Did you know that cataracts are the leading cause of blindness worldwide? This common aging-related condition affects more than half of all Americans 80 years and older. While no clear causative factor has been identified, studies have reported over 100 genes that can increase the risk of cataracts. Mutations in these genes can be passed down in the family, suggesting that some cases of cataracts may be hereditary. The article discusses the genetic landscape of cataracts and outlines some possible preventative measures.
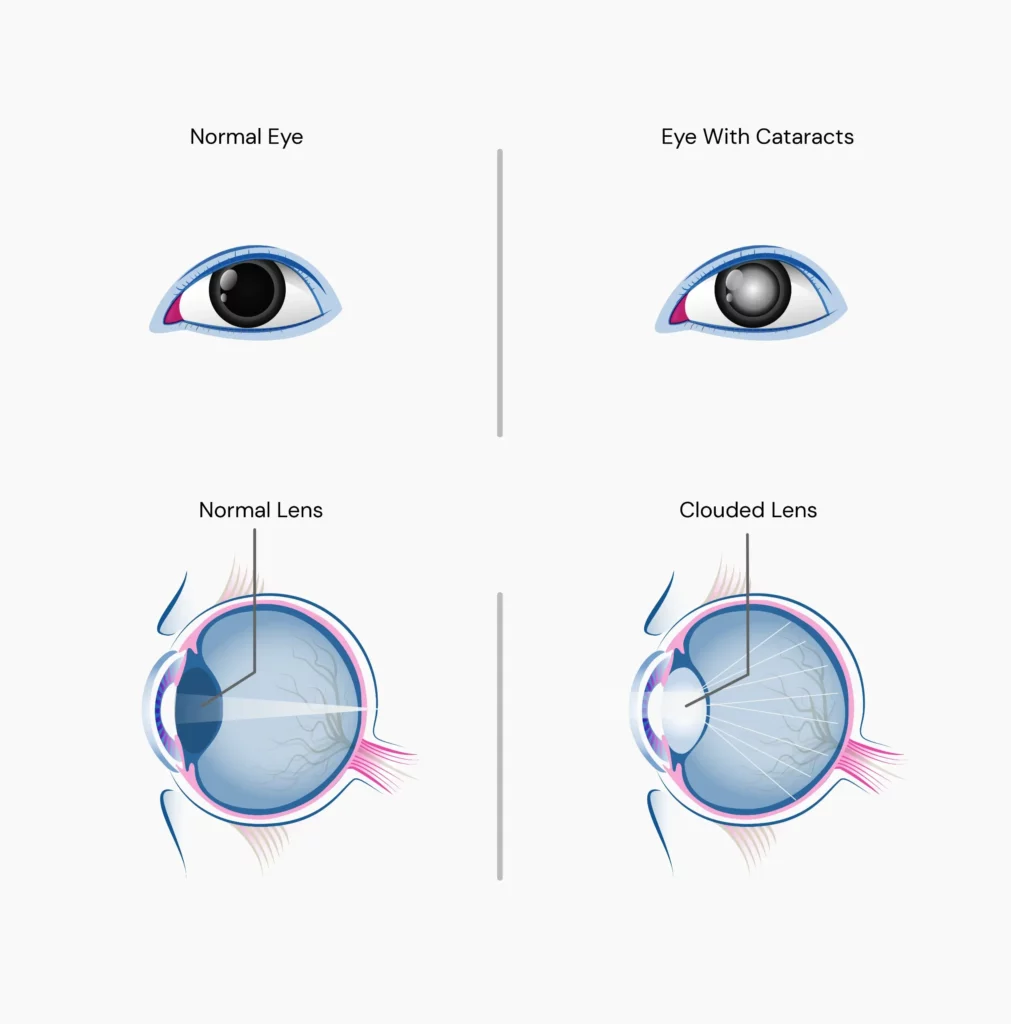
In a normal, healthy eye, the lens is clear.
In cataracts, the lens gets clouded due to an eye protein that breaks down and clumps together as a part of the aging process.
As a result, the light rays cannot pass through the lens and focus on the retina (the tissue that acts as the screen for images in the eye).
In the initial stages, cataracts do not cause any issues.
However, as they grow over time, it affects more of the lens, making it difficult for you to see.
While cataracts do not spread from one eye to the other, some people may develop cataracts in both eyes.
There are four types of cataracts:
The following symptoms are commonly noted in the case of cataracts.
If you experience two or more of these symptoms, it is recommended to get them checked by an ophthalmologist:
Though the exact cause of cataracts is unknown, a few potential reasons why they occur include:
More research is required to understand the causes of cataracts.
Aging is the most common cause of cataracts.
This condition is due to cumulative changes that occur in the eyes after 40 years of age.
Congenital cataract, on the other hand, is present at birth.
This type of cataract is rare and may be present as part of birth defects in Down Syndrome, Trisomy 13, Pierre-Robin Syndrome, Chondrodysplasia syndrome, and others.
Yes, cataracts can be hereditary.
Congenital cataracts, which occur at birth, are often caused by genetic mutations and can run in families.
Additionally, age-related cataracts may also have a hereditary component, as genetic factors can influence the shape and integrity of the lens, making it more susceptible to clouding.
Research has identified over 115 genes and 38 disease-causing genes associated with cataract formation. A twin eye study demonstrated that heritability accounts for 53% to 58% of the cortical cataracts risk and 48% of nuclear cataracts risk.
Yes, cataracts can run in families.
Hand-picked Article For You: Is Eye Color Genetic?
Abnormal changes (mutations) in crystallins (a type of eye lens protein) or other lens proteins may lead to protein aggregation.
This results in congenital cataracts.
When these genetic mutations increase the susceptibility of the eye to environmental insults like light, oxidative or hyperglycemic damage, they may result in age-related cataracts.
Hereditary congenital cataracts are inherited in Mendelian fashion, while age-related cataracts are influenced by multiple genes and environmental factors.
Several genes have been identified to cause congenital cataracts:
Unfortunately, there is no way to prevent hereditary cataracts.
However, timely detection and treatment of hereditary cataracts may help restore clear vision.
Besides genetics, several other factors may increase your risk of developing cataracts.
Your risk of cataracts increases with age.
Other risk factors for cataracts include:
Related Read: Double Eyelashes (Distichiasis) – Why Does It Happen?
While you cannot prevent cataracts from occurring, you can reduce your risk for the same.
Here are some ways to do so:
Let’s be real. We have all tried one of those “trendy” diets that seem to do miraculous things to your health - be it a significant drop in weight or a healthy and “natural” glow to your skin. But how many of us actually have been able to lose weight on such diets or avoid weight regain? You may not see too many hands go up for this one. The reason is everyone's body is unique and has different needs when it comes to nutrition. What works for one person may not work for another. Their paths to success might differ due to their unique genetic makeup. This is where nutrigenomics, the science exploring the interplay between genes and diet, steps in. Studying gene reactions to different diets (low-fat, low-carb) helps personalize dietary advice based on your unique genetic makeup. Continue reading to learn about nutrigenomics, its testing benefits, disease prevention role, and day-to-day applications.
Did You Know?
The interaction between your diet and genes impacts everything from weight management and vitamin needs to food intolerances and eating behavior. You can use your existing ancestry test DNA data to unlock all this information with Xcode Life's Gene Nutrition report. Learn more.
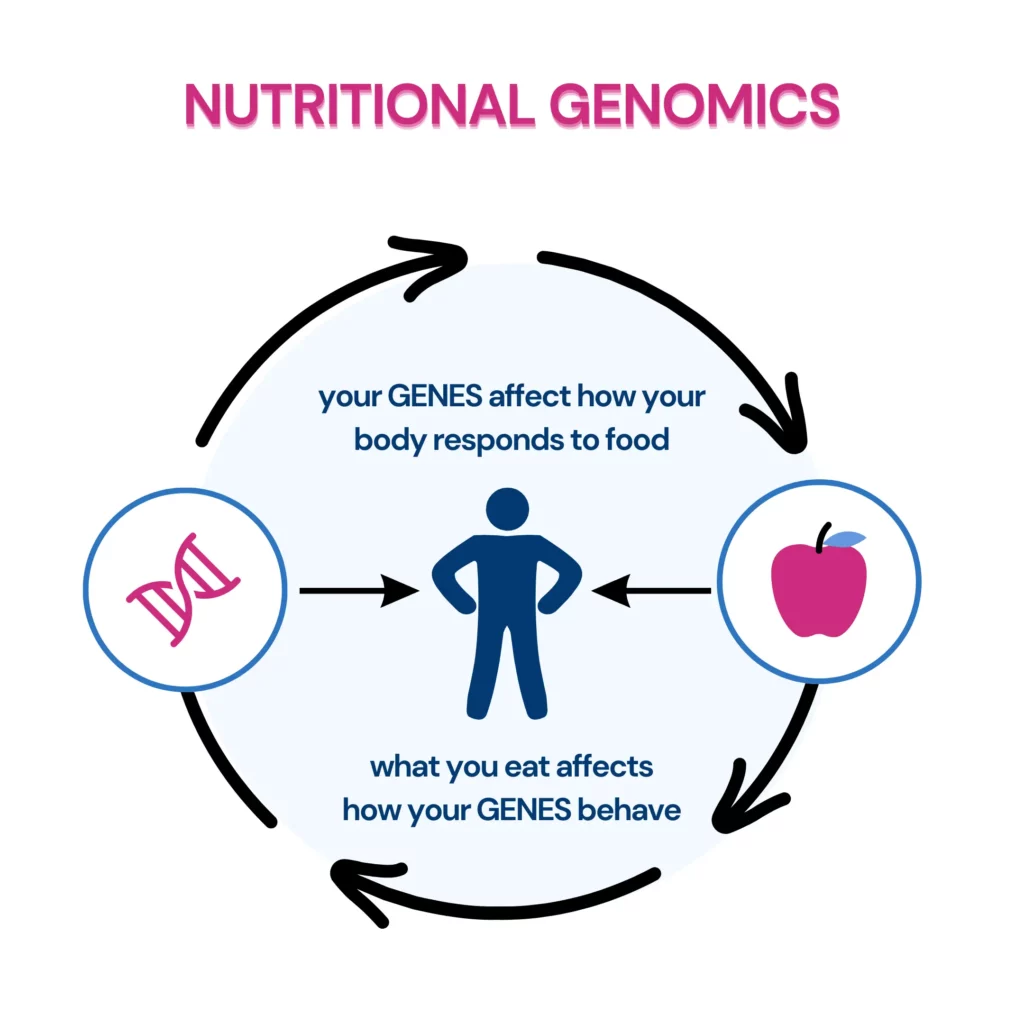
Nutrigenomics, or nutritional genomics, studies how food and genes interact.
It tells us there's no one perfect diet because we all have slightly different genetic makeups. What works for your friend's body might work differently for yours!
Here's a simple way to think about it:
So nutrigenomics tries listening to this nutrient-gene conversation to customize nutrition advice.
Nutrigenetics and nutrigenomics explore the complex relationship between nutrients and our genetic makeup, but they do so from distinct perspectives.
Nutrigenetics:
Nutrigenomics:
Nutrigenomics is increasingly influential in modern health and nutrition, offering personalized healthcare and disease prevention possibilities. Here’s how:
While still growing, nutrigenomics promises personalized nutrition and preventive medicine, improving health outcomes.
Remember, consulting healthcare professionals before dietary changes based on genetic information is crucial.
Our genes affect just about every aspect of nutrition, from how our bodies break down macros and micros to food intolerances and preferences.
For example, if a person has an excess of caffeine-metabolizing enzyme, they may be able to drink seven cups of coffee a day without experiencing any jitteriness or sleep issues.
On the other hand, if they are deficient in lactase-producing genes, they may not be able to add milk to their coffees without experiencing abdominal discomfort.
Another gene called FTO has garnered attention for its role in body weight regulation.
Variations in this gene can influence a person's metabolism, how they burn energy, and their overall energy balance, all of which contribute to weight management challenges or advantages.
Each individual carries a distinct combination of genetic "pros" and "cons" when it comes to nutrition and metabolism.
Nutrigenomic analysis allows us to make more informed dietary choices to enhance health and mitigate disease risks.
While genetics are undoubtedly a crucial piece of the puzzle, it's also clear that lifestyle and environmental factors significantly shape how our bodies respond to what we eat.
Genetic predispositions, which some may view as "disadvantages," can often be mitigated with strategic diet and lifestyle modifications.
For example, if a genetic variant tends to predispose you to overeat, incorporating foods that are high in satiety in your main meals and opting for healthier snacks can help curb this tendency.
Nutrigenomics opens the door to a more personalized approach to nutrition, emphasizing the power of understanding our genetic profiles.
It teaches us that while we may have genetic predispositions that influence our nutritional health, we are not bound by our DNA.
With the insights provided by nutrigenomics, combined with mindful lifestyle choices, we can take control of our health, turning genetic knowledge into a tool for personalized wellness strategies.
Direct-to-consumer genetic testing companies like Xcode Life now allow users to order a nutrition genetic test without requiring a doctor’s help.
Genetic testing looks at your DNA to find mutations (variations) that could lead to health issues.
Nutrigenomic testing is a genetic test that shows your specific nutritional needs.
It's done by swabbing your cheek and sending the sample to a lab to examine specific nutrition-related genes.
After sequencing the genes, lab companies and healthcare providers in nutrigenomics analyze the results to understand what they mean for your health.
To take a nutrigenomics test, you typically need to provide a saliva or blood sample. The phlebotomist provides the testing tool kit.
Most saliva tests are done using at-home DNA test kits.
This sample is analyzed in a laboratory to identify specific genetic variations related to nutrition and health.
DNA data analysis companies such as Xcode Life allow users to upload their existing genetic ancestry test DNA data to provide insights on 48 crucial nutrition aspects.
The cost of nutrigenomics testing can vary depending on the provider and the comprehensiveness of the test. Prices typically range from $300 to a few thousand dollars.
Xcode Life's Gene Nutrition Report: 48 Traits for $40
(DNA kit not included; only for those who have already taken a DNA ancestry test)
As individual needs and goals vary, no single best test exists. To find your perfect match:
Nutrigenomics can provide insights into how your genes influence metabolism and appetite regulation.
This, in turn, impacts fat-burning efforts.
Further, it also helps identify your ideal macro breakup by shedding light on how well your body processes carbs, fats, and protein.
However, it's not a guaranteed solution and should be combined with a healthy lifestyle. Remember, research is ongoing, and its definitive role in weight loss currently has limited evidence.
According to the Current Research In Nutrition And Food Science, nutrigenomic studies help prevent diseases like type 2 diabetes, hypertension, gestational diabetes, and cardiovascular diseases.
Similarly, diet plays a role in about 30–40% of all cancer cases. Numerous studies suggest that breast, prostate, liver, colon, and lung cancers are associated with dietary habits.
Nutrigenomics can assess a person's unique nutritional needs based on their genes, creating a personalized diet. It also aids in treating and preventing chronic diseases.
The role of Nutrigenomics in Disease Prevention is as follows:
Since recognizing the right to food in 1948, there has been major progress in making food available worldwide.
International trade and organizations like the Codex Alimentarius Commission have helped ensure food safety and nutrition globally.
However, in recent years, challenges have arisen, such as increased consumption of processed foods and sedentary lifestyles.
The same has resulted in more lifestyle-related diseases, especially in developing countries.
With advances in understanding how food, nutrition, and genes interact, a new field called Nutritional Genomics or Nutrigenomics has emerged.
This field focuses on personalized dietary interventions based on genetic makeup to manage nutrition-related diseases and improve health outcomes.
The practical applications of nutrigenomics in daily life include:
Nutrigenomics is exciting, but integrating it into public healthcare poses several crucial ethical and regulatory challenges. Here's why:
By tackling these challenges, we can make sure everyone benefits from the exciting possibilities of nutrigenomics.
About 60% of deaths worldwide resulted from lifestyle-associated chronic diseases, double that of infectious diseases.
Nutrigenomics is no science or magic that can be a one-stop solution for all your health issues. Your lifestyle and environmental factors play a significant role, too.
Prolonged exposure to a poor lifestyle and environmental conditions can harm your health despite eating a good diet.
These dos and don'ts can help you maintain healthy genes and body:
Nutrigenomics is the study of how nutrients influence genetic makeup.
Nutrigenomic testing is a genetic test that shows your specific nutritional needs. It's done by swabbing your cheek and sending it to a lab to examine around 70 or more specific genes.
The testing helps you identify your nutritional needs and get a personalized diet plan for yourself. The diet plan can also help in weight balance and disease control.
However, nutrigenomics alone cannot be a one-stop solution for all your health issues. It's also essential to check your lifestyle and environmental conditions.
https://pubmed.ncbi.nlm.nih.gov/23113033
https://www.mdpi.com/1422-0067/21/7/2633
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/metabolome
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/proteome
https://www.genome.gov/genetics-glossary/Genome
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1193991
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3481686
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7071525
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4210933
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5634986
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4869012
Superfood is a term used to describe a nutrient-dense food item that can help protect you against multiple health concerns. While many exotic foods are claimed to be superfoods by social media, not all of these claims are supported by science. Spirulina has long been used as a source of nutrition in many cultures worldwide. Researchers have found that Spirulina is a superfood and can do wonders for your health. It also has proven health benefits specifically for men, making Spirulina an incredible superfood.
Spirulina is a type of blue-green algae that is also one of the oldest life forms on earth.
It is a type of cyanobacteria, a single-celled microbe colloquially termed blue-green algae.
Spirulina has been a food source in Mexico and South Africa for centuries.
It has numerous health benefits, is often used as a supplement, and is a common ingredient in smoothies and energy bars.
According to the US Department of Food and Agriculture, one teaspoon of Spirulina contains:
Spirulina is usually available as a powder.
Mix it in a glass of water, add it to your morning oatmeal or smoothie, or sprinkle it on salads.
Most people find Spirulina neutral, so it won’t affect the taste of the food you add it to.
It can take 1-3 weeks, or sometimes more than that, for Spirulina to affect your overall health.
Spirulina's effects on health depend on health, physical activity, and food consumption.
You will see faster results if you follow a healthy lifestyle and take spirulina supplements.
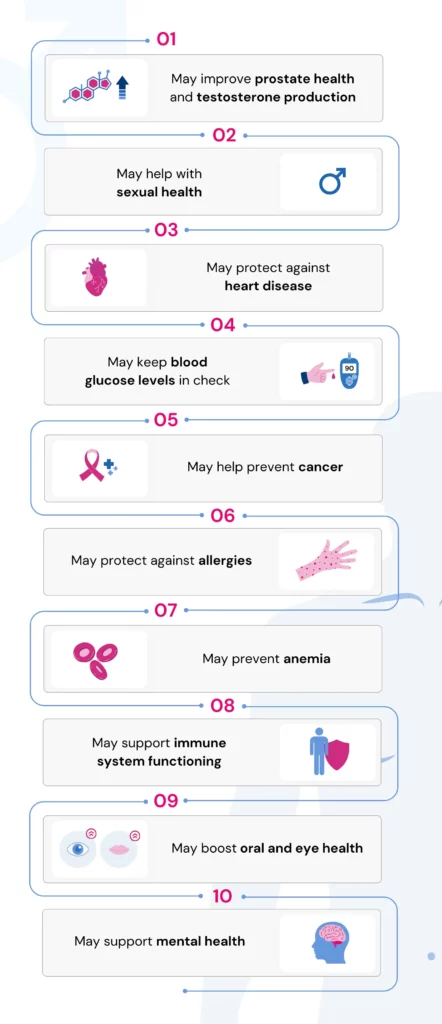
Consuming Spirulina can be highly beneficial for your health.
However, it can also come with certain risks.
During Spirulina’s growth in marine water, it can accumulate heavy metals, harmful bacteria, and microcystins that can damage your liver.
Spirulina is an anticoagulant with blood-thinning properties, so those with clotting disorders should avoid it.
Spirulina also contains an amino acid called phenylalanine, which can be harmful to those with the genetic disorder phenylketonuria.
You should not take Spirulina if you are
Always consult your healthcare provider before starting any supplements.
Spirulina can increase the production of testosterone in men.
This, in turn, can improve athletic performance and sexual health.
Spirulina is rich in antioxidants that lower inflammation in the body.
When taking Spirulina regularly, you may notice less joint pain and bloating and clearer skin.
Over time, Spirulina may improve your heart and gut health and help you lose excess weight.
Research shows that Spirulina can help strengthen your muscles.
In one study, men took a 6-gram spirulina supplement every day for a month.
They reported enjoying more extended periods of exercise without fatigue than those who didn’t take the supplement.
Spirulina contains up to 4 grams of protein per tablespoon.
Consuming it may increase stamina and improve athletic performance.
Spirulina, a single-celled microbe, has long been a food source in many cultures.
Now, scientists have found that Spirulina has a lot of health benefits, especially for men.
Spirulina is rich in antioxidants and can reduce inflammation in the body, improving heart health.
It can also help control diabetes and protect against cancers.
In men, it can improve prostate health and increase testosterone production.
Spirulina is usually safe for consumption.
However, as with all supplements, it is a good idea to consult your doctor before taking Spirulina.
https://pubmed.ncbi.nlm.nih.gov/20010119
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6241722
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3576896
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8212345
FamilyTreeNow is a free and popular website designed to assist individuals in constructing their family trees and unearthing intriguing genealogical secrets. Offering access to a treasure trove of public records and a user-friendly family tree builder, FamilyTreeNow has sparked both excitement and controversy. From concerns about data accuracy to questions surrounding privacy, it's a platform that has left users intrigued yet cautious. Here is everything you need to know about FamilyTreeNow, its services, data privacy concerns, and ways to opt out of their services.
FamilyTreeNow is a website that helps trace ancestries, build family trees, and get contact details of millions of individuals.
Launched in 2014, this genealogy website is based in Roseville, California, and has over 1.6 billion personal records in its database.
Yes. FamilyTreeNow is a free website allowing individuals to search for people and build and store their family tree without paying anything.
FamilyTreeNow offers two primary services - people finder and family tree builder.
Follow these easy steps to search for records on FamilyTreeNow’s database.
Below are the steps to use the family tree builder service.
Recommended for you: How to download your Family Tree DNA Raw Data?
Unlike other genealogy websites, FamilyTreeNow does not ask for a fee to utilize any of their services.
Some genealogy websites have free services but require customers to upgrade to premium services for a fee. FamilyTreeNow doesn’t offer such premium services either.
According to the website's founders, their mission is to create the best genealogy website in the world that both amateur and professional genealogists can utilize.
The accuracy of FamilyTreeNow’s records depends on two factors.
The controversy surrounding FamilyTreeNow primarily revolves around the accessibility and potential misuse of personal information available on the site.
It has raised significant privacy concerns due to the ease with which personal details can be obtained.
Additionally, the website has been linked to cases of stalking and other malicious activities, sparking apprehension regarding the security and ethical implications of its services.
Furthermore, the owner of FamilyTreeNow, Dustin Weirich, has faced criticism for being unresponsive to requests for comment, which has fueled skepticism about the platform's commitment to addressing privacy and security issues.
FamilyTreeNow's website tells you exactly how you could opt out of its services, so your information isn’t visible to those who search for it.
Here are the detailed steps to opt out.
The internet is split in its opinion, having a free-to-access genealogy website.
Global genealogy enthusiasts are excited about having a free tool that helps them pursue their passion for genealogy.
However, a larger group of people are worried that this free database will give anyone access to your details, including your address, contact number, and relationships.
Here are some pros and cons of using FamilyTreeNow to help you make an informed decision.
| Pros | Cons |
| Unlimited free access to create a family tree and search for ancestry details | Risk of data privacy |
| Quick access to multiple public records all in one place | Since the database depends on open public records, it may be hard to eliminate inaccuracies and incomplete information |
| Advanced search features make it easy to narrow down search results | FamilyTreeNow does not have extensive customer support features like other paid websites |
https://www.familytreenow.com/
https://blog.incogni.com/family-tree-now-opt-out/
https://www.lifewire.com/family-tree-now-4129031
https://www.trustpilot.com/review/www.familytreenow.com
Did you know that not all natural supplements are as safe as they seem? While some can offer health benefits, others might harm your liver, the most vital organ responsible for cleansing your body. NIH research has revealed that liver injury induced by herbal and dietary supplements (HDS) accounts for 20% of hepatotoxicity cases in the United States. This means being cautious about your supplements, which is crucial for safeguarding your liver health. Keep reading to explore 7 natural supplements that may cause liver damage, either directly or through interactions with other medications. Additionally, we'll address liver damage signs, delve into liver-stressing vitamins, and provide practical supplement selection tips for liver health maintenance.
While many turn to natural supplements for improved health, some contain unexpected downsides.
It's important to be aware of potential side effects, especially those impacting the vital liver.
Here are 7 commonly used supplements that, under certain circumstances, can harm your liver:
As mentioned earlier, herbal and dietary supplements contribute to 20% of hepatotoxicity cases in the US.
The research found significant culprits like anabolic steroids, green tea extract, and multi-ingredient nutritional supplements (MINS) as common causes.
Anabolic steroids, often sold as bodybuilding supplements, usually result in a prolonged cholestatic liver injury. A specific pattern in blood tests and liver tissue samples characterizes this type of injury.
On the flip side, green tea extract and similar products are prone to trigger acute liver injury, with symptoms closely mirroring those of hepatitis.
However, the majority of HDS-associated liver injuries are linked to MINS, where the specific toxic component is often unknown.
This poses challenges in diagnosis, treatment, and prevention. Improved regulatory oversight is crucial to ensure the purity and safety of non-prescription products.
Collaboration among healthcare professionals, chemists, and toxicologists is essential to identifying and regulating harmful ingredients and promoting public safety.
Symptoms indicating potential liver function issues can appear in various ways.
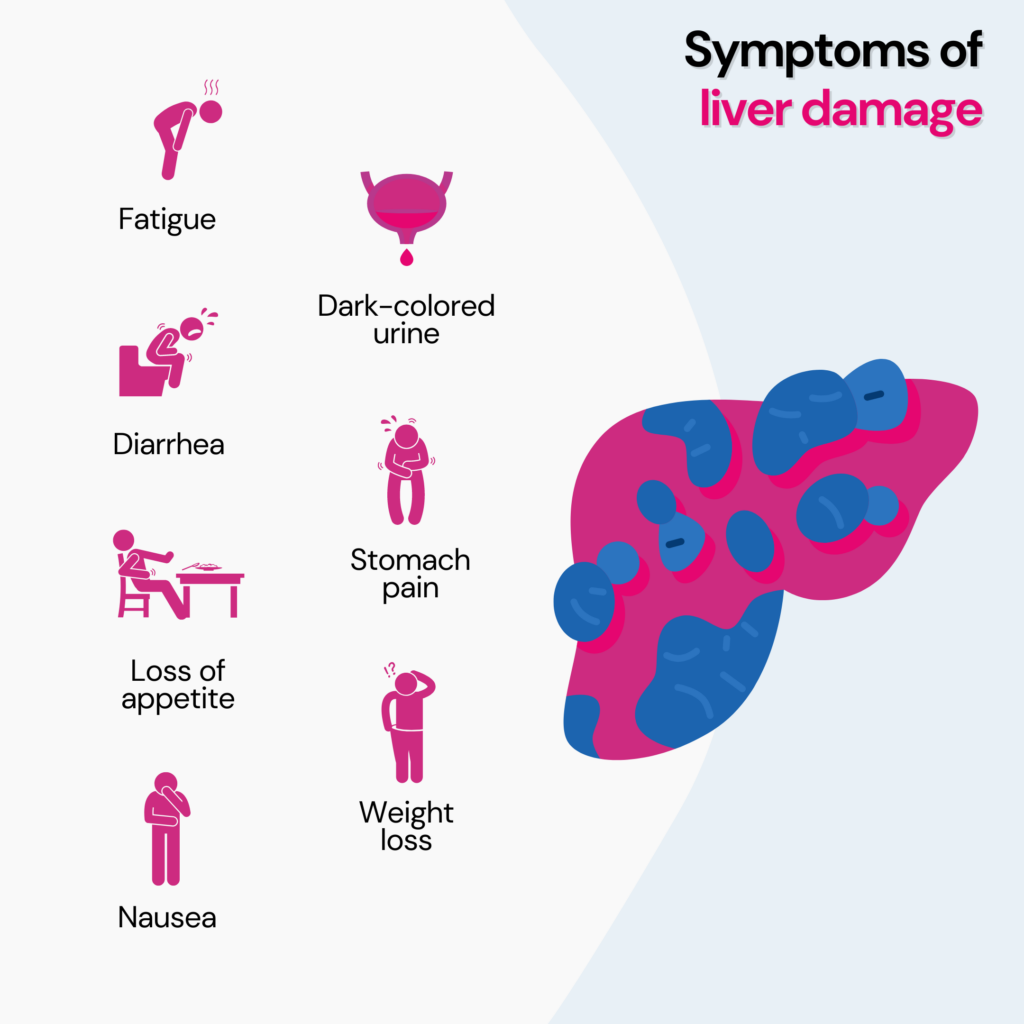
Other symptoms include:
These indications could appear rapidly or gradually, depending on the cause and severity of liver injury.
It is vital to consult a physician promptly if you notice any of these signs so they can evaluate the condition and provide necessary treatment.
Vitamin A and niacin (vitamin B3) are the vitamins that are hard on the liver in high doses.
While most vitamins, when taken within recommended amounts, rarely cause liver harm, vitamin A and niacin can lead to distinctive forms of liver injury.
This risk arises because many vitamins, especially fat-soluble ones, are concentrated, metabolized, and stored in the liver.
Exceeding safe intake levels can overload the liver's capacity to process these vitamins, resulting in liver damage.
Thus, caution should be exercised with vitamin A and niacin supplementation to prevent liver injury.
While some supplements may be effective in supporting liver health, it is important to talk to your doctor about it and only take those that are prescribed.
Be careful with some natural supplements, as they can hurt your liver.
Be cautious with kava, green tea extract, comfrey, chaparral, aloe vera, black cohosh, and echinacea supplements, especially if you have liver issues or take other medications.
Watch for signs like tiredness, yellow skin, or belly pain, which could mean liver damage.
Too much vitamin A and niacin can harm your liver. Before starting any new supplements, consult your doctor first.
Check what's inside them and pick brands that have been properly tested and approved.
Eating healthy foods and living a good lifestyle is best for keeping your liver healthy. Only use supplements when you really need them.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5502701/
https://www.ncbi.nlm.nih.gov/books/NBK548637/
https://www.ncbi.nlm.nih.gov/books/NBK547925/
https://www.ncbi.nlm.nih.gov/books/NBK548370/
https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/larrea
https://www.ncbi.nlm.nih.gov/books/NBK547990/
https://www.ncbi.nlm.nih.gov/books/NBK548440/
https://www.webmd.com/hepatitis/toxic-liver-disease
https://www.ncbi.nlm.nih.gov/books/NBK548888/
https://www.everydayhealth.com/news/toxic-not-healthy-surprising-liver-dangers-herbal-products/
Imagine this: You've been regularly going to the gym, pushing yourself, and attempting to gain lean muscle mass. Along the way, you've heard about the advantages of using creatine supplements, including
Excited to try it out, you dive into the world of creatine, only to be met with concerns about bloating. But does creatine make you bloated?
Let's unravel the truth behind this common question and explore effective strategies to minimize any potential bloating.
Creatine, an amino acid found in our muscles, is a powerful energy generator during high-intensity exercise.
Its primary role is to help regenerate ATP (Adenosine Triphosphate), the body's major energy source, allowing you to perform at your best throughout heavy workouts.
This amino acid is available in various forms:
You can also consume it by taking creatine-rich foods, such as:
Creatine supplementation can improve athletic performance and has several benefits, including:
Now, onto the burning question – does creatine make you bloated?
A phenomenon known as creatine bloating can often occur while adopting creatine supplements, especially during the early loading phase.
Taking a more significant dose of creatine, usually 20–25 grams, to saturate the muscles is required during this period, which lasts for about 5-7 days on average.
Temporary bloating may result at this time due to an increase in creatine intake and increased water consumption.
Thus, it is important to note the bloating felt during the loading period is temporary and usually goes away within a few weeks.
This is not the same as bloating caused by digestive issues or excess gas.
Creatine helps generate energy by increasing the concentration of creatine phosphate in the muscles.
As a result, the muscles hold onto extra water, which helps rise in body weight.
It's important to understand that this water retention is intramuscular, meaning it stays within the muscle cells and not in the spaces between cells or organs.
The water retention associated with creatine usage may make you feel slightly heavier or fuller, but it is not the same as bloating caused by digestive problems.
True bloating often involves discomfort, distention, and excessive gas.
With creatine-related water retention, you may notice a subtle increase in body weight and muscle fullness, but it should not cause significant discomfort.
Creatine bloating is temporary and should stop within a few days to a couple of weeks - this can be avoided by taking a lower dosage.
Did You Know?
Your genes influence important aspects of fitness like your endurance potential, injury risk, premature fatigue, motivation to work out, etc. Unlocking this information using your ancestry test DNA data can help you achieve your fitness goals seamlessly.
Creatine significantly influences people who engage in high-intensity, short-duration activities.
For example, weightlifting, running, and boxing athletes often see a significant performance boost with creatine supplementation.
However, even if you are not a top athlete, creatine can enhance your fitness journey by helping you gain strength, stamina, and total muscle development.
While creatine is usually safe for most people, certain groups should use caution or avoid supplementation.
For example, individuals with kidney disease, high blood pressure, liver disease, or a history of kidney stones shouldn’t use creatine.
If you are breastfeeding or pregnant, it is advisable to avoid creatine.
Making informed decisions about supplements and prioritizing your health is important.
If you experience water retention or perceived bloating from creatine, there are effective strategies to minimize these effects:
Yes, the water retention associated with creatine usage will gradually subside once you stop taking the supplement.
However, it's important to remember that this temporary water weight is unrelated to body fat or actual bloating, and it should not be a cause for long-term concern.
If you discontinue creatine, your body's water balance will normalize.
Aim to consume an additional 8-16 ounces (240-480 ml) of water daily to support the benefits of creatine supplementation and maintain maximum hydration.*
This helps to flush out waste products, support muscle function, and promote overall well-being.
Remember, hydration is key to unlocking your full fitness potential.
If you're concerned about water retention and potential bloating, stick with creatine monohydrate.**
This form of creatine is widely recognized as safe and effective, with numerous scientific studies backing its benefits.
Avoid experimental or lesser-known forms of creatine that lack sufficient evidence or may have undesirable side effects.
By choosing creatine monohydrate from a reputable brand, you can maximize the advantages of creatine while minimizing any temporary water retention.
*overhydration can also lead to digestive issues like nausea or vomiting.
**Please consult a doctor for advice on the best supplement for your body’s needs
Taking creatine can cause temporary muscle hydration that leads to bloating, but it's not permanent. When you stop taking creatine, the bloating will disappear, and your body will return to normal rather than digestive issues or excess gas.
By following a balanced diet, and selecting a reputable creatine monohydrate supplement, you can enjoy the benefits of creatine while minimizing any temporary water weight.
Before beginning creatine supplementation, seek advice from a healthcare professional to ensure it suits your needs and health status, just like any other dietary supplement.