gene changes don’t just affect your appearance—they can influence your behavior, too.
So, if you felt more rebellious or moody as a teenager, you can thank your hormones for pulling the strings behind the scenes.
This gene-hormone interaction isn’t just something that happens during puberty. It continues throughout your life.
For example, genes and hormones work together in adulthood to control your metabolism, immune system, and even your risk for certain diseases.
Here’s a fun fact: If you were born underweight, your genes might respond by making your hormones work overtime to help you "catch up" in growth.
Research has shown that children who experience rapid growth after being born with a low birth weight tend to have higher levels of certain hormones, like IGF-1, which helps regulate growth.
These hormonal shifts can increase the risk of conditions like diabetes later in life.
Let’s look at some important health aspects overseen by the gene-hormone interaction.
Think of the tallest person you know. It’s fun to joke about them walking into door frames, but behind the scenes, the growth hormone is responsible for their height.
It’s secreted from the pituitary gland in our brain and regulates our growth and metabolism.
This is also a perfect example of the gene-hormone interplay at work.
If you have a version of the gene that causes normal growth hormone production, you may end up with an average height.
However, if the gene version causes high growth hormone production, you grow very tall.
During puberty, hormones like testosterone and estrogen flood your body, triggering the genes responsible for growth and development.
They also play a role in fertility.
Testosterone is the male sex hormone.
The SRY gene helps regulate testosterone production.
If it malfunctions, fertility is affected, leading to a host of reproductive disorders.
Conversely, testosterone can activate or deactivate the genes that control how much sperm is produced at a time.
Why do some people seem to eat anything they want and never gain weight, while others gain pounds just by looking at dessert?
Part of the answer lies in the interaction between your genes and hormones.
Your metabolism—the process your body uses to convert food into energy—is regulated by hormones like thyroid hormones and insulin, which are influenced by your genes.
Some people inherit genes that make their hormones super-efficient at burning calories, while others may have slower metabolic rates.
In addition to this, hormones like ghrelin and leptin regulate hunger and satiety, respectively.
The ideal combination would be gene variations that result in lower ghrelin and higher leptin so that you don’t get hungry very often but easily get full upon eating!
This is why weight management can feel like a breeze for some and a battle for others.
Lately, stress has become an unavoidable part of our lives, but it isn’t the real enemy.
The stress response is also called the fight-or-flight response, an important process that helps us navigate through various situations in life.
The stress hormone, called cortisol, prepares your body for this.
Certain genes influence how much cortisol you produce and how quickly it’s cleared from your system.
For some, cortisol levels spike and remain high longer, which can lead to feeling frazzled or anxious.
For others, the stress response is more like a short-lived blip on the radar.
This gene-hormone connection helps explain why some people are calm under pressure, while others may struggle with stress management.
Have you ever had those days when you just can’t shake off a bad mood?
Your hormones could be playing a major part, and your genes may be directing them.
Hormones like serotonin and dopamine, known as the “feel-good” hormones, are partly regulated by your genes.
Some people are genetically more likely to have higher or lower levels of serotonin, which can influence their mental health.
For instance, individuals with certain genetic variants may be more prone to anxiety or depression, as their genes may not allow them to produce or process serotonin effectively.
Now that we know how genes and hormones interact, what can you do to ensure this relationship stays balanced and supports your overall health?
Here are a few practical tips:
Chronic stress can throw your hormone levels out of whack.
Engage in stress-reducing activities like yoga, meditation, or daily walks.
These simple practices can help regulate your cortisol levels, allowing your genes to work in a more balanced environment.
A nutrient-rich diet supports healthy hormone function.
Omega-3 fatty acids (found in fish and flaxseeds) can improve hormonal balance.
Foods rich in antioxidants(like berries) help reduce oxidative stress.
This allows your genes and hormones to work efficiently.
Exercise boosts mood by increasing serotonin and dopamine and helps regulate hormones like insulin and cortisol.
Aim for a mix of cardiovascular workouts, strength training, and flexibility exercises to keep hormones in check and support healthy gene function.
Quality sleep is essential for the optimal function of hormones like melatonin and growth hormone.
It’s crucial for everything from cell repair to stress regulation.
Create a sleep routine that includes unwinding before bed, avoiding screens, and keeping your bedroom dark and cool.
Understanding your genetic predispositions can be incredibly empowering.
Genetic testing services allow you to get insights into how your genes influence hormone levels.
Armed with this knowledge, you can make more informed lifestyle and health choices that work for your body.
Researchers are just scratching the surface of understanding the full interaction between genes and hormones.
From alcohol consumption to mental health, scientists are uncovering more ways in which gene-hormone interaction influences our lives.
With enough research, we could even tailor medical treatments based on our unique genetic and hormonal profiles.

Ghrelin Receptor Gene: The Hunger Hormone And Eating Behaviour

Is Handedness Genetic? What Science Tells Us

Is GERD Hereditary?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4445642
https://academic.oup.com/ijnp/article/15/9/1229/670462
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6065213
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4345409
Every menstrual cycle phase brings different physical and mental changes in females. GI issues, especially bloating, are common problems for millions. Bloating during ovulation occurs mid-menstrual cycle and can cause discomfort and a constant feeling of fullness. If you struggle with fluctuating weight and body shape, your menstrual cycle could be the culprit. Know more about why the ovulation phase causes bloating and the lifestyle changes to help combat this.
Did You Know? Your genes hold precious clues about nearly all aspects of your health and wellness. Harnessing this information can help you understand your genetic makeup and decide about your nutrition, fitness, and lifestyle choices. Learn more
Bloating is a feeling of fullness or tightness in the abdomen area.
Bloating is a common problem in Americans, with 1 in 7 adults experiencing the symptoms weekly.
According to research, females are more likely to experience bloating than males (19% vs. 10.5%).
Some of the common reasons for bloating are:
Menstrual cycles are a part of the reproductive system in those with a uterus and are a preparation of the body for a possible pregnancy.
Most females have a menstrual cycle of 24-38 days.
The body goes through varied changes throughout the cycle, from day one of bleeding to the start of the next cycle.
There are different phases to the menstrual cycle; one such phase of interest is ovulation.
The ovulation phase is the fertile window where the ovary releases the egg and can fall between day ten and day 17 of the menstrual cycle.
Bloating during ovulation is a common problem faced by millions globally.
The female reproductive hormones drive ovulation.
Luteinizing hormone (LH) levels rise to help release the eggs from the ovaries and prepare them to travel toward the fallopian tube.
The follicle-stimulating hormone (FSH) and estrogen levels also increase during this phase.
Progesterone, another sex hormone, slowly increases levels from day one of ovulation to prepare the uterus for pregnancy.
Some of the physical signs of ovulation are:
Hormonal fluctuations are the reasons for most physical and mental discomforts women face in their menstrual cycles.
During ovulation, sudden surges in the reproductive hormones could be causing fluid retention in the body.
Fluid retention adds to the signs of bloating during ovulation.
Many women also see that they slightly gain weight during their mid-menstrual cycle.
The weight gain could also be because of these hormonal surges.
Increased hormonal levels lead to fluid retention in the body.
Fluid retention worsens bloating signs and contributes to slight weight gain.
A 2011 study recorded self-reported fluid retention during different menstrual cycle phases in 62 healthy women.
This study reports that fluid retention in the body was highest on the first day of menstruation and started increasing during the ovulation phase.
So, it's normal to experience sudden weight gain and signs of bloating during the ovulation phase.
Yes. It is normal to be bloated during ovulation.
For women with regular menstrual cycles, the bloating usually subsides 1-2 days after ovulation and may reappear during menstruation.
In women with conditions like polycystic ovary syndrome (PCOS) or endometriosis, bloating could be a constant discomfort throughout the menstrual cycle due to fluctuations in the sex hormones.
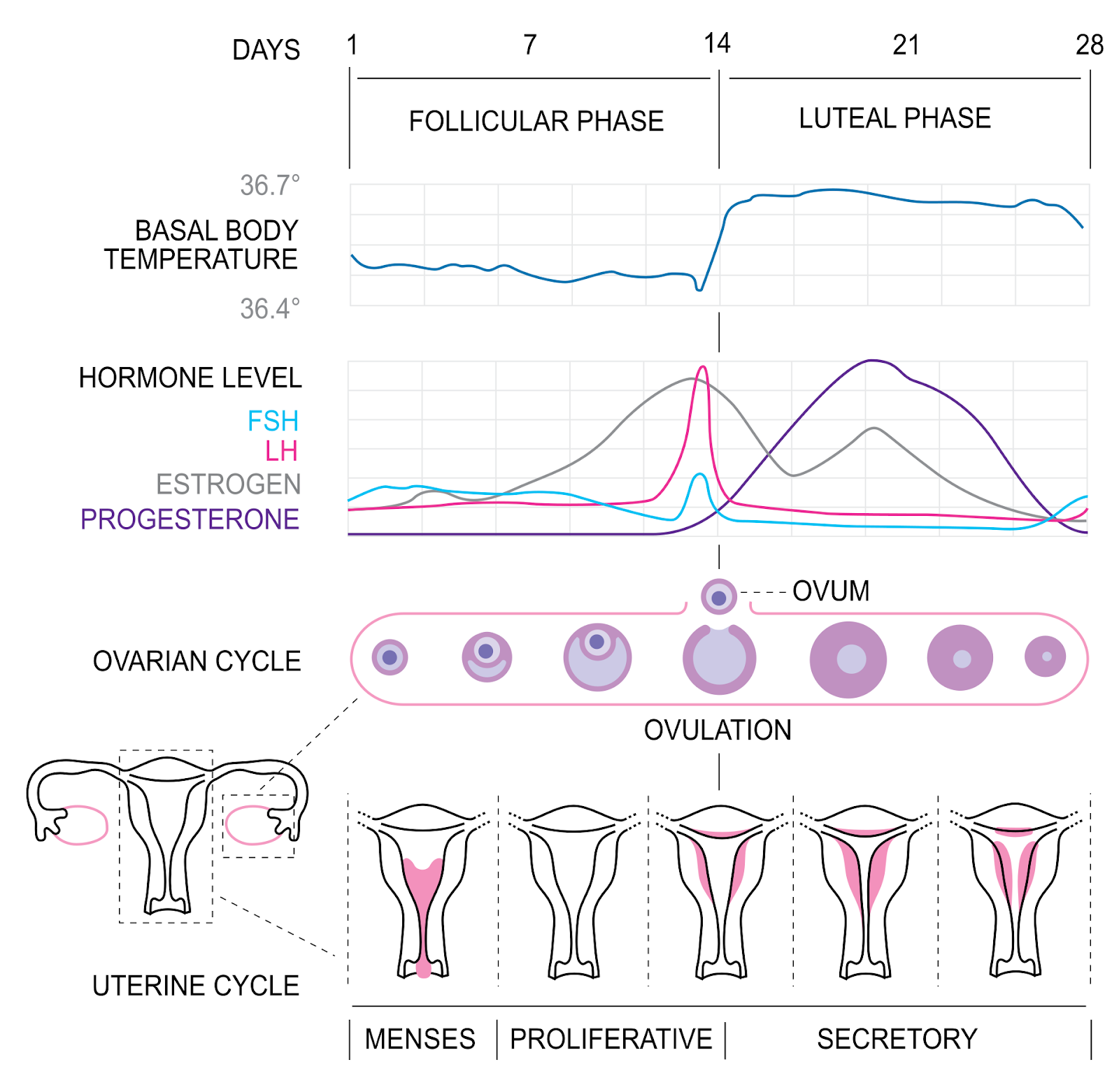
Image source: https://en.wikipedia.org/wiki/Menstrual_cycle#/media/File:MenstrualCycle2_en.svg
Premenstrual syndrome (PMS) is a group of symptoms showing up between the ovulation and menstruation phases.
3 out of 4 women may experience PMS every month, and the symptoms can range from GI issues to mood swings, breast tenderness, headaches, and body pain.
The PMS symptoms peak during the late-luteal phase, about a week before the onset of periods.
In this phase, once the body realizes that there was no successful conception, the hormone levels start fluctuating again.
The levels of progesterone, FSH, and estrogen start dropping.
This drop in hormones can cause fluid retention and bloating too.
The differences between premenstrual bloating and ovulation bloating are explained below.
| Premenstrual bloating | Ovulation bloating |
| May occur 2-7 before the onset of bleeding. | Occurs during the ovulation phase (10-17 days into the menstrual cycle). |
| Could be accompanied by cramps, mood swings, tender breasts, and food cravings. | Could be accompanied by cervical mucus changes, libido changes, slight menstruation-like cramping, and breast tenderness. |
| Can last for 2-7 days or until the start of menstruation. | Can last for 1-2 days. |
A low-FODMAP diet may help handle the signs of bloating during ovulation.
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols.
These are short-chain carbohydrates found in high amounts in foods like the ones below.
These high FODMAP foods can trigger or worsen bloating.
Instead, choose low-FODMAP foods like the following to help handle bloating.
Studies report that being physically active after a meal can help bring down the intensity of abdominal bloating.
In a 2021 study, 94 participants were divided into two groups, and one group was asked to walk 10-15 minutes after every meal.
The intervention group’s signs of bloating and fullness were reduced after walking.
Probiotics are good bacteria that are beneficial for gut health.
Probiotic-rich foods can help reduce gas production, thereby improving bloating.
Some natural sources of probiotics are yogurt, kefir, sauerkraut, and miso.
There are different ways water can help bloating during ovulation.
An excess sodium in your diet can encourage water retention in the body.
It is common to have junk food cravings and enjoy packets of crisps and other processed foods during ovulation.
However, this can be a major cause of bloating during ovulation.
https://pubmed.ncbi.nlm.nih.gov/32809533/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3154522/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC27529/
https://www.sciencedaily.com/releases/2022/11/221123213555.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6824367/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3322543/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8035544/
https://pubmed.ncbi.nlm.nih.gov/35143108/
https://www.health.harvard.edu/diseases-and-conditions/a-new-diet-to-manage-irritable-bowel-syndrome
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7122060/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3322543/
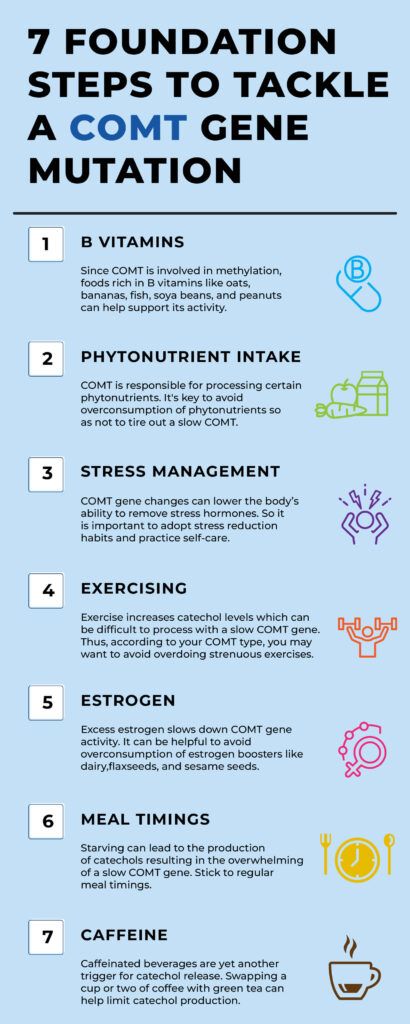
Have you ever wondered why some people are more sensitive to stress while others handle it easily? The answer might lie in a gene called COMT. COMT, short for catechol-O-methyltransferase, is a gene that plays a crucial role in regulating stress response and dopamine levels in our brains. In this blog post, we'll explore what it means to have a slow COMT gene and discuss effective strategies to navigate its effects.
What does it mean to be a COMT Warrior or Worrier? Is a warrior better than a worrier in handling stress? All your questions about the COMT gene are answered in the video below.
Catechol-O-methyltransferase (COMT) is an enzyme that regulates the breakdown of catechols.
Catechols include dopamine, norepinephrine epinephrine, and estrogen metabolites.
The COMT gene helps the body in making this enzyme.
The COMT gene provides instructions for the functioning of the COMT enzyme.
The COMT enzyme breaks down brain chemicals called catecholamine neurotransmitters.
They include dopamine, norepinephrine, and epinephrine.
The slow variant of this gene has been associated with anxiety and mood disorders.
The COMT gene produces two types of COMT enzymes.
There are three variants of the COMT gene.
| Genotype | Amino acid | Enzyme activity | Stress response and other effects |
| AA | Met/Met | Low: Worrier | Poor; lower pain threshold, more efficient at processing information under most conditions |
| AG | Met/Val | Intermediate | Average; moderate pain threshold, moderate cognitive performance |
| GG | Val/Val | High: Warrior | Good; higher pain threshold, modest reduction in executive cognition performance under most conditions |
It is important to note that even though the AA variant of COMT is associated with poor stress response, it also provides an advantage in memory and attention tasks.
The worrier variant or the COMT Met allele is also called the slow COMT gene since it results in the slow breakdown of dopamine and other catecholamines.
When you have this variant, your body has difficulty removing catechols from the system.
As a result, you are more sensitive to stress and more prone to anxiety.
About 20-30 % of Caucasians of European ancestry have the slow COMT gene.
It limits the body's ability to remove catechols.
It directly affects stress reactivity, health, and well-being of a person.
No set of symptoms can conclusively tell that you have a slow COMT gene. Only genetic tests can reveal this information.
However, there are certain symptoms that are characteristic of a slow COMT gene. They include:
COMT is a methylation gene
DNA methylation is a biochemical process required for normal development. Several B vitamins play an important role in DNA methylation.
A slow COMT gene may have difficulty removing them from the system as they trigger catechol release.
**Please consult a qualified specialist before making any significant changes to your diet. The content above is for informational purposes only and doesn’t substitute for medical advice.
If you have done an ancestry genetic test with companies like 23andMe, AncestryDNA, MyHeritage, etc., you can learn your COMT gene status in just 3 steps.
In your report, look at the “Warrior Personality” and “Worrier Personality” sections in your report.
The COMT gene plays an essential role in our health and well-being. It regulates the COMT enzyme, which removes catechols from the body.
This gene can have 3 variants: a slow variant, an intermediate variant, and a fast variant.
Having the slow variant means that your body has a hard time removing catechols. It might make you more sensitive to stress and traumatic events and predisposed to depression.
Cutting out certain protein-rich foods from your diet might help deal with a slow COMT gene.
Practicing stress reduction techniques helps deal with stress.

Is Gout Hereditary? How To Identify Your Genetic Risk

Is Photographic Memory Genetic?

Is GERD Hereditary?
https://medlineplus.gov/genetics/gene/comt/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4345409/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4759319/
https://www.snpedia.com/index.php/Rs4680
Do you wake up every morning feeling exhausted despite hours spent in bed? This isn't just a matter of inadequate sleep but could be a sign of a serious condition affecting health and quality of life. With a striking 40% of obese individuals experiencing significant sleep apnea and 70% of OSA patients being obese, the search for effective solutions becomes crucial. Could weight loss be the most powerful tool in tackling this widespread issue? Read further to see how making one significant lifestyle change might hold the secret to better sleep and improved health.
Sleep apnea is characterized by repeated breathing stoppages during sleep. It causes sleep disruptions and increases the risk of long-term health issues.
The most common form, obstructive sleep apnea (OSA), arises when throat muscles relax and block the airway.
This blockage causes pauses in breathing, resulting in low oxygen levels, which trigger the brain to wake the body just enough to restore normal breathing.
Although this response prevents suffocation, it interrupts the sleep cycle and stops the body from reaching the deep, restful sleep necessary for overall health.
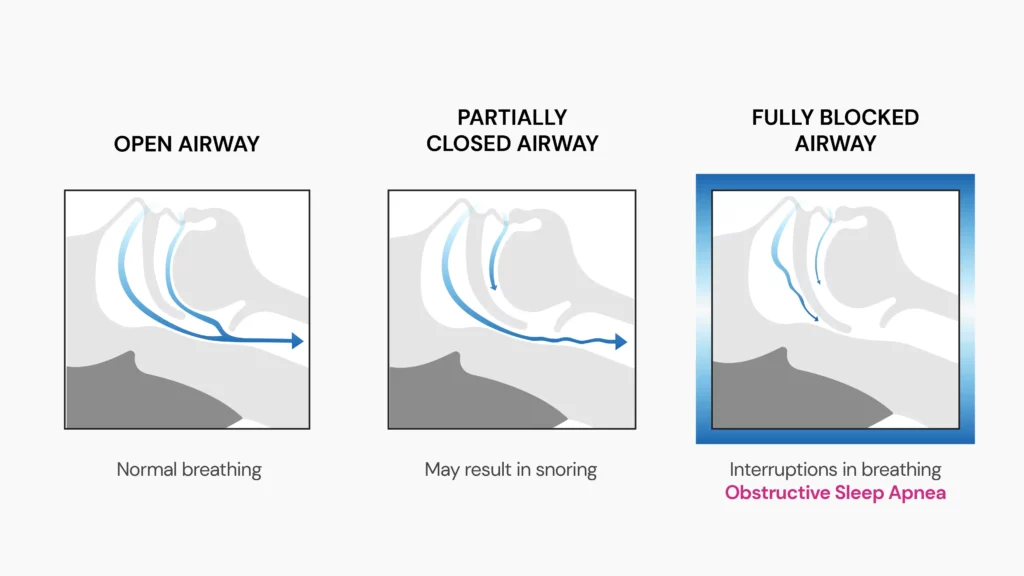
If sleep apnea remains untreated, it can contribute to serious health risks, including heart disease, hypertension, and stroke.
Common treatments for OSA focus on keeping the airways open during sleep. These include:
These treatments aim to improve sleep quality and prevent the health risks associated with sleep apnea.
This relationship is complex and multifaceted, as each condition can exacerbate the other, worsening symptoms and overall health.
Obesity, characterized by excessive body fat, particularly around the neck and abdomen, can significantly increase the likelihood of developing OSA.
Conversely, OSA can lead to weight gain and make it more difficult for individuals to lose weight, creating a vicious cycle that is hard to break.
Excess fat around the neck and upper body can put pressure on the airways and cause them to collapse during sleep, leading to breathing interruptions and apnea episodes.
Studies have shown that for every 1-point increase in body mass index (BMI), the risk of OSA increases by 14%.
Obesity or being overweight contributes to OSA in the following ways:
Sleep apnea can lead to weight gain through several mechanisms:
Weight loss is an effective strategy for managing obstructive sleep apnea (OSA), particularly for individuals who are overweight or obese.
According to a mathematical model, for every 7-pound drop in weight, there is a corresponding 7% decrease in the apnea-hypopnea index (AHI), which measures the severity of sleep apnea.
Let us see how weight loss helps treat sleep apnea.
It is important to note here that while weight loss significantly improves OSA, it may not fully resolve the condition for everyone.
Other treatments, such as CPAP therapy, may still be necessary.
Combining dietary changes, increased physical activity, and behavioral therapy can significantly improve weight loss and sleep apnea symptoms. Here’s how:
A calorie-restricted, well-balanced diet is fundamental for weight loss, particularly for those managing sleep apnea.
Aiming for around 1,200–1,500 calories* per day for females and 1,500–1,800 calories* for males is recommended. This approach helps reduce excess body fat, which is often linked to the worsening of sleep apnea.
*The exact calorie requirement for weight loss varies from person to person. Please consult a qualified nutritionist before making any significant changes to your diet
Physical activity is vital to both weight loss and improving the body's overall functioning.
Regular exercise burns calories and strengthens muscles that help maintain open airways during sleep.
Behavioral therapy can be instrumental in developing sustainable weight loss habits and overcoming mental or emotional barriers that may affect weight management.
While weight loss is a critical intervention, there are additional lifestyle changes and therapeutic approaches that can amplify its effects.
Let’s take a closer look at these strategies:
However, CPAP therapy and other sleep apnea treatments may still be necessary in some cases, especially when OSA is moderate to severe.

Is Sleep Apnea Genetic? Risk Factors, Treatment, And More

Can Sleep Apnea Lead To Brain Damage?

Can Vitamin B12 Help In Weight Loss?
https://www.ahajournals.org/doi/full/10.1161/01.hyp.0000101686.98973.a3
https://my.clevelandclinic.org/health/diseases/8718-sleep-apnea
https://www.nhlbi.nih.gov/health/sleep-apnea/treatment
https://www.sleepfoundation.org/sleep-apnea/weight-loss-and-sleep-apnea
https://www.atsjournals.org/doi/10.1164/rccm.201903-0692OC
https://www.healthline.com/health/sleep-apnea/sleep-apnea-weight-loss
https://www.hopkinsmedicine.org/health/wellness-and-prevention/choosing-the-best-sleep-position
https://www.nature.com/articles/s41598-023-34956-5
https://www.sleepapnea.org/snoring/mouth-exercises-to-stop-snoring/
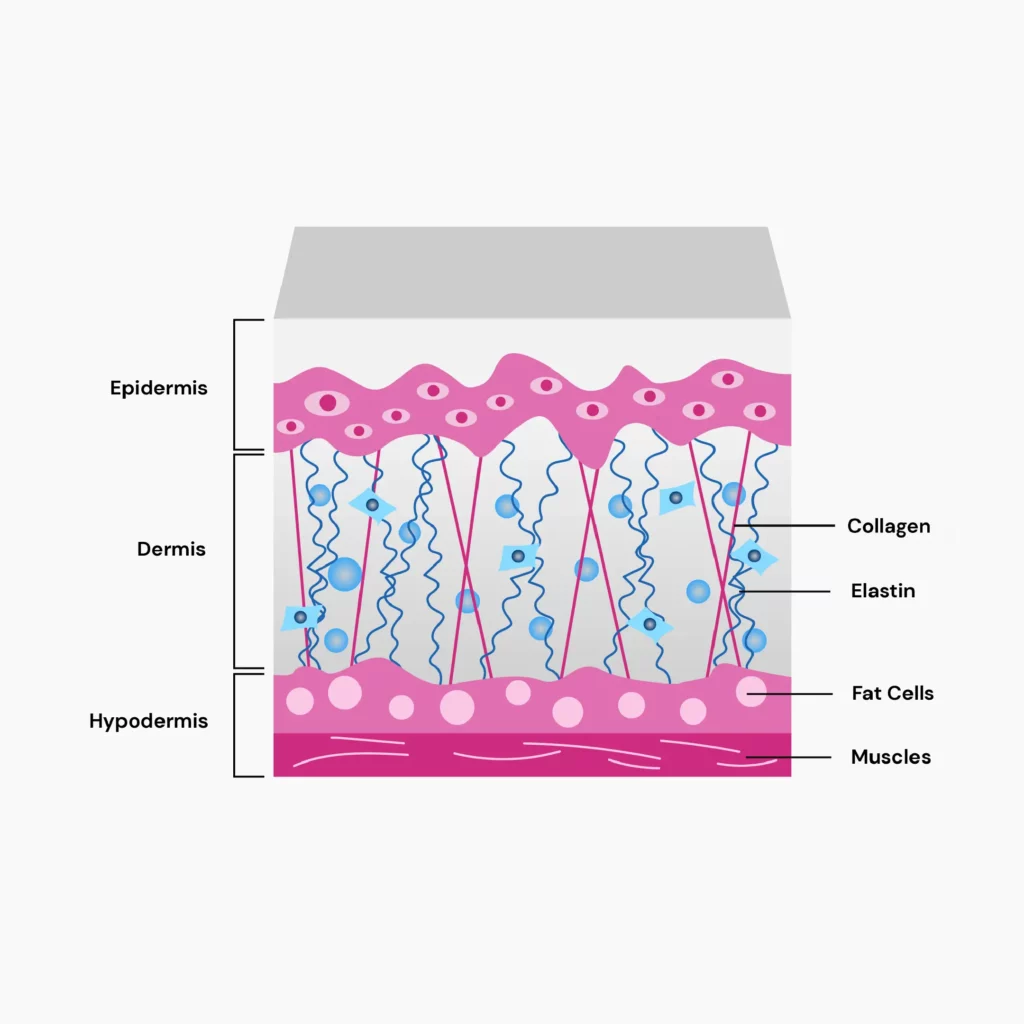
What is common in up to 90% of those who are pregnant, 70% of adolescent females, and, surprisingly, 40% of males? Stretch marks! Also known as striae distensae, stretch marks are often a result of sudden weight gain, pregnancy, or growth spurts. Despite this high prevalence, how do some people manage to avoid stretch marks altogether? Is it due to a religious coconut oil sugar scrub routine, or are there some hidden genetic factors at play? This article delves into the hereditary nature of stretch marks and explores whether they could be genetic.
Striae distensae or stretch marks are scars that develop in the skin when it expands or shrinks. This puts excess pressure on the collagen and elastin that support the skin, ultimately causing breakage in them. This leads to the appearance of scars.
While stretch marks are not medically serious, they can affect a person’s appearance. Females are at a higher risk of developing stretch marks than males.
Stretch marks commonly appear on the abdomen, breasts, shoulders, and thighs. In children experiencing growth spurts, you can also see stretch marks on the thighs and buttocks.
Stretch marks start out as thin pink or pale-colored lines on the skin. As they develop, lines perpendicular to the skin tension start developing.
These lines look slightly swollen and can turn pink or purple in color. Mature stretch marks are pale-white in color.

Genetics is one of the most significant factors that contribute to stretch mark development. There's no one "stretch mark gene," but a group of genes that regulate skin elasticity, collagen, etc., together influence the risk of stretch marks.
According to a study, females with a family history of stretch marks were more likely to develop them during pregnancy, further supporting the role of genetic factors in the development of stretch marks.
Let's explore some genes known to be involved in stretch marks.
The ELN gene helps produce a type of protein called tropoelastin.
Multiple copies of this protein join together to become elastin fibers. They provide stretch, recoil, and elasticity to the skin.
Certain changes in the ELN gene can interfere with the normal functioning of elastin protein, leaving the individual susceptible to stretch marks.
The T allele of the rs7787362 SNP (an SNP is a single-letter change) in the ELN gene is associated with an increased risk for stretch marks.
The FN1 gene produces two types of proteins - cellular fibronectin-1 and plasma fibronectin-1.
Plasma fibronectin-1 attaches itself to other proteins in the skin, including.
This helps strengthen the tissues and helps repair them, too.
Certain changes in this gene result in lower fibronectin levels, which may result in poor tissue repair, increasing the risk of stretch marks.
The A allele of the rs3910516 SNP in the FN1 gene is associated with an increased risk for stretch marks.
Pregnancy is the biggest non-genetic influence on stretch marks.
But the tendency to develop even pregnancy stretch marks can be genetic!
About 90% of women develop stretch marks during pregnancy and continue handling them for the rest of their lives.
Women with larger abdominal areas and more weight gain during the pregnancy period develop severe striae distensae.
Up to 43% of people who are overweight and obese develop striae distensae in their lifetimes.
The increase in weight puts more stress on the skin.
As a result, it stretches it beyond its usual capacity, leading to stretch marks.
Cushing syndrome is a result of excess cortisol hormone in the body.
Cortisol is an important hormone that reduces inflammation, regulates blood pressure, and helps the body handle stress.
Cortisol-based drugs are prescribed to handle inflammatory diseases and chronic pain. Sometimes, the body overproduces this hormone. This results in Cushing syndrome.
The main symptom of Cushing syndrome is the development of stretch marks (pink and purple lines) all over the breast, buttocks, abdomen, thighs, and shoulders.
Some conditions like anorexia nervosa, Marfan syndrome, and chronic liver diseases can make an individual prone to developing stretch marks.
Corticosteroid creams, lotions, and gels are prescribed to treat conditions like eczema, itching, dermatitis, and psoriasis.
Corticosteroids can decrease the skin’s ability to stretch and cause stretch marks.
Those opting for breast enlargement surgeries are at higher risk for developing stretch marks.
Placing an implant under the breast skin causes it to stretch and cover the larger area.
This can lead to the development of striae distensae.
Losing and gaining weight gradually will give your skin time to adjust to the new changes and prevent the appearance of stretch marks.
Natural remedies work only in the initial stages of stretch marks and not on mature marks. While they may not be able to get rid of the marks completely, they may improve their appearance. Here are a few options you can try out.
There are two ingredients in topical creams that seem to be effective.
They are available as over-the-counter medications. These are also only most effective when applied as soon as you spot signs of stretch marks. As the marks get more mature, treating them will be difficult.
Microdermabrasion is performed by an expert in a clinical setting.
This involves removing the top layers of the skin to help finer and better skin grow back.
Microdermabrasion can help bring down the intensity of striae distensae scars.
Chemical peels are being used widely to bring down the prominence of stretch marks.
These peels remove the topmost or the subsequent layers of the skin and give a faded appearance to stretch marks.
They cannot completely remove the marks, though. Regular chemical peel treatments can harm the skin.
As of now, there is no recommended treatment or lifestyle change that can completely remove stretch marks or prevent them from appearing.
Maintaining a healthy weight, keeping the skin moisturized and hydrated, and treating the early signs of stretch marks help.
*please consult a qualified dermatologist for the best course of action. This is intended for informational purposes only
Hand-picked Content For You: Widows Peak Genetics: Is There An Evolutionary Significance?
https://www.mayoclinic.org/diseases-conditions/cushing-syndrome/symptoms-causes/syc-20351310
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5181654/
https://www.aad.org/public/cosmetic/scars-stretch-marks/stretch-marks-why-appear
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6615396/
https://www.mayoclinic.org/diseases-conditions/stretch-marks/diagnosis-treatment/drc-20351144
https://emedicine.medscape.com/article/1074868-treatment#d9
https://www.ncbi.nlm.nih.gov/books/NBK436005/
https://pubmed.ncbi.nlm.nih.gov/23579949/
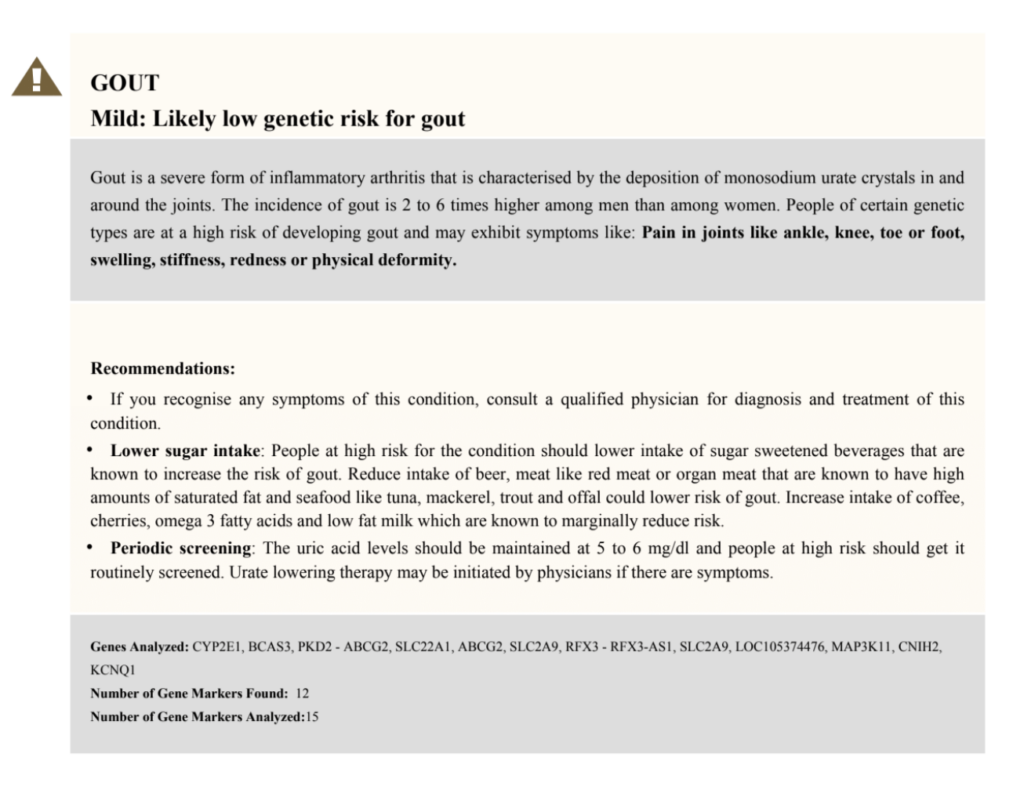
Gout is often thought to be the "disease of kings" due to its association with gluttony and alcohol consumption. This stigma has prevented us from exploring its root cause for many years. Research in the last decade suggests the cause of gout is a lot more genetics than just diet. Gout can affect anyone, but if you have an affected first-degree family member, your risk increases by 2.5x! This begs the answer to the question, "Is gout hereditary?" While we attempt to discuss this, we'll also touch upon how to learn your risk for gout via a genetic test.
Gout is one type of arthritis that results in inflammation, tenderness, and redness of one or more joints (ankles, wrists, fingers, and knees), most frequently the big toe joint.
People with gout have high levels of a chemical compound called urate or uric acid in their blood (hyperuricemia).
Generally, uric acid dissolves in the blood and is excreted by the kidneys through the urine.
But sometimes, the body produces excess uric acid, or the kidneys excrete too little uric acid.
During this stage, uric acid builds up, and forms sharp, needle-like structures called urate crystals that accumulate in joints, and the immune system reacts by causing inflammation.
Types of gout:
With a strong genetic influence, gout is a condition that can be inherited. The heritability of gout is 65%!
Although there's no clear inheritance pattern, studies suggest that having a close affected family member can increase your risk significantly.
An estimated 20% of gout sufferers have a relative with the condition.
To explore the heritability of gout, a group of researchers analyzed 4.2 million families.
Study Observations
A meta-analysis published in 2018 suggests that the impact of genes on gout was much more significant than that of diet.
The study was done on 16,760 individuals with European ancestry.
They were exposed to several food items, some of which increased serum urate levels and others that it.
The researchers observed that diet only contributed to ≤0.3% of the variance in urate levels; by contrast, genetics contributed to a whopping 23.9% of the variance!
Genes that produce proteins that are responsible for urate transport play a prominent role in gout.
Urate transporters mediate urate excretion.
A variation in one of these urate-related genes may cause gout.
The genes that have so far been identified to have the strongest association with gout include
The SLC2A9 gene produces a protein called GLUT-9, which is found in the kidneys.
This protein regulates the reabsorption of urate from the urine back into the blood.
It also assists in the removal of urate through urine.
A mutation in the SLC2A9 gene may result in increased urate reabsorption or decreased urate excretion.
This could lead to hyperuricemia and, eventually, gout.
The ABCG2 gene produces a multifunctional transporter protein called ABCG2, primarily in the stomach and liver.
The protein regulates the excretion of urate via stools (or poop).
If the ABCG2 gene is altered, the protein won't be able to release urate into the intestines as it should.
As a result, urate excretion may decrease, increasing serum urate levels and leading to gout.
Gout sufferers frequently experience sudden, excruciating pain attacks that start at night and last for up to 12 hours.
This extreme discomfort, which usually begins at night, is a significant symptom of gout.
Most people only have pain in one particular joint. Your big toe is commonly where it starts, although it can happen anywhere.
Other gout symptoms include:
Did You Know?
Many chronic conditions like diabetes, hypertension, or gout are influenced by many gene changes. Each change adds to the risk of developing the condition. You can learn your risk for these conditions as well as recommendations to lower your risk using your existing ancestry test DNA data.
Learn How.
Now that we have seen that family history and genes play a vital role in gout risk let's explore some of the other factors that can contribute to the risk.
At present, no genetic test can confirm with 100% accuracy whether or not you'll get gout. But, it can really be helpful in understanding your risk for the condition.
These tests analyze commonly-associated genes with gout to identify the presence of genetic variants, if any.
If you possess a genetic variant, you may be at risk for gout.
You can then discuss the results with your doctor, who, after considering your medical, family, and personal history, can recommend steps to lower your risk and prevent gout.
Researchers have identified several genes associated with gout.
Xcode Life's Gene Health report, which analyzes your genetic risk for over 45+ health conditions, can help you understand your gout risk.
You can identify your genetic risk of gout by using your 23andMe (or any ancestry test) DNA data and placing an order for the Gene Health Report.
A Sample Gout DNA Report

Is GERD Hereditary?

How To Prevent Gout Flare-Ups: Probiotics Could Be The Key

Is Lupus Hereditary? An Overview of Genetic Factors