Did you know that gluten sensitivity affects about 6% of the U.S. population, making it more common than celiac disease, which only impacts roughly 1%? Many people experience bloating, fatigue, or digestive discomfort after eating gluten, but not all of them have celiac disease or a wheat allergy. Could gluten sensitivity be in your genes, or are other factors influencing your reaction to gluten? How can you tell if you're at risk? Read on to explore the complexities of gluten sensitivity and uncover what science reveals about the role of genetics and beyond.
Gluten sensitivity, also termed non-celiac gluten sensitivity (NCGS), is a condition where individuals react negatively to gluten, a protein in barley, wheat, rye, and other grains.
While commonly associated with foods like bread, pasta, and beer, gluten is also found in some non-food items like cosmetics and medications.
It’s important to understand that NCGS differs from celiac disease, which is an autoimmune disorder influenced by gluten consumption.
Unlike celiac disease, NCGS does not cause damage to the intestines and is also distinct from a wheat allergy.
People with gluten sensitivity often experience bloating, gas, fatigue, and nausea.
Genetics plays a pivotal role in gluten sensitivity, with the condition often running in families and appearing in siblings or cousins.
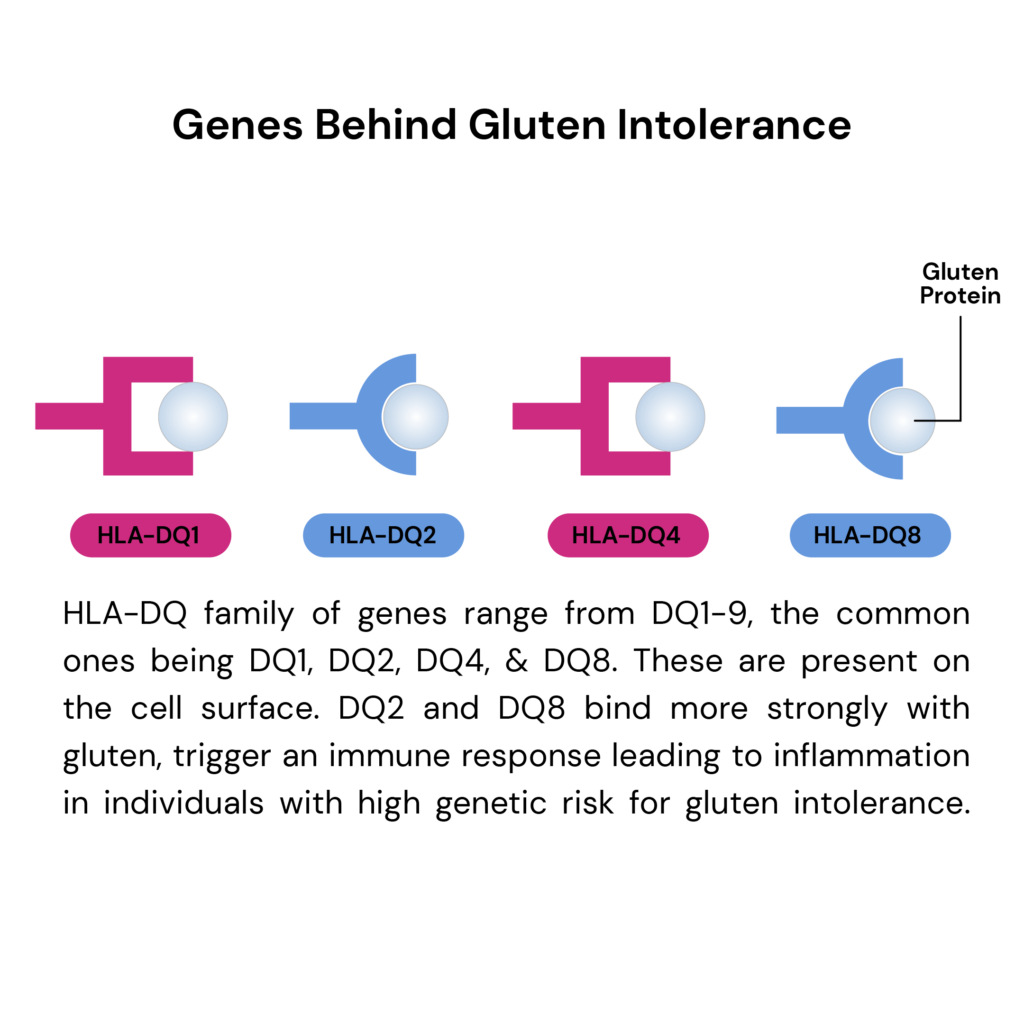
The genetic basis lies primarily in variations of the HLA-DQ gene (HLA stands for human leukocyte antigen), which individuals inherit from both parents.
Specific combinations of HLA-DQ genes, particularly HLA-DQ2 and HLA-DQ8, significantly increase the risk of developing gluten sensitivity.
Gluten exposure in sensitive individuals can cause a wide range of effects. These can be as mild as slight stomach discomfort or as serious as damage to the intestines.
When the intestines are damaged, the body may have trouble absorbing essential nutrients from food. This can lead to various health problems over time.
The severity of the condition depends on both genetic factors and gluten intake.
Dietary management is crucial for those with pronounced gluten sensitivity, especially celiac disease.
Eliminating gluten from the diet is often the most effective approach to prevent symptoms and avoid long-term health complications.
Gluten sensitivity is linked to certain genetic markers, though the connection is less clear than with celiac disease.
Research by Dr. Alessio Fasano from the University of Maryland found that only 56% of those with gluten sensitivity carry the HLA-DQ2 or HLA-DQ8 genes.
These genes are strongly associated with celiac disease, suggesting that while they may play a role, they are not the primary cause of gluten sensitivity.
Another study by Dr. Kenneth Fine, developer of EnteroLab testing, suggests genes like HLA-DQ1 and HLA-DQ3 might also contribute to gluten sensitivity.
He believes that only a small fraction of the population lacks the genetic potential for gluten sensitivity.
However, further research has yet to accept or validate these findings widely.
Yes, there is a gluten sensitivity gene with certain variants that are more influential:
Gluten gene mutations like HLA-DQ2 or HLA-DQ8 increase the risk of developing gluten sensitivity, but their presence doesn't definitively predict the condition.
While strongly associated with the condition, not everyone with these mutations experiences symptoms.
Gluten sensitivity can also occur in individuals without these specific genetic markers, indicating that other factors contribute to its development.
Not everyone carries the HLA-DQ8 gene.
According to studies, approximately 30%-40% of the general population has either the HLA-DQ2 or HLA-DQ8 genes without developing celiac disease.
Among those with celiac disease, about 95% express the HLA-DQ2 gene, while the remaining 5% typically have the HLA-DQ8 gene variant.
If you have done an ancestry genetic test with companies like 23andMe, AncestryDNA, MyHeritage, etc., you can download your raw DNA data, order the Gene Nutrition test, and upload your file for analysis.
While genetics play a significant role in gluten sensitivity, other factors can also affect its development and severity. These include:
It's important to note that while these factors can contribute to gluten sensitivity, ongoing research is working to understand their specific roles better.
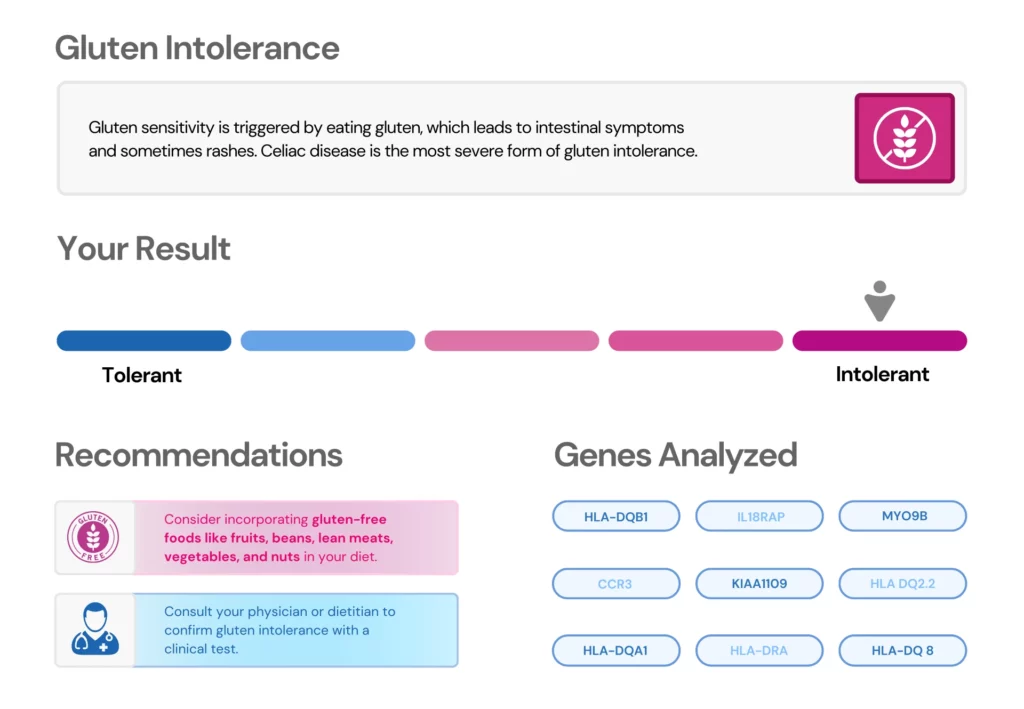
At present, no diagnostic procedure exists specifically for gluten sensitivity. The gluten intolerance gene test is more precisely a genetic risk assessment for celiac disease.
This test examines DNA for specific gene variants, especially in the HLA-DQ complex, associated with an increased risk of developing gluten intolerance.
Individuals suspecting gluten intolerance can use the test to evaluate their genetic risk before changing their diet or seeking medical advice.
Being positive for DQ8 means carrying the HLA-DQ8 gene, which is part of the HLA gene complex.
This gene variant is linked to a higher risk of gluten sensitivity and celiac disease.
While having the DQ8 gene does not guarantee that you will develop these conditions, it does indicate a higher genetic predisposition.
The presence of DQ8 suggests that your immune system might react adversely to gluten, potentially leading to intestinal damage if celiac disease develops.
Testing positive for DQ8 can help in diagnosing celiac disease, especially when combined with other medical tests and symptoms.

Gluten-Free Good For You? Analyze Your DNA Raw Data Now!

How Genes Influence Your Risk For Lactose Intolerance
https://my.clevelandclinic.org/health/diseases/21622-gluten-intolerance
https://celiac.org/about-celiac-disease/what-is-celiac-disease
https://www.mayoclinic.org/diseases-conditions/wheat-allergy/symptoms-causes/syc-20378897
https://pubmed.ncbi.nlm.nih.gov/11892082
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3641836
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6502200
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10096482
https://my.clevelandclinic.org/health/diseases/21622-gluten-intolerance
https://www.verywellhealth.com/gluten-sensitivity-genes-562967
https://www.verywellhealth.com/hla-dq8-one-of-the-main-celiac-disease-genes-562571
Ancestry DNA testing is a booming industry at the moment, with millions around the globe learning more and more about their genetic heritage and ancestry each day. Ancestry tests can connect you with relatives you never knew about and unveil the rich history of your ancestors. Just how far back do ancestry DNA tests go, though? The answer to this question varies depending on the kind of ancestry test you opt for. This article will explore ancestry DNA tests- how they work and what you can (and cannot) learn from them.
Your genes comprise only 3% of your DNA but contain a world of information about you, your relatives, and your ancestors.
Due to different inheritance patterns, you and your sibling may inherit different genes from your parents, giving both of you slightly different ancestry results.
With over 26 million people adding their DNA to the four leading commercial ancestry databases, many people naturally have questions about these tests.
Genetic ancestry tests or genetic genealogy tests allow people to learn more about their ancestors, sometimes going beyond what relatives have told them.
Examining an individual’s DNA variations can provide clues to who their ancestors may have been.
It also helps determine relationships between families.
The genetic patterns and variations are shared between people of particular backgrounds.
Closely related individuals share more genetic patterns and variations.
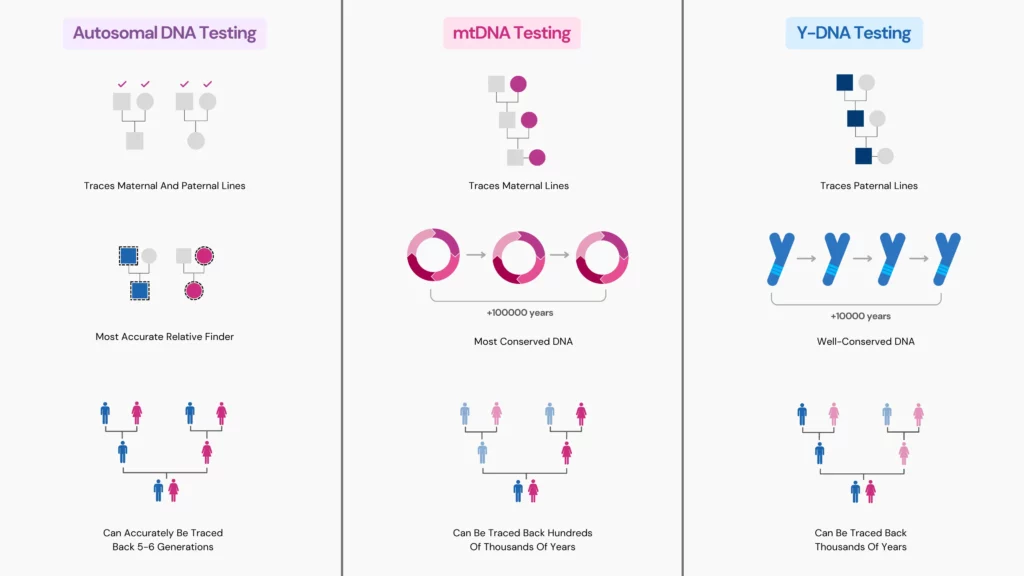
There are three main types of DNA tests:
How far back ancestry DNA tests go depends upon:
Most people can learn about their maternal and paternal ancestry as far back as six to ten generations.
Mitochondrial or mtDNA is a type of DNA testing that takes you back the farthest.
This is because mtDNA mutates slower than Y-DNA over generations.
Thus, it’s exceptionally well-conserved.
Additionally, since we have mtDNA in almost all our cells, studying these DNA samples is more reliable than studying ancient ones.
Y-DNA testing follows your paternal lineage.
Since this kind of DNA occurs on the Y chromosome, only biological males can learn about their heritage through this test.
Additionally, you cannot learn anything about your maternal lineage through a Y-DNA test.
Y-DNA is well-conserved across generations and can be traced back thousands of years.
mtDNA testing can trace your maternal ancestry back 150,000 to 200,000 years.
The mitochondrial Eve lived hundreds of thousands of years ago and is the most recent common ancestor.
Her direct descendant is alive today and carries a fragment of her mtDNA.
Certain mtDNA types can help you trace direct-line maternal ancestry nearly 52 generations or 1300 years prior.
Even though mtDNA testing takes us back into your family history, we can only learn about 1% of our ancestors using this method.
Several companies offer autosomal DNA testing, including:
This type of DNA test provides information about a wide range of ancestors, going back up to five or six generations.
Traveling back one generation halves your DNA.
Your parents carry 50% of your DNA
Your grandparents carried 25% of your DNA, their parents carried 12.5%, and so on.
After a point, the percentage of your DNA becomes too small to track reliably.
Thus, autosomal DNA tests only help trace recent ancestry.
Here’s how you can get the most out of your DNA raw data in 3 simple steps:
The amount of your autosomal DNA halves with each generation.
Thus, after around 8 generations, you are related to fewer and fewer ancestors on your family tree.
The Lurie family is known as the oldest family in the world.
Their lineage can be traced back to the 11th century BCE.
No human can be classified definitively under only one ethnicity.
Migration is inevitable, leading to the mixing of DNA from different ethnicities.

How Long Does 23andMe Take?

Do Ancestry DNA Kits Expire?

Jewish DNA Test: Can Genetic Tests Help Identify Jewish Ancestry?
Ancestry tests are all the rage these days. With a few clicks of a button and a sample of your DNA, you can find out all sorts of things about your family history. But what does it mean if you get 23andMe Native American results? For many, the results can be both exciting and daunting. The test aims to provide individuals with an understanding of their ethnicity and ancestral heritage, but it can also raise questions about what the results mean for them. To help those who have taken the test gain clarity on the results, this article will provide an overview of 23andMe's Native American-specific testing, what data points it covers, and how to interpret your own results.
23andMe analyzes your genes and provides information on the percentage of DNA that you have from different worldwide populations.
The ancestry composition is calculated by comparing your DNA with more than 14,000 people’s ancestries.
If a portion of your DNA resembles that of 1 of the 46 populations, that particular ancestry is assigned to the corresponding portion.
In a similar way, different ancestries are added to different portions of your DNA.
They are then computed together to calculate the overall ancestry composition.
23andMe’s ancestry service includes features that can identify genes associated with Native American ancestry.
These results, however, aren’t confirmatory in nature.
Several million people have availed 23andMe’s ancestry services, and many have discovered at least a small percentage of Native American ancestry in their results.
Whether or not your results indicate Native American ancestry, it is important to understand what it means.
The 23andMe Indigenous American population includes the following genetic groups:
In the above example, the Native American ancestry is pretty high.
This means that certain sections of their DNA match a set of Indigenous American reference individuals more closely than other global reference populations.
Furthermore, people who have indigenous ancestry in North and South America have a common shared ancestry with the people of East Asia.
This is because many thousand years ago, populations migrated from Central to Southern Asia.
Descendants of these populations began to move north to populate the rest of the eastern regions of Asia and Siberia.
The test results should be taken with a pinch of salt, owing to the limitations of this technology.
This can happen when you inherit certain genetic markers that are not yet included in 23andMe’s Native American population reference database.
Further, certain communities of Native American ancestry are underrepresented in genetic research.
Some common physical genetic traits associated with native American ancestry include:
Got your 23andMe test done? Now, you can upload your raw DNA data to Xcode Life to learn 1000+ things about your health, including nutrition, fitness, methylation, and health risks.
Along with the ancestry composition report, 23andMe provides various tools to dig deep into your ancestry.
Map view
Gives a quick and easy overview of your ancestry composition by highlighting the regions in the map associated with your ancestry.
Ancestry details and recent ancestor locations
Provides a microscopic view of your ancestry by narrowing down your results to city and state levels.
This section also comes with cultural, language, and other information about the reference populations.
You can also see a more recent and granular view of your ancestry in this section.
Ancestry timeline
Helps you find out how many generations ago you had a single ancestor from just one population.
Parental inheritance
Applicable only if you match with a biological parent who is also a 23andMe user.
Ancestry composition will display which portion of your ancestry was inherited from which parent.
However, this is not available for everyone.
Chromosome painting
Overview of all 23 pairs of chromosomes, highlighting where your different ancestries are located on your genome.
With the information present in your DNA data, you can uncover insights into several aspects of your health and well-being.
To get your 23andMe raw data, follow the instructions from this page:
How to download your 23andMe Raw Data for 1000+ Health Reports
Yes, 23andMe's ancestry test analyzes markers associated with Native American ancestry.
While DNA tests can identify markers associated with certain ancestral populations, they may not be able to zero down on the exact tribe or clan.
Your ancestry test results may not be consistent with your cultural identity.
While you can celebrate the “Native American” ancestry results, claiming your identity solely based on these results is not advised.
How To Login To Your 23andMe Account – 2024 Updated

How Long Does 23andMe Take?
AncestryDNA vs 23andMe: Which Is Better For Raw Data Analysis?
In the field of DNA analysis, Xcode Life stands out as a reputable, reliable, and regularly recommended choice. Xcode Life analyzes data ranging from a few genes to whole genomes to generate health-related reports on various topics, including nutrition, fitness, skin, and allergies. They accept data from various platforms, including Illumina, Affymetrix, Sequenom, etc. Here are 5 things you should know before you buy Xcode Life's products.
You can use your DNA raw data from several service providers to sign up for Xcode Life.
Some of these include:
Xcode Life offers 11 health-related reports that cover over 700 categories.
Xcode Life offers 11 health-related reports that cover over 700 categories.
| Report Name | Number of Traits Analyzed | Examples |
| Allergy and Drug Sensitivities | 40+ | Pet Allergy Gluten Sensitivity Pollen Allergy Contact Dermatitis |
| Gene Skin | 20+ | Acne Premature Wrinkling Tanning Response Stretch Marks |
| Gene Health | 45+ | Alzheimer’s Type 2 Diabetes Hypertension Heart Diseases Depression Autoimmune Diseases |
| Gene Nutrition | 45+ | Vitamin Deficiencies Tendency to Lose Weight on Protein Intake Lactose Intolerance Alcohol Metabolism Tendency to Prefer Bitter/Fatty/Sweet Foods |
| Gene Fitness | 25+ | Endurance Pain Tolerance Hand Grip Strength Exercise Recovery |
| Traits & Personality | 25+ | Musical Ability Leadership Potential Creativity Warrior Personality. |
| Methylation & MTHFR | 65+ | MTHFR MTRR MTHFD1 CLCN6 NOX4 |
| Gene Sleep | 10+ | Sleep Duration Narcolepsy Frequent Daytime Napping Snoring Tendency |
| BRCA & Breast Cancer | 15+ | Breast Cancer Risk in Men Hormone Receptor and Breast Cancer Breast Size and Breast Cancer Alcohol Consumption and Breast Cancer Risk |
| Personalized Medicine | 500+ | Response to drugs like: Antidepressants Morphine Aspirin Warfarin |
| Caffeine Report | 10+ | Caffeine sensitivity Caffeine metabolism Caffeine overconsumption Caffeine-induced insomnia |
Xcode Life’s individual reports are priced between $20 and $50.
They also offer the following money-saving bundles:
| Health Pack | Wellness Pack | Genome Pack | |
| Number of Reports | 4 | 6 | 9 |
| Reports Included: | Gene HealthGene AllergyBRCA and Breast CancerPersonalized Medicine | Gene NutritionGene FitnessGene SkinGene SleepTraits and PersonalityMTHFR and Methylation | Gene NutritionGene FitnessGene SkinGene SleepTraits and PersonalityMTHFR and MethylationBRCA and Breast CancerPersonalized Medicine |
| Price: | $ | $ | $ |
Users appreciate the variety of traits in the reports and the speed at which reports are delivered.
The nutrition and MTHFR reports are the most popular.
Several users are pleased with the results of their personality trait reports.
Xcode Life has hundreds of testimonials and reviews online. Check them out below:
Check out more testimonials here.
Xcode Life has a customer-friendly privacy policy.
You can delete your raw data and entire account anytime without needing prior permission or approval from Xcode Life.
Review their detailed privacy policy here.
Upload your DNA raw data to Xcode Life to receive 700+ health-related traits.
5 Ways Xcode Life Protects Your DNA Data
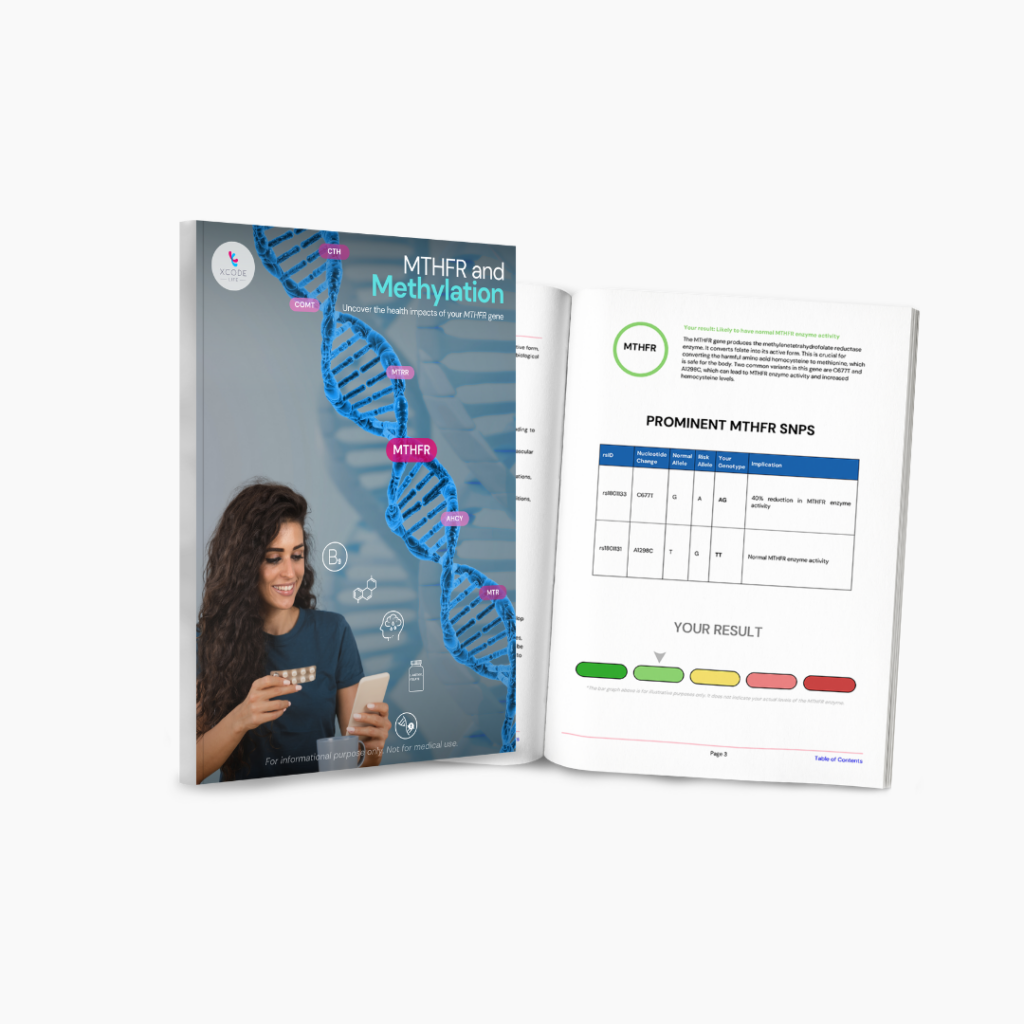
Xcode Life’s MTHFR Methylation Updated Genetic Report: A Walkthrough
Spots appearing on your skin from sun exposure could cause concern. However, freckles are entirely harmless. For many generations, they have been a source of admiration, envy, and curiosity. But how do freckles form? Why do some people have freckles on their faces and others do not? Are freckles genetic? Scientists have discovered that along with sun exposure, your genes may also play a role in developing freckles.
Freckles are small brownish dot-like structures seen on sun-exposed areas (mainly the face).
The primary causes of freckles are genetics and sun exposure.
During sun exposure, skin cells called melanocytes produce a pigment called melanin.
Melanin pigments your hair, eyes, and skin.
If the melanocytes produce melanin evenly, you get a tan in the sun.
However, some people produce more pigment in some areas than others, which can cause them to develop freckles.
Freckles are also more common in European populations due to their lighter skin.
There are two main types of freckles.
| Ephelides | Solar lentigines |
| Smaller in size (1-2mm) | Larger in size (up to a few cm) |
| Usually red or brown | Red, yellow, brown or black |
| More frequent in lighter-skinned people | More frequent in darker-skinned people |
| Common in children and teenagers | Common in people above 40 years of age |
| Caused by genetic factors | Caused by environmental factors |
Certain genetic factors regulate the function of melanocytes, which play an essential role in skin pigmentation.
Changes in these genes can increase a person's risk for freckles, sun spots, and tanning.
For example, a gene called MC1R produces the receptor for the melanocyte-stimulating hormone, one of the two hormones that regulate pigmentation.
Certain changes in MC1R reduce the production of pheomelanin (the lighter pigment), resulting in the overproduction of eumelanin (the darker pigment) in certain areas, leading to freckles.
The freckling trait is passed down from generation to generation in a complex manner.
Several genes interact with each other in this process.
Generally, the MC1R gene has a dominant inheritance pattern for freckles.
If your parents are prone to freckles, you probably will be too.
However, some people may carry the genetic marker for freckles and still never develop freckles.
Since sun exposure is the immediate cause of freckling; you could develop freckles even if your parents didn’t pass down the gene.
The MC1R gene also influences the chances of someone having red hair.
Some people produce eumelanin much less frequently than pheomelanin.
This results in light-colored hair.
It also explains why several red-haired people have freckles.
Freckles aren’t a cause for concern since they fade away with time.
However, since people who are prone to freckles have more sensitive skin, it’s best to be cautious when in the sun.
Long-term sun exposure can cause sunburns, wrinkling, and even some types of skin cancer.
The American Academy of Dermatology has issued the following recommendations to avoid sun damage and freckle formation.
Curious about your freckle genes? Here’s how you can learn about it in 3 simple steps:

Is Sleep Apnea Genetic? Risk Factors, Treatment, And More

Is Handedness Genetic? What Science Tells Us

National Wellness Month | 5 Life-changing Wellness Tips
https://my.clevelandclinic.org/health/articles/23091-freckles
https://www.medicalnewstoday.com/articles/323471
https://www.ancestry.com/c/traits-learning-hub/freckles
https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-all-about-freckles
https://www.hopkinsmedicine.org/health/wellness-and-prevention/sun-safety
Tattoos, once considered a form of self-expression, are now raising concern for potential health risks. According to the Pew Research Center, 32% of Americans have a tattoo, and 22% have more than one. Yet, the safety of tattoo inks remains unexplored, and the potentially harmful effects of injecting them into the body remain unknown. A new study reveals that getting tattoos might increase the chances of cancer like malignant lymphoma. This article discusses the methodology, results, and limitations of the research to provide a clearer understanding of how tattoo inks might contribute to health risks like lymphoma.
A study conducted in Sweden suggests that getting a tattoo might increase the chances of getting malignant lymphoma by 21%.
Malignant lymphoma is a type of blood cancer that affects the lymph nodes.
The research was published in May in the journal eClinicalMedicine.
The study, conducted by researchers at the University of Lund, Sweden, correlates tattoos with malignant lymphoma and does not suggest that tattoos cause lymphoma.
They used the Swedish National Cancer Register to identify people diagnosed with malignant lymphoma.
The researchers then sent them questionnaires, asking them how many of them had tattoos.
About 20% of people responded that they had tattoos before their diagnoses, which led to the study's conclusion.
The study included around 12,000 people.
The researchers identified every person between 20 and 60 who had malignant lymphoma during the ten years from 2007 to 2017.
The researchers also found three randomly selected control groups with matching ages and sexes using the Total Population Register.
Nevertheless, getting a tattoo might increase the risk of developing lymphoma.
Tattoo ink contains various carcinogenic compounds and metals such as nickel, chromium, cobalt, and arsenic.
They can get deposited in lymph nodes when you get a tattoo.
Further, many tattoo artists and parlors don't practice good quality control and hygiene.
Thus, it's important to evaluate the risks before getting that tattoo you have wanted for a long time.
Some studies have attempted to understand if tattoos increase the risk of cancer.
However, these studies could not establish a link between tattoos and lymphoma.
Some risk factors for lymphoma are:
Experts say that while there is no evidence to prove that tattoos cause lymphoma, it is still essential to be cautious.
Tattoo ink contains some carcinogens, and unsterilized needles can cause diseases other than cancer.
Usually, getting a tattoo from certified studios and tattooists is relatively safe.
However, tattoos do have the risk of some complications, such as:
While this study has attempted to correlate tattoos with cancer, we still need more research to understand the risks thoroughly.
Getting a tattoo will probably not give you lymphoma.
However, it can still give you other diseases if you do it from unhygienic parlors and untrained tattooists.
Before getting a tattoo, consider the possible risks and ensure you get it from a trustworthy place.

Alcohol Does Raise Blood Pressure, Even With 1 Drink: Study Finds

Excess Use Of Smartphones Affects Male Fertility: Study Finds
https://www.sciencedirect.com/science/article/pii/S2589537024002281
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(24)00228-1/fulltext#%20