Wellness isn't just a buzzword; it's an ongoing journey that many of us are trying to navigate. We've all had those moments where we promise ourselves to start eating healthier, exercise more, or finally get enough sleep, only to find that life gets in the way. The truth is, wellness isn’t a one-size-fits-all approach; it’s about understanding what your body and mind truly need. This National Wellness Month, instead of being overwhelmed by all the advice out there, let’s focus on five simple yet life-changing wellness tips that you can easily integrate into your daily routine. Whether you're looking to improve your physical health, mental clarity, or emotional balance, these tips are designed to help you achieve a well-rounded sense of well-being.
When we think of wellness, physical health often comes to mind first.
However, true wellness is a much broader concept, encompassing multiple dimensions that all contribute to our overall well-being.
Here’s a deeper look into the various facets of wellness and how they intertwine to create a balanced and fulfilling life:
Physical wellness is about more than just the absence of illness; it’s about thriving.
This dimension includes healthy behaviors like eating a balanced diet, staying active, getting enough sleep, and practicing safe habits.
By making these choices, you not only maintain your body but also set a foundation for a vibrant, energetic life.
Emotional and mental wellness are the cornerstones of perceiving and responding to life’s challenges.
It’s about understanding and managing your emotions, cultivating resilience, and maintaining a positive outlook.
Good mental health influences every other aspect of wellness, helping you navigate stress, build strong relationships, and find joy in daily life.
Spiritual wellness is often overlooked, yet it plays a crucial role in finding meaning and purpose.
Nurturing your spiritual side, whether through religion, meditation, or personal reflection, helps you align with your core values and find a sense of direction and inner peace.
Human connections are vital to our well-being.
Social wellness is about building and maintaining healthy relationships, communicating effectively, and being an active part of your community.
Strong social ties provide support during tough times and enhance the joys of life, contributing to a sense of belonging and security.
Financial wellness isn’t just about having enough money; it’s about managing your resources in a way that supports your life goals without causing undue stress.
Understanding how to balance income, savings, and expenses can lead to peace of mind and the freedom to enjoy life rather than being burdened by financial worries.
Vocational wellness goes beyond your job; it’s about finding fulfillment and purpose in what you do.
Whether through your career, hobbies, or volunteer work, using your skills and talents in meaningful ways contributes to your overall sense of achievement and satisfaction.
The environment you live in has a profound impact on your well-being.
Environmental wellness involves creating a living space that nurtures your health and happiness, whether it’s through reducing clutter, connecting with nature, or fostering sustainability.
A positive environment supports your other wellness goals and promotes a sense of peace and harmony.
Wellness is not a single entity but a complex, interconnected web of factors that work together to create a life of balance and fulfillment. By nurturing each of these dimensions, you can build a strong foundation for a healthier, happier life.
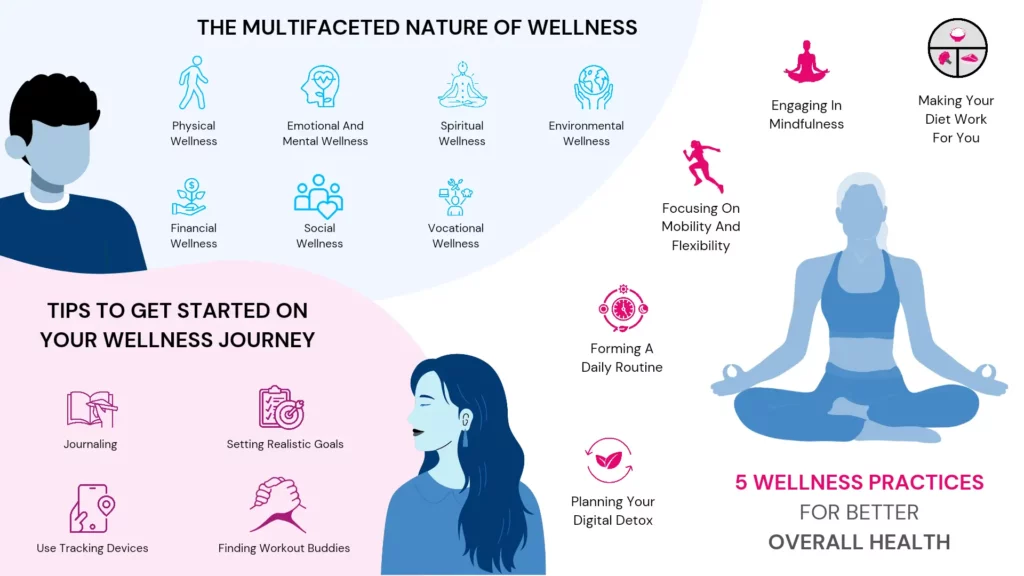
With a clear understanding of wellness and its dimensions, let’s look at 5 wellness practices that can improve your overall health!
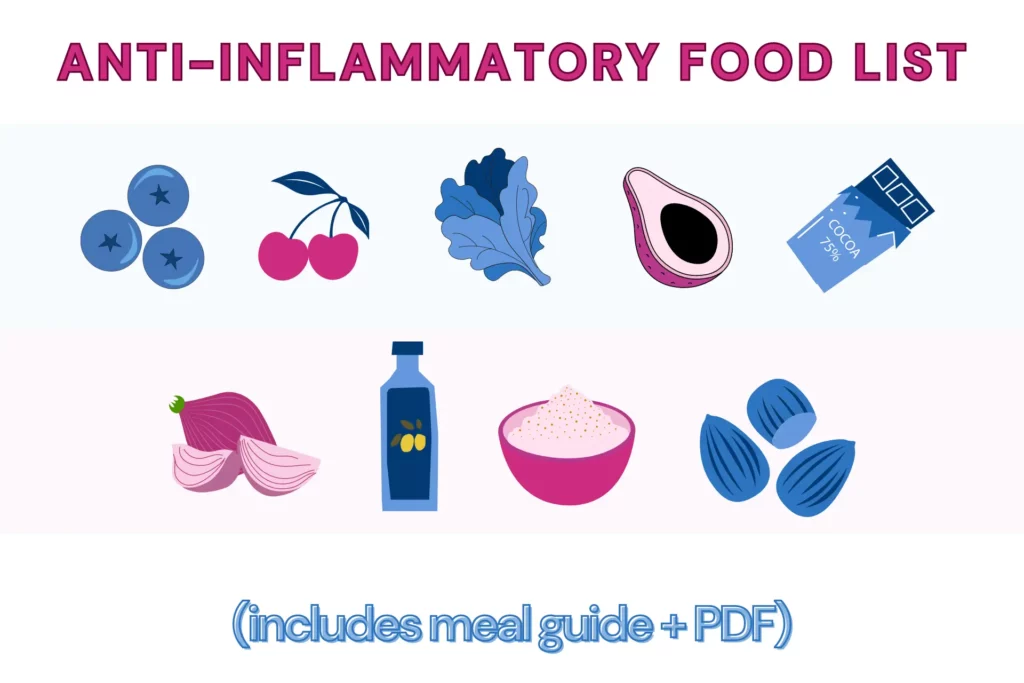
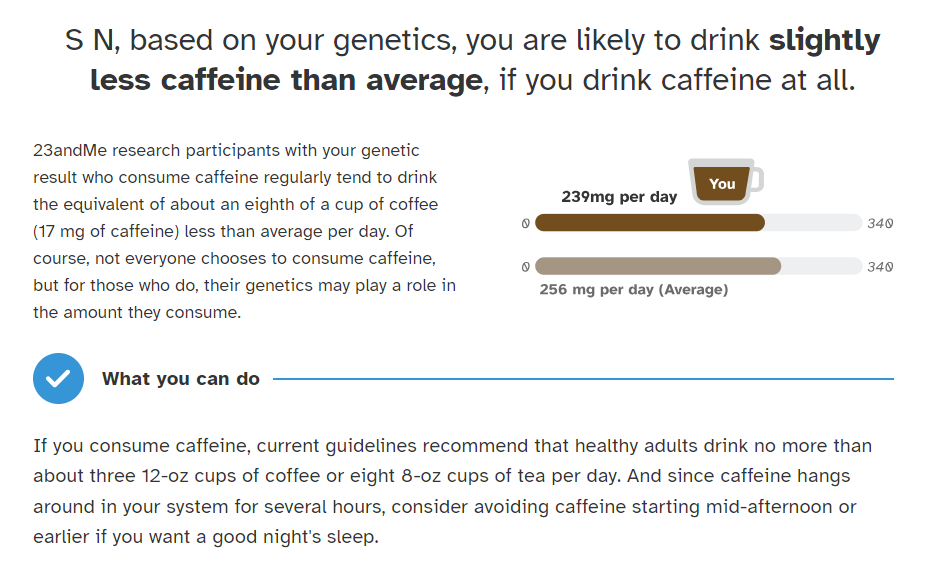
In today’s digital era, there's no shortage of diet and nutrition advice at your fingertips.
Unfortunately, with this abundance comes a flood of misinformation. The truth is, there’s no one-size-fits-all diet that works for everyone.
What works wonders for one person might not yield the same results for another.
This is because our bodies are unique and influenced by factors like lifestyle, environment, and even genetics.
The way your body processes nutrients can differ significantly from someone else’s, meaning a diet that’s effective for one person might not suit your needs at all.
That’s why personalized nutrition is so important. Instead of following the latest diet trend, it’s crucial to understand what your body specifically needs.
Working with a nutritionist can help you tailor a diet plan that aligns with your individual health goals and lifestyle.
Ultimately, the key is to listen to your body and focus on what makes you feel your best rather than relying on generalized advice.
Mindfulness and meditation have gained significant recognition for their profound impact on both physical and mental health.
The American Heart Association (AHA) recommends mindfulness practices that involve deep breathing, quiet contemplation, and focused attention as effective tools for reducing stress and enhancing overall well-being.
Research supported by the AHA highlights several benefits of mindfulness, including:
If you’re new to mindfulness, getting started can be simple and accessible.
Starting with just 5-10 minutes of mindfulness in a comfortable space can help anchor the habit.
There are also online videos on guided mindfulness that can give a boost.
Further, mindfulness is not just about sitting in a place and meditating; try being fully present while engaging in daily activities, such as eating, walking, or even washing dishes.
In the current fitness landscape, strength and weight training have rightfully earned their place in the spotlight.
However, flexibility and mobility often remain overlooked despite being crucial components of a well-rounded fitness routine.
These two aspects of fitness are not just about achieving a deeper stretch or a wider range of motion—they are key to aging gracefully and maintaining independence as we grow older.
Incorporating flexibility and mobility exercises into your routine offers a multitude of benefits:
As we age, the importance of mobility training becomes even more apparent.
Regular flexibility exercises can help ensure that, even in your later years, you maintain the ability to move freely and independently.
This can significantly enhance your quality of life, allowing you to stay active and engaged in the activities you love.
Humans thrive on routine, and establishing a daily structure can be a powerful tool for improving overall health and well-being.
Doctors and wellness experts worldwide emphasize the importance of having a consistent routine, as it provides numerous benefits beyond just physical health.
Creating and sticking to a daily routine can:
By forming a daily routine that works for you, you create a framework that supports both your physical and mental well-being.
This consistency not only helps you stay on track with your health goals but also contributes to a more balanced and fulfilling life.
In today’s hyperconnected world, we're glued to our screens—whether it’s our phones, laptops, or TVs.
While technology keeps us informed and entertained, too much screen time can start to wear us down, both mentally and physically.
That’s why taking a break with a digital detox can be so refreshing.
A digital detox simply means stepping away from your devices for a while to reconnect with the real world.
It’s about giving your mind a breather from the endless notifications and information overload.
This break can help you feel less stressed, sleep better, and improve your overall well-being.
Here’s how you can make the most of your digital detox:
By regularly taking time away from your screens, you give yourself a chance to recharge and focus on what really matters. It’s a simple step that can make a big difference in how you feel day-to-day.
Tips to Get Started on Your Well-being Journey This National Wellness Month
Now that you have a solid understanding of wellness and the practices that contribute to overall well-being let’s dive into some practical tips to help you kickstart your wellness journey. These tips are designed to be easy to implement and can make a real difference in your daily life.
Journaling is a powerful tool that allows you to articulate and reflect on your thoughts and experiences. It’s more than just writing down your day—it’s about setting clear goals, gaining clarity, and boosting your mental health.
To get started:
It’s easy to get excited about starting your wellness journey, but it’s important to set goals that are realistic and achievable. The biggest obstacle people face is burnout from setting goals that are too ambitious.
In our digital age, we have access to tools that can make our wellness journey more informed and personalized. Fitness trackers and health apps can monitor everything from heart rate to sleep patterns.
Staying motivated can be tough when you’re on your own, which is why finding a workout buddy or joining a community can be so beneficial.
By integrating these tips into your daily life, you can create a strong foundation for your wellness journey. Remember, it’s all about making small, consistent changes that add up to big improvements in your overall health and well-being.

Low-calorie High-volume Foods: The Key To Feeling Fuller For Longer
The Ultimate Guide To Anti-inflammatory Diet + Food List PDF
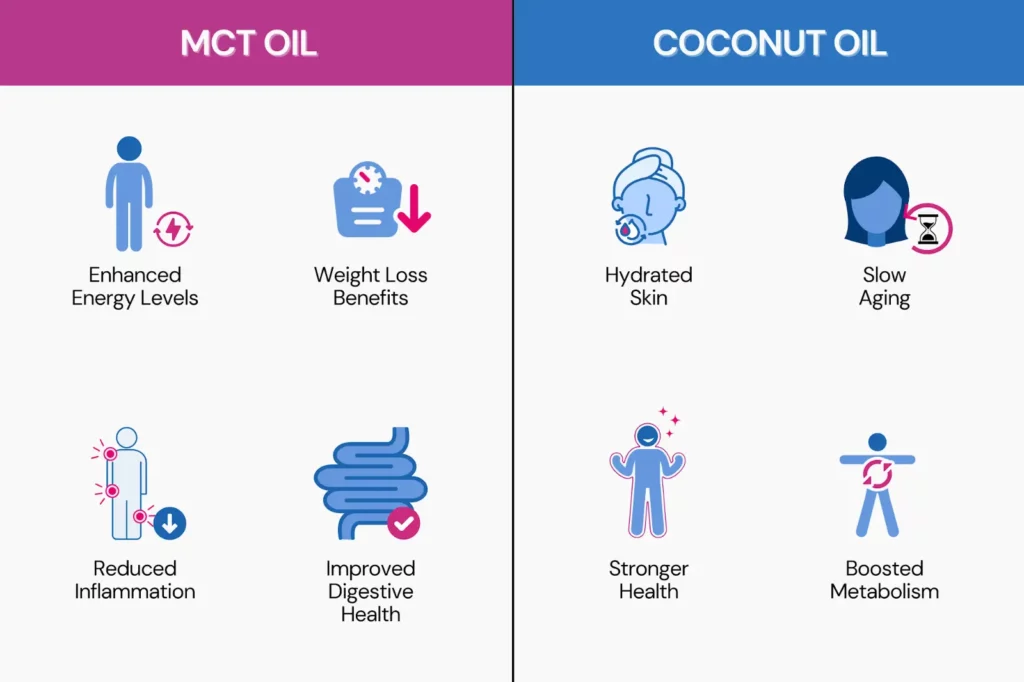
MCT Oil vs. Coconut Oil: Differences In Benefits And Risks
As of 2023, there are over 15 million Jewish people worldwide. If you suspect that you have Jewish heritage, there are several companies that offer a Jewish DNA test as part of their ancestry reports. Since Jewish people mingled within their communities for generations, their DNA has some markers and traits that were passed down through generations. These markers can help identify your Jewish ancestry even today, hundreds of years on. This article will elaborate on Jewish heritage, how to test for it, and what you could learn from your results.
Scientists identify certain markers in your DNA when you take a genetic test.
They can compare these markers to similar genomes in a database.
People with common ancestry often share certain markers that are specific to a region.
Scientists can estimate your ethnic ancestry based on the similarity and frequency of these markers in your DNA.
That’s how these tests can identify Jewish ancestry, which is actually a religious identity.
According to history, Jewish communities settled in Europe during the Roman rule of Judea.
They remained an independent community for a long time, marrying within their own communities.
Being genetically Jewish means that some or all of your ancestors were Jewish.
Thus, Jews of European descent may carry the same gene mutations and traits that have been passed on across generations within the Jewish community.
These genetic variations can be identified with Jewish DNA tests.
The most significant Jewish ancestries/communities include:
Most of the DNA tests right now can only identify Ashkenazi Jewish ancestry.
The other sub-groups have spread out wider and have mixed ethnicities.
A Jewish DNA test is similar to any home DNA test. You can order any ancestry DNA test kit and provide your sample (cheek swab or saliva).
The lab will then analyze your DNA and email the results.
There are three ways in which Jewish DNA test kits can identify your ancestry.
Your ancestry composition report highlights the regions from which your DNA originated out of thousands of regions in its database.
Since it is believed that the original Ashkenazi Jews originated from a particular region, the ancestry composition test may include this detail in their report.
Y-DNA tests are done on males to determine their paternal ethnic origins.
Since the Y chromosome is passed on from the father to the son, this can help trace the ancestors from the paternal side.
Women cannot get their paternal line tested with their DNA samples because they don’t carry the Y chromosome.
They may need to provide samples of their male relatives to run the test.
mtDNA or mitochondrial DNA is passed on from the mothers to their children.
These reports generate something called the mitochondrial haplogroup using mtDNA.
Mitochondrial haplogroups comprise people with similar mtDNA worldwide who have descended from a common female ancestor.
Four mitochondrial haplogroups occur frequently in people with Ashkenazi ancestry – N1b, K1a1b1a, K1a9, and K2a2a.
Europeans who carry these four haplotypes are more likely to have Jewish ancestry.
Being genetically Jewish means that some or all of your ancestors were Jewish.
You may carry the same gene mutations and traits that have been passed on across generations within the Jewish community.
Millions of people worldwide test their DNA to find their ancestral origins.
While curiosity is one reason, many want to understand their lineage and connect with possible relatives they don’t know exist.
Knowing your ancestry may also give a clearer idea about some of your traits and behavior.
A 2010 study mentions that people of Ashkenazi Jewish descent are at higher risk for conditions like cystic fibrosis.
The descendants of these individuals are at higher risk for certain genetic conditions compared to non-Jewish individuals.
Some studies recommend that Ashkenazi Jewish partners get tested for carrier status for the following diseases to know the risk their descendants carry.

Haplogroups: The Key To Unraveling Ancestral Origins

7 Physical Signs Of Viking Ancestry That May Suggest You Have Viking DNA
AncestryDNA vs 23andMe: Which Is Better For Raw Data Analysis?
Want to know how your genetic makeup impacts your health, ancestry, and fitness? Sequencing.com might provide the answers you need. As the DNA testing industry grows, Sequencing.com distinguishes itself by offering both affordability and comprehensive analysis. Founded by a leading genetics expert, this platform is changing the way genetic testing is approached. It provides advanced genetic analysis tools and a broad marketplace of DNA-related applications. Explore what Sequencing.com can offer and decide if it’s the right fit for your needs.
Sequencing.com is a DNA testing company that also offers a platform for various DNA-related apps.
Their marketplace includes both free and paid options for services such as ancestry analysis, health reports, and nutrition recommendations.
The company was founded by Dr. Brandon Colby, a genetics expert who earned an MD from Mount Sinai School of Medicine.
Sequencing.com aims to make genetic testing more affordable and accessible.
It provides free, unlimited DNA data storage to ensure secure storage, meaningful interpretation, and privacy of genetic data.
Additionally, the company offers detailed reports and tools that turn complex genetic information into practical health advice.
Sequencing.com provides a straightforward process for accessing genetic insights:
Sequencing.com offers an advanced Whole-Genome Sequencing (WGS) service that provides a detailed analysis of an individual's complete DNA.
While standard DNA tests analyze less than 0.1% of the genome, Sequencing.com's WGS covers the whole genome, including about 30,000 genes and 3 billion variants.
This service, which used to be very expensive, is now available at a more economical rate through Sequencing.com.
With a 'Privacy Forever' guarantee, Sequencing.com ensures that your data is never sold or shared.
WGS offers features like the Wellness and Longevity View and Genome Explorer and complete access to both raw and analyzed genome data.
These features make it valuable for both individuals and healthcare professionals.
Sequencing.com lets you easily import your DNA data if you've tested with 23andMe, MyHeritage, FamilyTreeDNA, Living DNA, HomeDNA, Vitagene, or DNA Land.
You can either import your data directly into your account or upload it from your PC.
Here’s how to do it in a few simple actions:
Your file is typically uploaded to Sequencing.com account within 15 minutes.
Already taken an ancestry genetic test with companies like 23andMe, AncestryDNA, MyHeritage, etc.? You can now upload your raw DNA files to access over 10 health and wellness reports (including methylation reports) starting from $30.
| Category | Trait | Free/Price |
| Health | Next-Gen Disease Screen | Free |
| Health Scan | Free | |
| Healthcare Pro | $199 | |
| Hormone Health | $59 | |
| Female Sexual & Reproductive Health | $59 | |
| Prevent Breast Cancer | $19 | |
| Inflammation And Immunity | $59 | |
| Cardiovascular DNA Wellness Report | $59 | |
| Disease Risk Genetic Test Report | $59 | |
| Healthy Heart | Free | |
| Immune System & Infectious Diseases | $19 | |
| Malignant Hyperthermia | $19 | |
| Basic Wellness | $4.99 | |
| Blood Traits and Conditions | $19 | |
| Birth Control Pill Risk | $1 | |
| Will Aspirin Help | $1 | |
| Promethease | Free | |
| Ancestry | Genetic Ancestry with Haplogroups | $59 |
| World Ancestry Report | $79 | |
| Map My Genes Archaeology Edition | $19.99 | |
| Map My Genes | $19.99 | |
| DNA Ancestry and Genealogy Report | $10.99 | |
| Am I An Einstein | Free | |
| Am I Related To Trump? | Free | |
| Relative Matching | DNA Family Finder | Free | |
| Am I Related? Relatedness Calculator | $9.99 | |
| Ancient Ancestry DNA and Me | Free | |
| Nutrition | Nutrigenomics: Nutrition Analysis | $29 |
| Nourish | $59 | |
| Weight Loss | $139 | |
| Beauty | Genetic Risk of Hair Loss | $19.99 |
| Health/Nutrition | Gut Health | $59 |
| Lactose Intolerance | Free | |
| Health/Nutrition/Fitness/Lifestyle | Empower | $59 |
| Bioinformatics/Health | Genome Explorer v3 | Free |
| Health/Lifestyle/Children | Brain Health: Mental Health & Mood | $59 |
| Cognitive Function Genetic Test Report | $59 | |
| Comprehensive Wellness | $189 | |
| Health/Children | Wellness and Longevity | $199 |
| Complete Genome Analysis | $189 | |
| Medication & Drug Response | $59 | |
| Inherited Traits Genetic Analysis | $129 | |
| Prevent Sudden Death | $19 | |
| Carrier Status | $29 | |
| Alzheimer’s Risk | APOE Gene Analysis | $39 | |
| MTHFR DNA Wellness Report | $29 | |
| Health/Lifestyle | Psychedelics PGx: Complete DNA Guide | $149 |
| Cannabis DNA Health Report | $29.99 | |
| Weather My Way +RTP | Free | |
| Enhanced Longevity | $59 | |
| My Personality Traits | $59 | |
| Arthritis Prevention | $9.99 | |
| Age with Strength | $4 | |
| Health/Nutrition/Children | Vitamins DNA Wellness Report | $39 |
| Blood Type Analysis | Free | |
| Health/Beauty | Melanoma Skin Cancer Prevention | $9.99 |
| Ancestry/Beauty/Children/Art/Bioinformatics | DNA Selfie | Appearance Predictor | $4.99 |
| Art | DNA Art | $299 |
| Health/Lifestyle/Children/Beauty | Genetic Detoxification | $69 |
| Sleep DNA Wellness Report | $39 | |
| Ancestry/Children | Santa and Me | Compare Your DNA to St. Nick | Free |
| Lifestyle/Children/Nutrition | Healthy Nutrition | $39 |
| Lifestyle/Nutrition | DNA Diet | $59 |
| Health/Nutrition/Fitness/Lifestyle/Children | TBG Total Wellness | $119 |
| Health/Fitness | Athletic Performance | Free |
| Health/Nutrition/Children/Bioinformatics | Genetic Counseling | $179 |
| Lifestyle/Beauty | Longevity DNA | $139 |
| Skin Genes | $59 | |
| Lifestyle/Fitness | Gene-In-Form Personalized Fitness | $49 |
| Children/Lifestyle | Personality DNA | $99 |
| Thrive | $59 | |
| Beauty/Children | Physical Appearance Genetic Report | $19 |
| Fitness/Children | Sports and Exercise | $99 |
| Fitness | RunDNA | $59 |
| Athletic Training Pro | $169 | |
| Fitness DNA Test Report | $29 | |
| Bioinformatics | Genome VCF | $19.99 |
| Sequencing Depth and Coverage | $9.99 | |
| Variant Effect Predictor | $19.99 | |
| Variant Discovery | $19 | |
| Imputation Analysis | $9.99 | |
| EvE Premium | $19.99 | |
| Short Read Mapper | $249 | |
| Clinical Annotator of Variants | $19.99 | |
| Genome Overview | $29.99 |
Navigating the Marketplace is relatively straightforward.
Users can search for specific apps or browse categories to find relevant reports.
The platform is designed to be user-friendly, allowing for easy access to both free and paid services. Some notable apps include:
Despite the variety of tools available, users have expressed concerns regarding the quality and comprehensiveness of the reports.
Some reports are noted to be dense and complex, potentially overwhelming for those without a background in genetics.
Additionally, the pricing structure can lead to unexpected costs, as many reports require separate purchases beyond the initial membership fee.
Based on forum discussions and social media conversations, users' experiences with Sequencing.com appear mixed.
Many are intrigued by the affordable whole genome sequencing offered, especially compared to earlier prices.
However, questions persist about the accuracy and comprehensiveness of results, particularly for rare disease and ancestry testing.
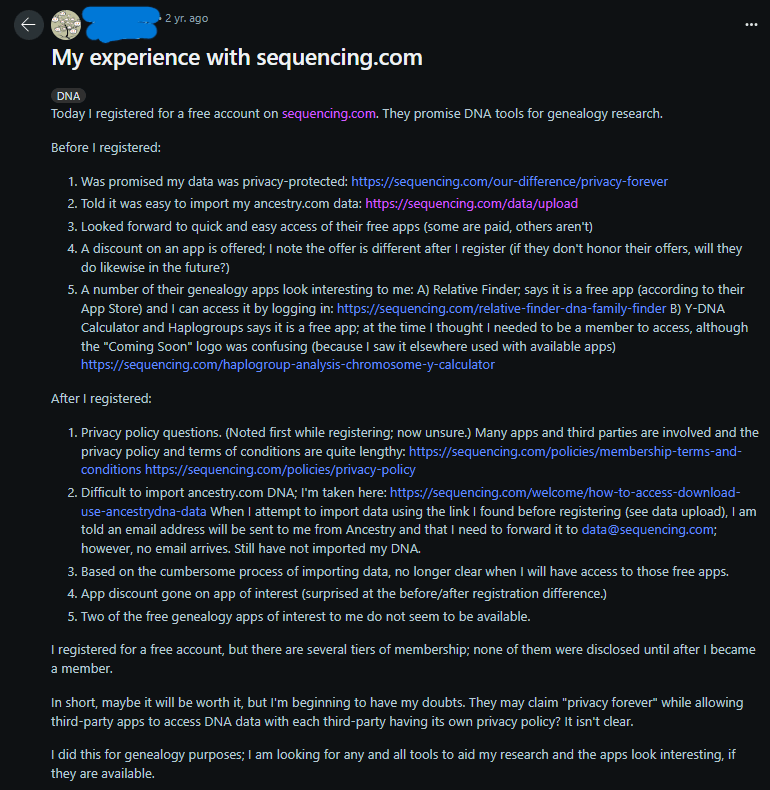
A recent review on Reddit highlights some challenges with Sequencing.com. The user appreciated the promise of privacy protection and the range of genealogy apps offered.
However, they encountered issues with importing Ancestry.com data, unclear privacy policies, and discrepancies in in-app discounts.
The review also mentioned that some apps appeared unavailable and that membership options were only disclosed after registration.
While the user is still hopeful about the service's potential, they expressed concerns about privacy and app accessibility.
Yes, Sequencing.com offers medical-grade DNA testing. They provide two key tests: the Ultimate DNA Test and the Ultimate Genome Sequencing.
The Ultimate DNA Test utilizes advanced microarray technology to examine over 30 million genetic variants.
On the other hand, the Ultimate Genome Sequencing offers clinical-grade 30x whole genome sequencing, covering your entire genome. This test also includes screening for over 2,000 genetic conditions.
Moreover, through their DNA App Store, you can explore numerous reports that deliver comprehensive insights into your health and well-being.
Sequencing.com holds an A+ accreditation from the Better Business Bureau and has gathered multiple reviews on its site, with an average rating of 3 out of 5 stars.
While some negative feedback relates to customer support, it seems that these issues have been addressed.
On TrustPilot, Sequencing.com has an average rating of 4.0 out of 5 stars. Many users appreciate the platform's ease of use and the valuable information it provides.
Customers have expressed their satisfaction with Sequencing.com, as seen in these reviews from Sequencing.com's testimonial page and TrustPilot:
One customer shared, "Mind-blowing insights! Everyone should have this information about their genetic makeup!"
Another customer expressed, "The results are real and true assessment. We discovered valuable information about my son's genetic conditions."
One user highlights, "I love this DNA Company. The monthly updates on health results are incredibly useful."
Anotheq reviewer mentions, "I am very satisfied with my experience ordering genetic testing from Sequencing. The disease screen and ancestry reports are fantastic."
Additionally, Sequencing.com is discussed on Reddit, where users and the company engage in conversations about their experiences.
This site is great. I’d been watching a lot of the Gary Becka videos about methylation tests and how they can help identify gene mutations and since we had already done a dna test with ancestry dna it was easy to just drop in our raw data from there and within just 1 day we had our results and are working towards our health now knowing ourselves better. At a much lower cost it’s a no brainer.
- John PerryReally great value compared to other medication gene testing, & you can see which genes you have & can cause affects to medication so even if they don’t have every single medication you need on the long list they give, you can research what medications are metabolized by said gene & learn even more. Really glad I found them 100% worth it. $25-$40 compared to $500-$900 for the same thing.
- N. Watson
Sequencing.com offers DNA testing and analysis services with a focus on affordability and accessibility.
They provide WGS, a detailed analysis of your entire genetic makeup.
You can upload DNA data from services like 23andMe, AncestryDNA, or MyHeritage or use their at-home DNA test kit.
Sequencing.com also offers a marketplace with various DNA-related apps for health, ancestry, nutrition, and more.
Customer reviews on Sequencing.com's website and Trustpilot are generally positive, highlighting valuable health insights and detailed reports.
However, a Reddit review raises concerns about data import issues, unclear privacy policies, and app accessibility.
While Sequencing.com provides medical-grade DNA testing, reviewing both positive and negative feedback is essential before making a choice.
2024 Update: Free Tools For 23andMe, AncestryDNA, FTDNA Raw Data Analysis

Family Tree DNA Review: What You Need To Know In 2024
AncestryDNA vs 23andMe: Which Is Better For Raw Data Analysis?
https://www.bbb.org/us/ca/pasadena/profile/biotechnology/sequencingcom-1216-1078918/customer-reviews
https://www.trustpilot.com/review/sequencing.com
If the confusing numbers and letters in your raw DNA data have left you scratching your head, you aren’t alone. Sites like 23andme, Ancestry, or MyHeritage DNA present your raw DNA data in a tabular format, with one column reserved for RSIDs. But what are RSIDs? Why do they matter? Why do they look so complicated? This article will answer all these questions, telling you everything you need to know about RSIDs and what they mean for your genetic report.
The term RSID stands for Reference SNP-cluster IDentification.
RSIDs are standard naming conventions for SNPs.
SNPs are short for single nucleotide polymorphisms.
They represent individual nucleotides on your DNA that have been mutated.
Mutations could happen by chance or be inherited from your parents.
These regions are called polymorphisms because they usually differ from person to person.
Scientists study DNA nucleotide-by-nucleotide (letter-by-letter) against a reference DNA sequence representing the human genome.
If they find a mismatch or a novel region, it is termed an SNP and denoted using an RSID.
When a researcher identifies an RSID, the mutated sequence is passed through a database that matches the sequence to a known RSID.
The format of an RSID is ‘rs’ followed by a number without a fixed length.
This number is incremental and grows with each new SNP that scientists discover.
A smaller or larger RSID number merely means it was discovered earlier or later, respectively.
It is unrelated to the SNP’s position in the genome and has no other biological significance.
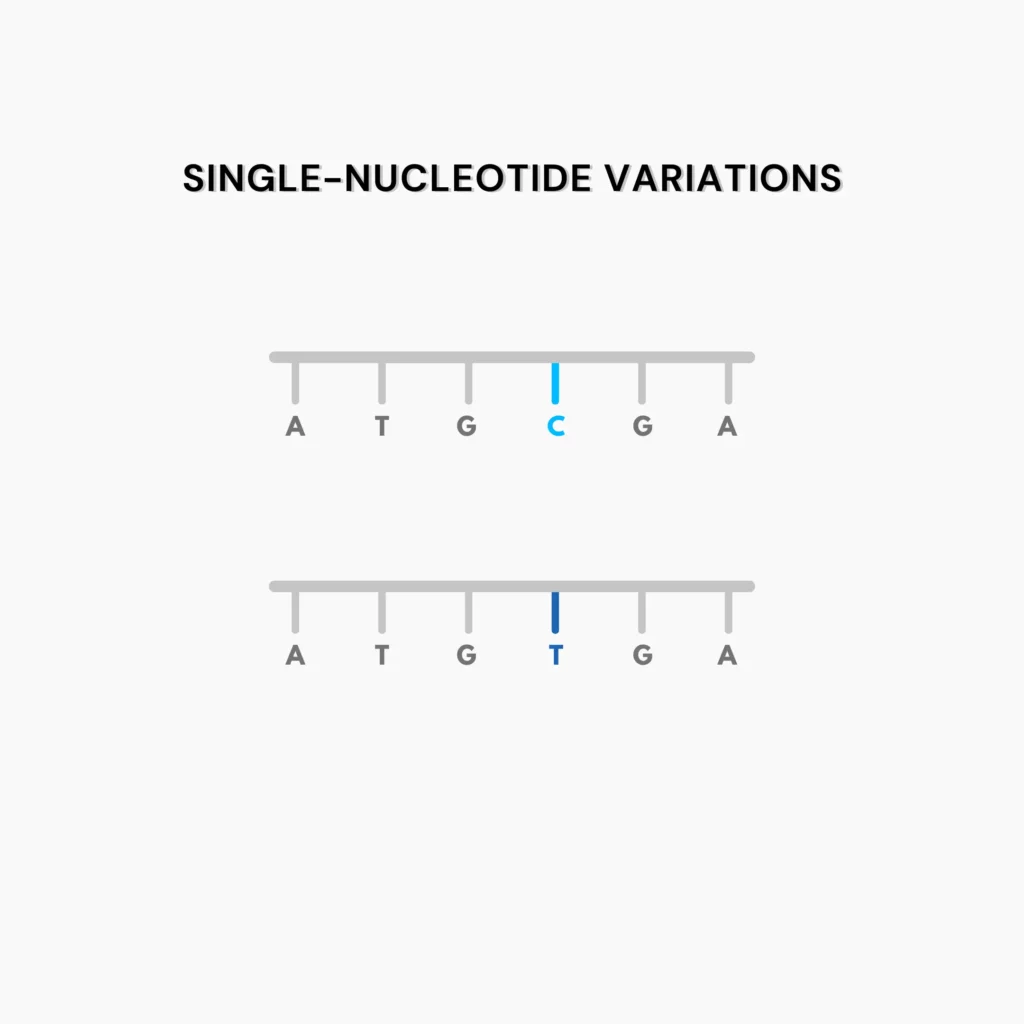
Scientists usually assign RSIDs to the following genetic variations:
These indicate variations in just one nucleotide.
For instance, nucleotide T may replace nucleotide C at a certain position in your DNA.
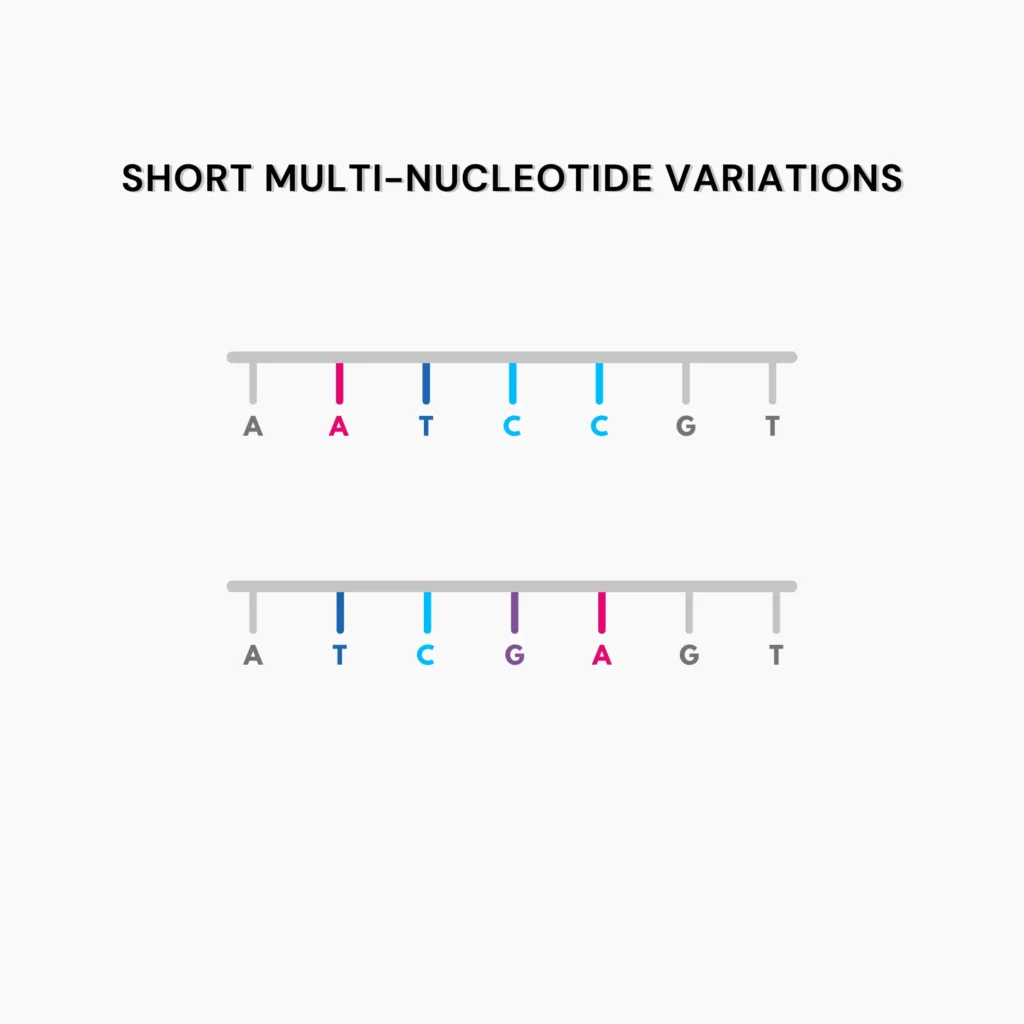
These imply variations in more than one nucleotide at a time.
For example, the nucleotide sequence ATCC at a certain position in your DNA may be replaced with the sequence TCGA.
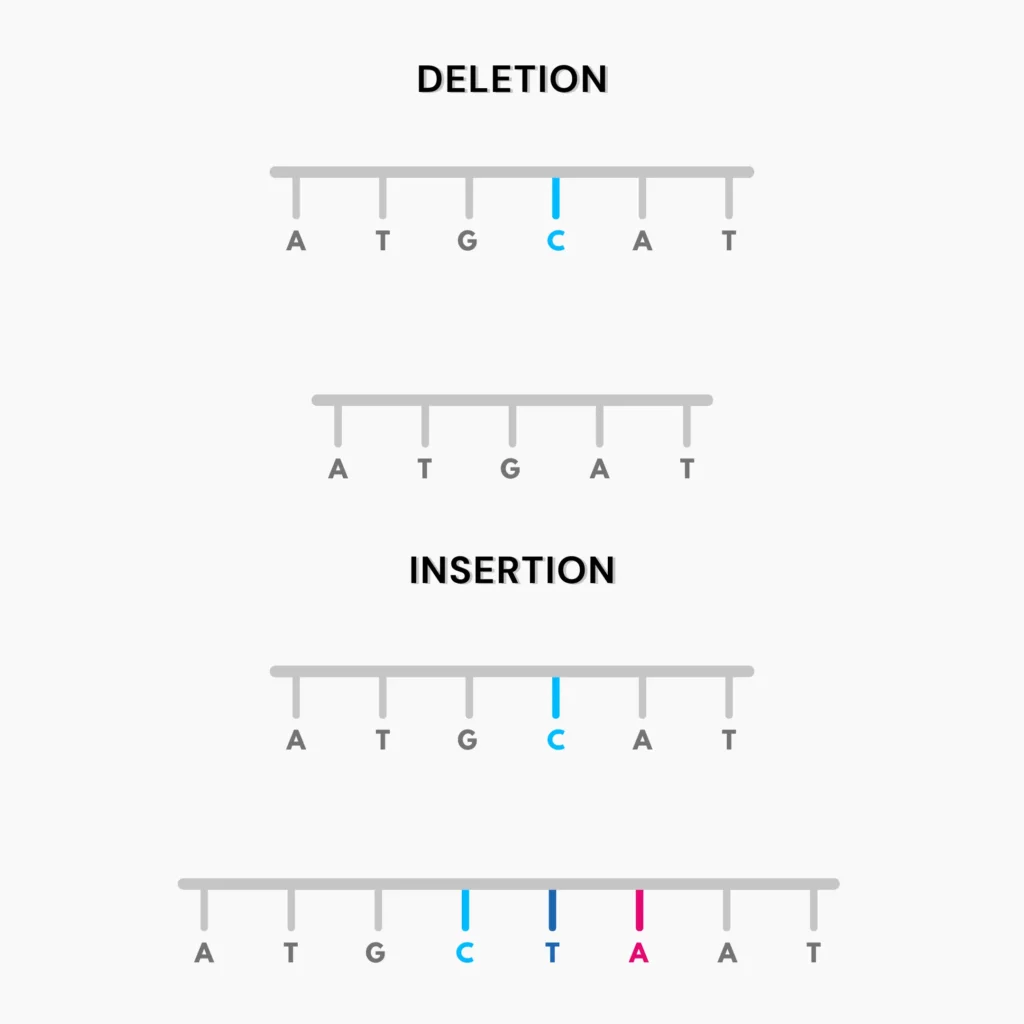
Deletions or insertions are types of genetic mutations often seen in DNA.
Deletions refer to missing nucleotides.
Say that the reference genome has the nucleotide C at a given position.
Deletion means that your DNA would be missing the C nucleotide at that position, shortening the sequence.
On the other hand, insertions refer to extraneous nucleotides.
For instance, your DNA could have the sequence CTA instead of C at the same position, lengthening the sequence.
Short tandem repeats (STRs) are sequences up to 6 nucleotides long that occur repeatedly in your genome.
They are highly polymorphic, meaning they are subject to slight mutations and differ from person to person.
Mutations or changes in STRs in your DNA are thus valid SNPs and are denoted by RSIDs.
Retrotransposons are genetic elements that flit around the genome at random.
They replicate several times, inserting DNA sequences at each of their destinations.
Thus, your DNA is bound to have a few retrotransposable elements at random positions.
A raw DNA data file contains tens of thousands of RSIDs on average.
However, an RSID doesn’t always spell trouble.
SNPs generally confer an increased likelihood of you having a particular trait.
These traits could be, but are not limited to:
Dozens of RSIDs govern any given trait.
Some RSIDs have more significant effects than others.
Their collective effect determines the presence of the trait in your DNA.
Genetic analysis companies weigh all the RSIDs in your DNA based on their significance to make recommendations for your lifestyle and well-being.
RSIDs and SNPs are one and the same.
SNPs are changes in your DNA, and RSIDs are methods of notating them.
SNPs are unexpected changes in the genome.
Thus, they can be termed mutations.
However, not all mutations are SNPs.
Restriction fragment length polymorphism (RFLP) is the simplest method to detect SNPs.
Certain enzymes can recognize specific sequences in DNA to cleave it at that position.
The presence of an SNP in these sequences would render the enzyme unable to cleave the DNA.
Thus, longer fragments indicate the presence of a SNP.
5 Ways Xcode Life Protects Your DNA Data

Analyze Your DNA Data For Depression – 2023 Updates

Are You A Morning Person? Analyze your DNA Raw Data To Find Out
https://customercare.23andme.com/hc/en-us/articles/212196908-What-Are-RS-Numbers-Rsid
https://www.ncbi.nlm.nih.gov/snp/docs/RefSNP_about
https://www.britannica.com/science/retrotransposon
https://www.genome.gov/genetics-glossary/Restriction-Fragment-Length-Polymorphism
The world of genetic testing is boundless, with several insights and traits available at your fingertips. AncestryDNA and 23andMe are two of the top players in this field, offering quality services to their consumers. Comprehensive DNA testing helps customers learn about their ancestry, health, and wellness. Both companies do a good job, but which one is better? This article will serve as a detailed review and comparison of AncestryDNA vs 23andme.
23andMe is a personal genomics company headquartered in California.
It was founded in 2006.
Since then, the company has sold more than 12.5 million DNA kits.
23andMe's mission is to help people access, understand, and benefit from the information present in the human genome.
23andMe offers four kinds of personal genetic services.
Health + Ancestry—Opting for this service will allow you to access more than 150 reports in the following categories.
| Service | Description | Price |
| Ancestry | Ancestry breakdown and 30+ trait reports– 80+ personalized reports– Ancestry percentages (to the 0.1%)– 2750+ geographic regions | $99 |
| Health + Ancestry | Everything in Ancestry service +– 150+ personalized reports– FDA-authorized reports– FSA/HSA eligibility | $199 |
| 23andMe+ Premium | Everything in Health + Ancestry service +– Heart health and personalized medicine reports– Health tracker– Health action plan– Historical Matches (new feature) | $199 for the first year, $69/yr after |
| 23andMe+ Total Health | Everything in 23andMe+ Premium +– Next-generation exome sequencing– Biannual blood testing– Access to clinicians | $999 for the first year, $499/yr after |
Did You Know? You can use your AncestryDNA test data to get up to 11 additional health and wellness reports from as low as $30. No new DNA test required. Reports within 24 hours.
AncestryDNA is a part of Ancestry LLC, founded in 1996.
Its parent company is based out of Utah.
The company has sold over 26 million testing kits to date.
AncestryDNA focuses exclusively on a person's ancestral traits and origin. The Ancestry website offers two kinds of testing services.
| Service | Description | Price |
| AncestryDNA | – Origins and ethnicity, including geographical regions– DNA matches to connect with your DNA relatives | $99$99 |
| AncestryDNA+ World Explorer Membership | Everything in AncestryDNA +– Access to over 40 billion records– 75+ traits on nutrition, fitness, and appearance – DNA Inheritance | $100, followed by $99.95 every 3 months $100, followed by $99.95 every 3 months |
| AncestryDNA+ All Access Membership | Everything in AncestryDNA + World Explorer Membership +– News articles and photos– Military records on Fold3– Up to 4 additional accounts | $199, followed by $149 every 3 months$199, followed by $149 every 3 months |
| Category | AncestryDNA | 23andMe |
| Ancestry services | More detailed and accurate – 25 million people in the database, more advanced tools | 50+ reports over 3000 regions, yet less detailed and accurate |
| Health services | Limited number of traits, no FDA approval | Many traits across 5 different health categories, FDA-approved |
| Cost | $99-$199 | $99-$999 |
| Timeline | 6-8 weeks after your sample is received; 12 weeks overall | 4-6 weeks from the time a sample is received at the lab; 10 weeks overall |
| DNA raw data download | Allowed | Allowed (was temporarily suspended due to a hack) |
Privacy is always a concern when you let any company access your personal information.
Users should be aware of what information these companies collect, store, and share with third parties.
Both companies have similar terms and conditions in their privacy policies.
AncestryDNA stores DNA details and samples without using your name or other personal information.
Both companies allow you to:
Note: Recently, 23andMe faced a massive hack that put the data of millions of people in jeopardy. Please review their policy in detail and talk to the customer care representatives for more clarity.
To get your 23andMe raw data, follow the instructions in this video:
To access your AncestryDNA account, follow the instructions on this page:
How To Login To Your Ancestry DNA Account + Get Health Reports At 70% Off!
Due to its more extensive database, AncestryDNA's ancestry results are more accurate.
For health information, 23andMe is better. The latter also has a better layout.
Ancestry results can vary between the two companies.
This happens because each company uses its own reference database and algorithm for report generation.
Further, the populations included in each service can also affect your results.
Ancestry briefly discontinued it to focus more on its ancestry services.
However, they soon reintroduced it as AncestryDNA Traits.

MyHeritage vs 23andMe: Detailed Review and Comparison

How Long Does 23andMe Take?
2024 Update: Free Tools For 23andMe, AncestryDNA, FTDNA Raw Data Analysis
A diabetes drug for weight loss? Semaglutide, also known by other brand names, is still making waves on the Internet even after years of FDA approval. In 2014, the FDA approved semaglutide (ozempic) for type 2 diabetes. But after clinical trails showed its promising effects on weight loss, in 2021, the FDA approved semaglutide (Wegovy), a once-weekly injection, for weight loss in adults when used in combination with a healthy diet and routine exercise. While these results are promising, delving into the potential side effects of semaglutide is essential.
Semaglutide is a medication used mainly to treat type 2 diabetes and chronic weight management.
It is commonly marketed under the brand names Ozempic and Rybelsus for diabetes and Wegovy for weight management.
As a GLP-1 receptor agonist, semaglutide mimics the incretin hormone GLP-1, increasing insulin release, decreasing glucagon levels, and slowing gastric emptying.
These actions lower blood sugar levels and suppress appetite, aiding in weight loss.
Semaglutide is administered via an injection under the skin once a week.
Clinical trials have shown promising results in terms of blood sugar (HbA1C) reduction and supporting weight loss compared to other treatments.
The medication is generally well-tolerated, with common side effects, including nausea, vomiting, and diarrhea, which tend to decrease over time.
Semaglutide has also shown potential benefits for cardiovascular health, lowering the risk of major cardiovascular events in patients with type 2 diabetes.
Its dual role in managing blood sugar and supporting weight loss makes it a valuable option for individuals struggling with both conditions.
However, it should be used under medical supervision, especially considering potential side effects and underlying health conditions.
Semaglutide supports weight loss via the following mechanisms:
But these effects may not be permanent. For example, the appetite and craving reduction effects aren't seen once the medication is stopped.
Numerous clinical trials have demonstrated the effectiveness of semaglutide for weight loss:
Semaglutide can have various side effects. While some are common and manageable, others are rare and may need medical attention.
Common side effects
Rare side effects:
Fatigue is a common side effect associated with semaglutide use, especially during the initial stages of treatment.
Several factors can cause this tiredness:
Yes, semaglutide can cause gastrointestinal troubles, which include constipation as well.
A 2021 human study published on NCBI found that GI issues were more common with semaglutide 2.4 mg compared to a placebo.
Constipation was reported in 24.2% of people taking semaglutide, compared to 11.1% taking the placebo.
Other GI side effects, like nausea, diarrhea, and vomiting, were also more frequent but were usually mild to moderate.
These side effects typically resolved on their own and were most common during or just after dose increases.
Importantly, these GI side effects, including constipation, were mostly non-serious, and only a few people (4.3%) stopped treatment.
The most commonly reported side effect of semaglutide is GI discomfort, which includes nausea, vomiting, and diarrhea.
This side effect can sometimes be severe, warranting discontinuing the medicine.
Despite the advantages of semaglutide, being informed about the potential long-term side effects is crucial.
Here are some key long-term side effects associated with semaglutide:
Semaglutide side effects are most noticeable when you first start taking the medication or after your dose is increased.
Like other medications, your body often needs time to adjust to the new treatment.
GI side effects are common during the initial weeks of treatment and usually improve over time.
However, individual experiences may vary. If you continue to experience severe or persistent side effects, consult your healthcare provider.
Managing the side effects of semaglutide involves several strategies, such as:
Contact your doctor if you have any health conditions or are taking medications, including over-the-counter drugs, vitamins, herbal products, or supplements.
Specifically, let them know if you have a history of pancreatitis, kidney problems, or diabetic retinopathy.
Also, discuss any concerns about low blood sugar and how to manage it.
Let your doctor know if you are pregnant, planning to become pregnant, or breastfeeding, as semaglutide's effects in these situations are not fully known.
Your doctor can guide you on whether semaglutide suits you and monitor potential interactions or side effects.

DHEA For Weight Loss: How Does It Work

Combating The Yo-Yo Effect: Avoiding Weight Regain After A Diet

How It Works: Genetic Testing For Weight Loss
https://www.drugs.com/semaglutide.html
https://link.springer.com/article/10.1007/s40618-024-02309-2
https://www.uclahealth.org/news/article/semaglutide-weight-loss-what-you-need-know
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9293236
https://www.webmd.com/drugs/2/drug-174491/ozempic-subcutaneous/details
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8961394
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10874596
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3281535
https://www.ncbi.nlm.nih.gov/books/NBK603723
https://www.medicalnewstoday.com/articles/drugs-ozempic-side-effects