Despite the tremendous growth of the healthcare industry, some diseases like cancer remain elusive and hard to handle. Multiple factors contribute to the development and progression of the condition, gene variations being one of them. Genetic testing now makes it possible to know if a person is at risk for developing certain kinds of cancers. The 23andMe BRCA test can check DNA samples for 44 cancer-causing variants and help at-risk individuals take timely preventive actions. What is 23andMe’s BRCA accuracy rate? How much can these test results be trusted? What are the limitations of the test? Keep reading to know more.
Did You Know
Contrary to popular belief, BRCA1 and BRCA2 genes don’t cause breast cancer. In fact, they have a protective role against cancers! In some cases, BRCA1 and BRCA2 genes have mutations that interfere with their protective role. Though these mutations may not definitely cause breast cancer, they do increase the chance for it to develop. Genetic tests can help find faulty genes and help family members find out whether they are at increased risk. Xcode Life looks for these mutations in your ancestry test DNA data and provides you with a comprehensive Breast Cancer Risk analysis. Learn more
Genetic testing can provide essential information about certain health risks, helping individuals take timely preventive actions.
23andMe is a personal genomics company that sells direct-to-consumer health and ancestry genetic testing kits.
23andMe’s testing kits offer a combination of health predisposition, carrier status, wellness, pharmacogenetic, and ancestry reports, depending on the service chosen.
The BRCA1/BRCA2 (Selected Variants) Genetic Health Risk report is one such test report.
According to 23andMe, this test report may tell if a person has an increased risk of developing certain types of cancers due to BRCA gene variations.
The 23andMe BRCA1/BRCA2 (Selected Variants) Genetic Health Risk report tests human DNA samples for 44 variants of the Breast Cancer 1 (BRCA1) and Breast Cancer 2 (BRCA2) genes.
The test uses human saliva samples for analysis. It may take up to a few weeks for the users to receive their test results digitally.
The BRCA1 and BRCA2 genes help create proteins that are tumor suppressors.
These proteins also repair damaged DNAs and regulate cell division.
According to the Centers for Disease Control and Prevention (CDC), 3% of breast and 10% of ovarian cancers are due to mutations in the BRCA1 and BRCA2 genes.
Mutations in these genes affect both men and women and may also increase their risks of developing uterine, colon, stomach, pancreatic, and testicular cancers.
According to the company’s website, all their health report tests, including the BRCA report, meet the Food and Drug Administration’s (FDA’s) analytical and clinical validity requirements.
What does that mean?
The 23andMe BRCA report is the only FDA-authorized direct-to-consumer test for BRCA variants available in the market.
However, the FDA specifies that the 23andMe BRCA report should not be used for diagnosis and cannot be used to make medical decisions.
What does this mean?
It means that even if the BRCA report is >99% accurate, it cannot say if a person would or wouldn’t develop cancer.
Some people with the risk variants may not develop cancer, while those who don’t have the variants could end up with cancer due to other reasons.
The FDA protects public health by monitoring the efficacy and safety of food, drugs, cosmetics, biological products, and radiation-emitting electronics.
The FDA assesses direct-to-consumer genetic tests for reliability, accuracy, clinical validity, and the truthfulness of their claims.
In 2018, the FDA authorized 23andMe’s initial BRCA genetic test.
This test analyzed and reported three variants of the BRCA1 and BRCA2 genes commonly found in people of Ashkenazi Jewish descent.
In August 2023, 23andMe received the FDA 501(k) clearance to test for 41 more variants in both these genes that may be associated with an increased risk of certain types of cancers.
Does the new FDA clearance mean the 23andMe BRCA accuracy rate has improved drastically?
Since the BRCA test now reports on 44 variants instead of just 3, the chance of the test identifying a person’s risk of developing cancers has improved.
This also means that the BRCA report would now be inclusive of people of different descents instead of just focusing on the Ashkenazi population.
According to the company, this report may have the following ethnic accuracy rate.
Any adult who can provide a saliva sample can take the 23andMe BRCA report.
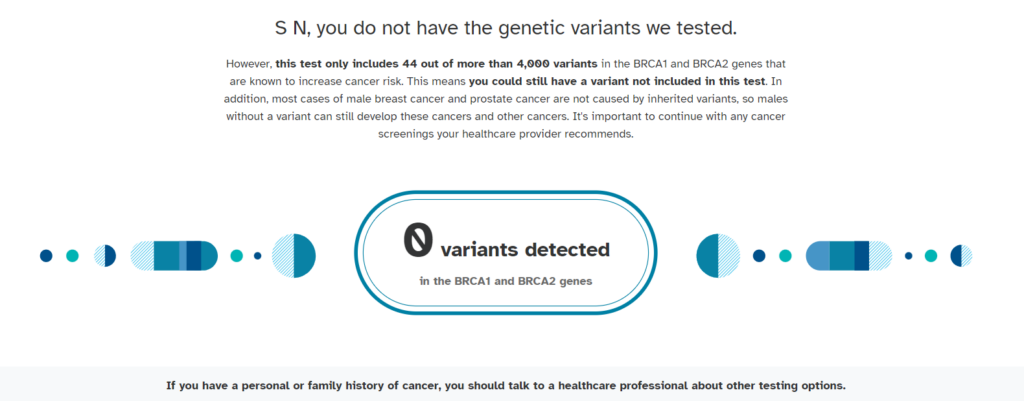
Once you receive the test results, you may find either of the three terms mentioned in the report.
This means none of the 44 variants tested were found in your DNA.
This, however, does not mean you have zero risks of developing cancers.
You may still have other cancer-causing variants not part of the test.
Non-genetic factors may also add to the risk.
If one or more variants were found in your test report, you have a higher risk of developing certain types of cancers.
The next step is to make an appointment with your healthcare provider and discuss the findings.
Your doctor may have strategies to prevent or reduce your risk of developing these conditions.
You can also speak to a genetic counselor to get more value from your test report.
This is especially helpful if the findings make you uncomfortable, fearful, or anxious or if you are worried about the risk status of your relatives.
Sometimes, the counselor may advise your closest family members to get their genes tested to see if they carry the same variant.
Random test errors, contaminated samples, or other external factors can prevent the lab from successfully analyzing your sample.
In this case, the lab may ask for a new sample.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7010426/
https://www.cdc.gov/genomics/disease/breast_ovarian_cancer/genes_hboc.htm
https://www.breastcancer.org/research-news/fda-authorizes-23andme-brca-genetic-test
https://www.fda.gov/medical-devices/in-vitro-diagnostics/direct-consumer-tests
AncestryDNA is the gold standard of genetic ancestry testing, giving you detailed information on your ancestral roots, along with some interesting tools to explore your ancestry. Follow this simple 3-step process to log in to your AncestryDNA account to access all this information.
Did you know that your AncestryDNA raw data contains around 700,000 genetic markers? Ancestry reports only use 0.01% of this information. There is more information about your health, nutrition, fitness, allergy, and specific genes like COMT, MTHFR, and APOE in your raw data. After finding out your ancestry information on the AncestryDNA site, you can download your raw data and use it to find out more about yourself. Learn how.
Or you can directly place a request to download your DNA data.
In case you are unable to access your AncestryDNA account, try the following:
Most AncestryDNA accounts renew automatically at the beginning of each calendar month. Semi-annual and annual memberships renew every six months and year, respectively.
If your account doesn't renew automatically, then:
Your AncestryDNA results cannot be moved from one account to another. However, if you are the account owner, you can invite other people (or your new email) to view the results.
If you would like to share your ethnicity results, visit this page for the instructions.

Comparing The Genetic Ancestry Testing Companies
Are Postbiotics Better Than Probiotics For Gut Health?
Do you love the balayage look and want it on yourself but don’t want to damage your hair by bleaching it? You might have heard that bleaching can damage and weaken your hair strands. So, you take a more natural route: bleach your hair with the sun’s rays. But is everything that is natural good for you? Photobleaching can be harmful to your hair and equally damaging as getting your hair bleached at the salon. Still want to do it? Here is your guide on what exactly photobleaching is, why it is harmful, and some better alternatives.
Did You Know?
The MC1R gene, a critical determinant of hair color, is also associated with aging, the risk for sunspots, and the likelihood of freckles. You can learn in-depth about your skin health and traits using your existing ancestry genetic test DNA data.
Photobleaching is the lightening of hair due to sun exposure.
Over time, the sun can turn your black hair to brown or lighten brown hair to blonde hair.
If you spend time outdoors, you will notice that your hair has darker roots and lighter strands.
It is an effect of photobleaching.
Your hair contains a pigment called melanin in them.
Melanin is responsible for dark hair and skin, which means it colors your hair and skin.
The sun’s UV rays react with the melanin in your hair, turning it colorless.
While this might seem inexpensive to bleach your hair, it can also have harmful side effects.
The sun lightens your hair through a chemical reaction called oxidation.
The same chemical reaction happens when you bleach your hair at a salon.
Oxidation occurs when a substance comes in contact with oxygen.
In this case, the sun’s rays bleach hair by naturally depleting its melanin.
The sun’s rays alter the level of melanin in your hair by depleting this pigment.
Your hair, unlike your skin, is dead tissue.
That is why you can get rid of a tan but cannot make sun-bleached hair return to normal.
You will only return to your natural hair color once your hair grows out and you decide to chop off the bleached part.
Photobleaching is a phenomenon that depletes the melanin present naturally in hair.
The effects of photobleaching will be more noticeable when you already have less melanin in your hair.
It means that people with blonde or lighter hair colors will get more affected due to photobleaching than people with darker hair.
Photobleaching is a result of light-induced hair aging. The hair becomes paler in color, and the softness and shine of the hair can change as well.
The photochemical effects on hair color highly depend on certain color pigments in the body called melanins and chromophores.
The melanin pigment is of two types: pheomelanin and eumelanin
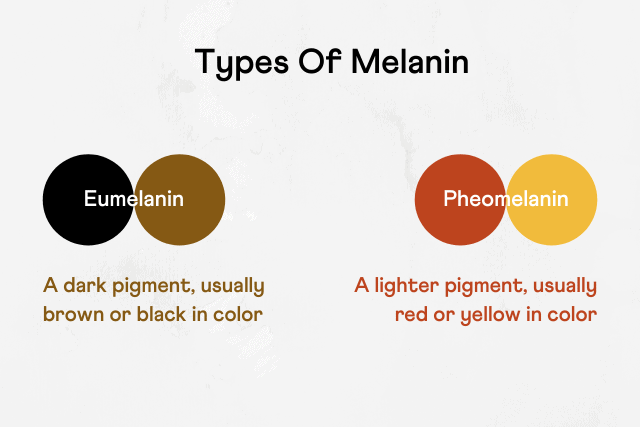
Our hair color is a result of which one of these pigments dominates the other.
Whether a person has more pheomelanin or eumelanin is determined by their genetics.
The dominant type of melanin in red hair is pheomelanin, while blonde hair is a mix of eumelanin and pheomelanin, with the former more present than the latter.
Research suggests that pheomelanin is more sensitive than eumelanin to sun-induced hair lightening. Thus, people with dark-colored hair may experience more photobleaching.
Hundreds of genes affect the amount of melanin in your hair.
Out of this, researchers have identified as many as 48 genetic markers that might affect hair photobleaching.
However, they have not identified any particular gene that specifically influences photobleaching.
Europeans are more affected by photobleaching than any other racial or ethnic groups.
People of non-European descent have lower chances of experiencing photobleaching.
Photobleaching your hair is potentially dangerous, even though it might be effective.
The sun’s UV rays break down keratin, the protein in your hair.
Over time, this will lead to weak and brittle hair.
Sun exposure can also dry up your scalp, leading to further hair damage.
Additionally, you also run the risk of developing skin cancer due to prolonged sun exposure.
Lightening your hair through sun exposure is probably not a good idea.
It can damage your hair and also increase your chances of developing skin cancer.
Here are a few safer alternatives to photobleaching that you can try:
*the alternatives provided are for informational purposes only. Please seek professional assistance before trying any method for hair lightening.
Photobleaching can be highly harmful to your hair.
It can dry out your scalp, weaken your strands, and even increase the risk of getting skin cancer.
Rather than getting sun exposure to lighten your hair, you should take steps to protect it from damage.
Always wear a hat or scarf if you are going out in the sun, and start using hair sunscreens.
Use a moisturizing shampoo and conditioner to prevent your scalp from drying out.
If you want to bleach your hair, visit a professional to get it done rather than exposing yourself to the sun’s rays.
https://www.healthline.com/health/beauty-skincare/sun-bleached-hair
https://www.cancer.org/cancer/risk-prevention/sun-and-uv/uv-radiation.html
https://medlineplus.gov/genetics/understanding/traits/haircolor/
Kiwi proudly boasts its “superfood” title for all the right reasons. In this nutrient-dense fruit, one particularly stands out - vitamin C. A recent study has revealed that consuming just 2 gold kiwis is as good as vitamin C supplements in preventing vitamin C deficiency. Let’s learn more about what this study says and other benefits of consuming kiwi every day.
Did You Know?
Animals like cats and dogs can synthesize vitamin C on their own, whereas, some birds, fish, and humans cannot. Though humans have the gene needed for vitamin C production, it has been inactivated through evolution. So, vitamin C needs to be supplemented through diet. Your genes can also influence how effectively vitamin C is absorbed from your diet and used by the body. SLC23A1 and SLC23A2 are two genes involved in this process. Mutations in these genes, influence the absorption of vitamin C by the body. You can learn in-depth about your nutritional requirements using your existing ancestry genetic test DNA data.
Vitamin C, or ascorbic acid, is a water-soluble vitamin required for the normal growth and development of the body.
Here are some functions of vitamin C in the body:
An important property of vitamin C is that it is one of the most powerful antioxidants.
Antioxidants are molecules that prevent free radical damage.
This free radical damage is responsible for aging and plays a role in cancer and the development of other chronic diseases.
Free radicals are formed due to many reasons, 2 common ones being:
Since the body cannot make or store vitamin C, consuming lots of vitamin C-containing foods in your daily diet is essential.
The recommended dietary allowance (RDA) of vitamin C is 90 mg/day for adult males and 75 mg/day for adult females.
Several fruits and vegetables are excellent sources of vitamin C. Some of these include:
Studies have shown that people who consume vitamin C supplements have stronger immunity.
One study states that consuming two kiwi fruits daily as part of the diet was as good as taking vitamin C supplements.
A study published in Foods stated that consuming two SunGold kiwis daily for six weeks increased vitamin C intake by 150 mg per day.
Researchers found that consuming this level of vitamin C eliminates the need for supplementation.
The 24 participants in the study were between 25 and 60 years of age and had no history of type 1 or type 2 diabetes or impaired glucose tolerance.
The study was designed to understand the effects of daily kiwi fruit consumption.
In this 6-week study, one set of participants was required to consume two Actinidia chinensis var. (marketed as Zespri SunGold Kiwifruit) per day. The remaining participants acted as a control.
Urine and venous blood samples and the participants' body weight were monitored before, during, and at the end of the study.
Though a small-scale study, the results were promising. The following observations were noted in the study:
Regular green kiwis contain 92.7 mg of vitamin C.
Every 100 g of Zespri kiwi contains 161.3 g of vitamin C, meaning having two of them gives you more than twice the RDA of the vitamin.
Consuming two SunGold kiwis gives you more vitamin C content than the RDA.
So, you can safely consume two kiwis in a day.
Eating kiwis offers several health benefits:
What if you have the power to change the way your gene functions, by hacking into your genetic code to make your genes behave favorably? Though it may sound something far-fetched, the field of epigenetics makes it possible for us to overcome some of our "genetic disadvantages" by making certain lifestyle changes.
Epigenetics is the study of how your behaviors and environment can cause changes that affect the way your genes work. Unlike genetic changes, epigenetic changes do not alter the DNA sequence but can still impact how your body reads a DNA sequence. Imagine your DNA as a recipe book. Epigenetics can't change the recipes, but it can decide which recipes are used and how. It's like having sticky notes in your recipe book that say "use this recipe more" or "don't use this one." Epigenetic changes act as a set of switches that turn genes on or off, determining which genes are active and which are dormant.
The debate between genetics (nature) and environment (nurture) takes a fascinating turn with epigenetics. It suggests that while you can't change your genetic code, your environment and behaviors, like diet, stress management, and exposure to toxins, can influence how those genes are expressed. For instance, someone genetically predisposed to diabetes may never develop the disease with the right lifestyle choices, thanks to epigenetic modifications.
Absolutely, converting the "How Can Your Epigenetics Change?" section into a listicle format can make the information more digestible and engaging. Here's the revised section:
Your lifestyle choices can lead to epigenetic changes in various ways. Here's a list of key factors that can influence your epigenetics:
Each of these factors plays a significant role in how your epigenetics can change, underlining the importance of healthy habits in influencing gene expression. By making conscious lifestyle choices, you can have a positive impact on your epigenetic profile.
Epigenetics is crucial in understanding how certain conditions develop. For instance, certain epigenetic changes are linked to the development of diseases like cancer, diabetes, and heart disease. The good news is that some epigenetic changes are reversible, offering potential pathways for novel treatments and preventive measures.
Epigenetic changes can sometimes be passed down through generations. This means the healthy habits you adopt today might not only benefit you but could also positively influence the health of your future children and grandchildren, offering a legacy of health influenced by your life choices.
That wraps up our quick dive into the world of epigenetics! Join us next time as we continue to explore the incredible landscape of genetics in our "2-Minute DNA Digest." Remember, your genes are just the beginning of the story – how you live your life can narrate the rest!
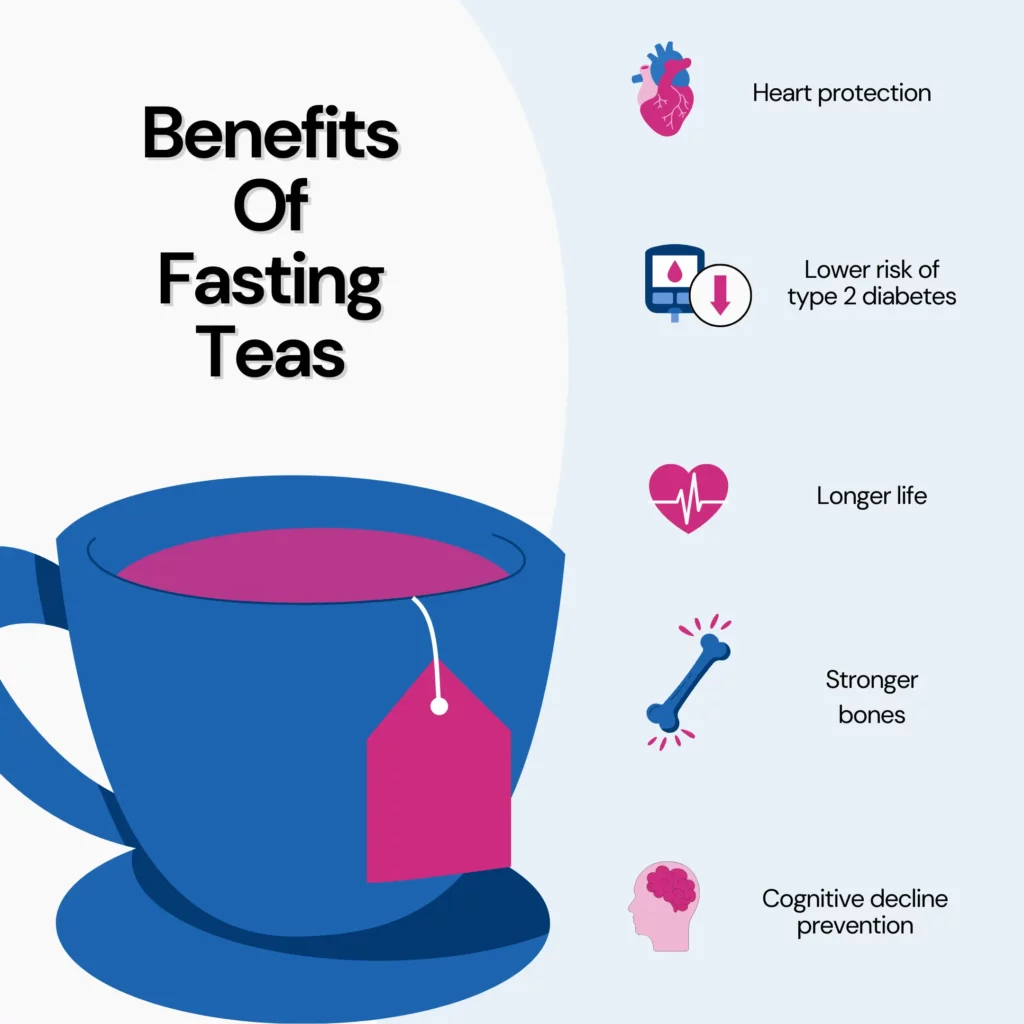
Fasting is an old practice with several health advantages, but it can also be challenging, especially for beginners. That's why some people drink fasting teas to support them during their fasting periods. Fasting teas are herbal preparations that help the body and mind during a fast. They can help with hunger, hydration, digestion, detoxification, and mood enhancement. However, not all fasting teas are made equal. Some may contain substances that are not suitable for fasting or may reduce the benefits of fasting. Keep reading to explore everything you need to know about fasting teas: what they are, what they do, how to pick them, and how to use them.
Did You Know?
Some researchers argue that not meal timings but meal quantity influences our body weight. According to a study, the times at which we eat don’t have any effect on the body.
Intermittent fasting (IF) flips the switch on your eating routine, cycling between feasting and fasting periods.
It does not prescribe specific foods to consume but rather the timing of consumption.
There are different methods of intermittent fasting, each with different durations and frequencies of fasting and eating, such as:
Intermittent fasting can bring various health benefits, such as promoting weight loss, enhancing insulin sensitivity, reducing inflammation, and lowering cholesterol levels.
It may also help lower the risk of specific diseases, such as type 2 diabetes, heart disease, and cancer.
Fasting teas are herbal blends crafted from plants with properties that help the body and mind during fasting.
They differ from regular teas containing caffeine and other compounds that can disrupt fasting by stimulating metabolism.
They are caffeine-free, unsweetened, and calorie-free and do not interfere with the fasting state.
Fasting teas can produce various effects based on their ingredients. Some anticipated impacts include:
Many types of fasting teas are available on the market and can vary in their ingredients, quality, and effectiveness.
Some of the most popular types are:
Fasting tea: It may contain a blend of different herbs that have various effects on the body and mind during fasting.
Some examples of brands that sell fasting tea are:*
Detox tea: This type of fasting tea may contain herbs that support the liver and kidneys in cleansing the body from toxins and waste products.
Some examples of brands that sell detox tea are:*
Slimming tea: This fasting tea may include herbs that suppress appetite, boost metabolism, and burn fat.
Some brands that sell slimming tea are:*
*Xcode Life neither endorses any of these brands nor is afflicted with them. They are listed here for informational purposes only.
Drinking tea has several health benefits, whether you are practicing intermittent fasting or not. Here's a look at what research says about the health benefits of tea:
While fasting teas are usually harmless, it is important to be aware of potential risks and side effects.
Potential side effects of fasting teas:
Potential risks of fasting teas:
With so many types and brands of fasting teas available, how do you choose the best one?
Here are some tips to help you:
Essential reminders to consider:
The ideal fasting tea for you depends on your personal preferences and needs. Some popular options are:
Hand-picked Content For You: Combating The Yo-Yo Effect: Avoiding Weight Regain After A Diet
Fasting teas, often marketed as "fasting teas" or "detox teas," claim to enhance the effects of fasting.
However, the direct impact of fasting teas on boosting the effectiveness of fasting is a complex question that needs comprehensive scientific evidence.
While certain teas, such as green tea, contain herbs with potential health benefits, the scientific support for their significant role in enhancing fasting effects remains conclusive.
It is essential to consider fasting teas complementary rather than standalone solutions within a dietary plan, seeking personalized advice from healthcare providers.
Fasting teas, marketed as supportive beverages during fasting, are herbal blends designed to help the body and mind.
They offer potential benefits such as appetite suppression, hydration, digestion support, detoxification, and mood enhancement.
Only limited scientific evidence supports the direct impact of fasting teas on boosting fasting effects.
These teas, often caffeine-free and calorie-free, can be part of a well-rounded fasting plan.
However, caution is advised, as some may have side effects like nausea or heartburn, and interactions with medications should be considered.
It is advisable to consult with a doctor and gradually incorporate fasting tea into one's routine based on personal goals and preferences.
The effectiveness of fasting teas varies among individuals, making it crucial to listen to your body and adopt a balanced approach to fasting and overall well-being.
https://www.medicalnewstoday.com/articles/323605
https://www.healthline.com/nutrition/eat-stop-eat-review
https://pubmed.ncbi.nlm.nih.gov/32662279/
https://www.everydayhealth.com/diet-nutrition/fasting-teas/guide/
https://www.healthline.com/nutrition/10-natural-appetite-suppressants
https://www.healthline.com/nutrition/tea-for-digestion
https://www.healthline.com/nutrition/herbs-for-liver
https://www.healthline.com/health/mental-health/tea-for-stress
https://journals.sagepub.com/doi/abs/10.1177/2047487319894685
https://www.acpjournals.org/doi/abs/10.7326/M22-0041
https://ajcn.nutrition.org/article/S0002-9165(22)00319-7/
https://link.springer.com/article/10.1007/s12603-016-0687-0
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/211409
https://www.webmd.com/vitamins/ai/ingredientmono-960/green-tea
https://www.mayoclinic.org/diseases-conditions/constipation/in-depth/laxatives/art-20045906