Last year, my cousin and I were prescribed the same antibiotic for similar infections. While I recovered quickly, she experienced severe side effects, leading us to question why. This personal experience brings us to the concept of pharmacogenomic testing – a revolutionary method that uses an individual’s genetic profile to predict drug response. Intriguingly, it reveals why medications don't have a uniform effect on everyone. However, pharmacogenomic testing isn't universally applicable. Understanding its scope and limitations is vital for those considering it. This article delves into the heart of why this groundbreaking testing, while transformative for some, remains out of reach or ineffective for others. We'll uncover the challenges and limitations surrounding pharmacogenomic testing and urge you to engage with this pivotal topic. Our collective understanding and advocacy can pave the way for more inclusive and effective healthcare solutions.
Did You Know?
While some genes may affect the drug's efficacy, others may result in nasty side effects. That is why we want to help you and your physician understand your genetic changes to optimize treatment and outcomes. Xcode Life's Personalized Medicine Report profiles gene variants that influence your metabolic response to various drug therapies. The results of this report can be used as a supplement to the clinical decision-making process and reduce the cost and time associated with a trial-and-error treatment.
You can get your report using your existing DNA raw data file. No new DNA test required! Learn More
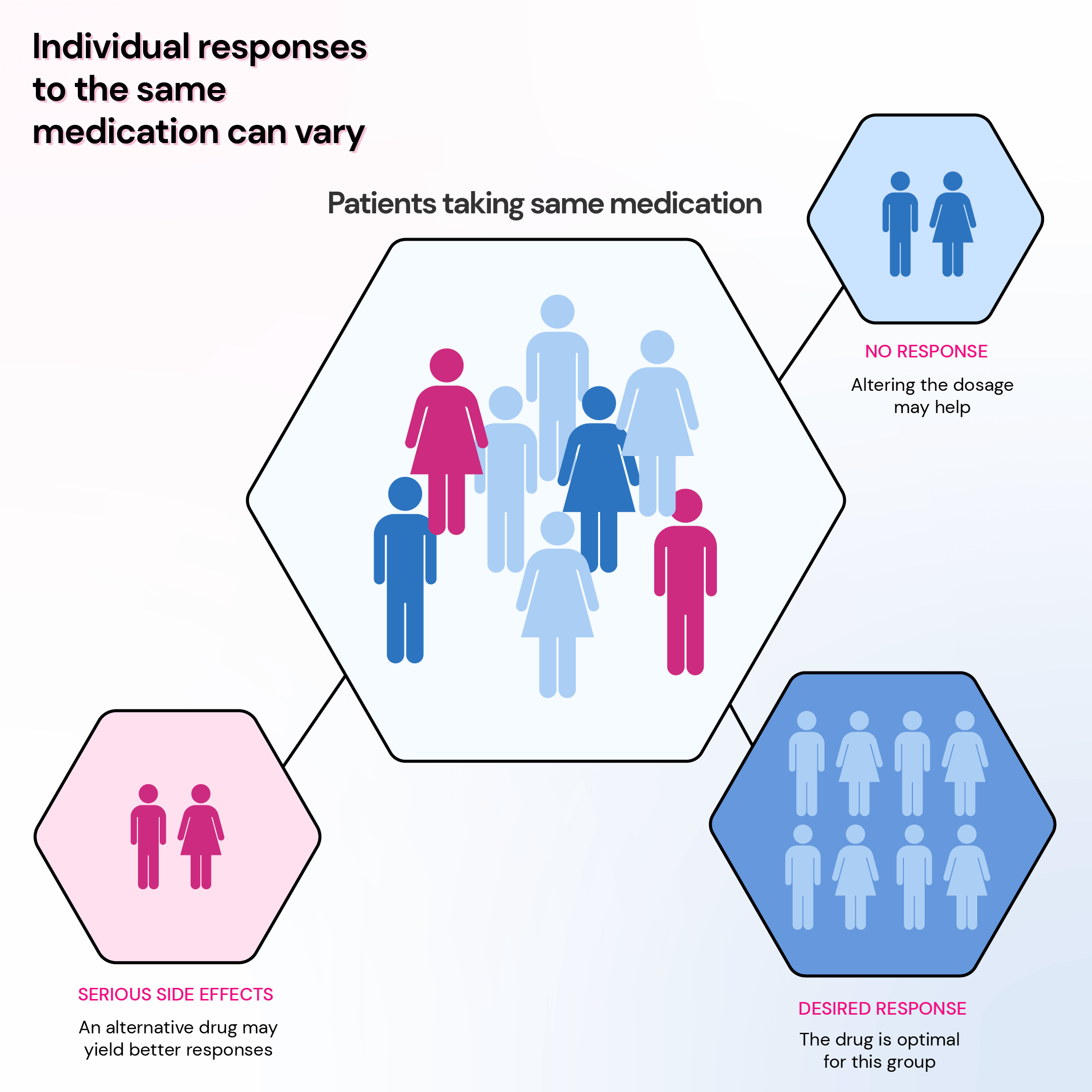
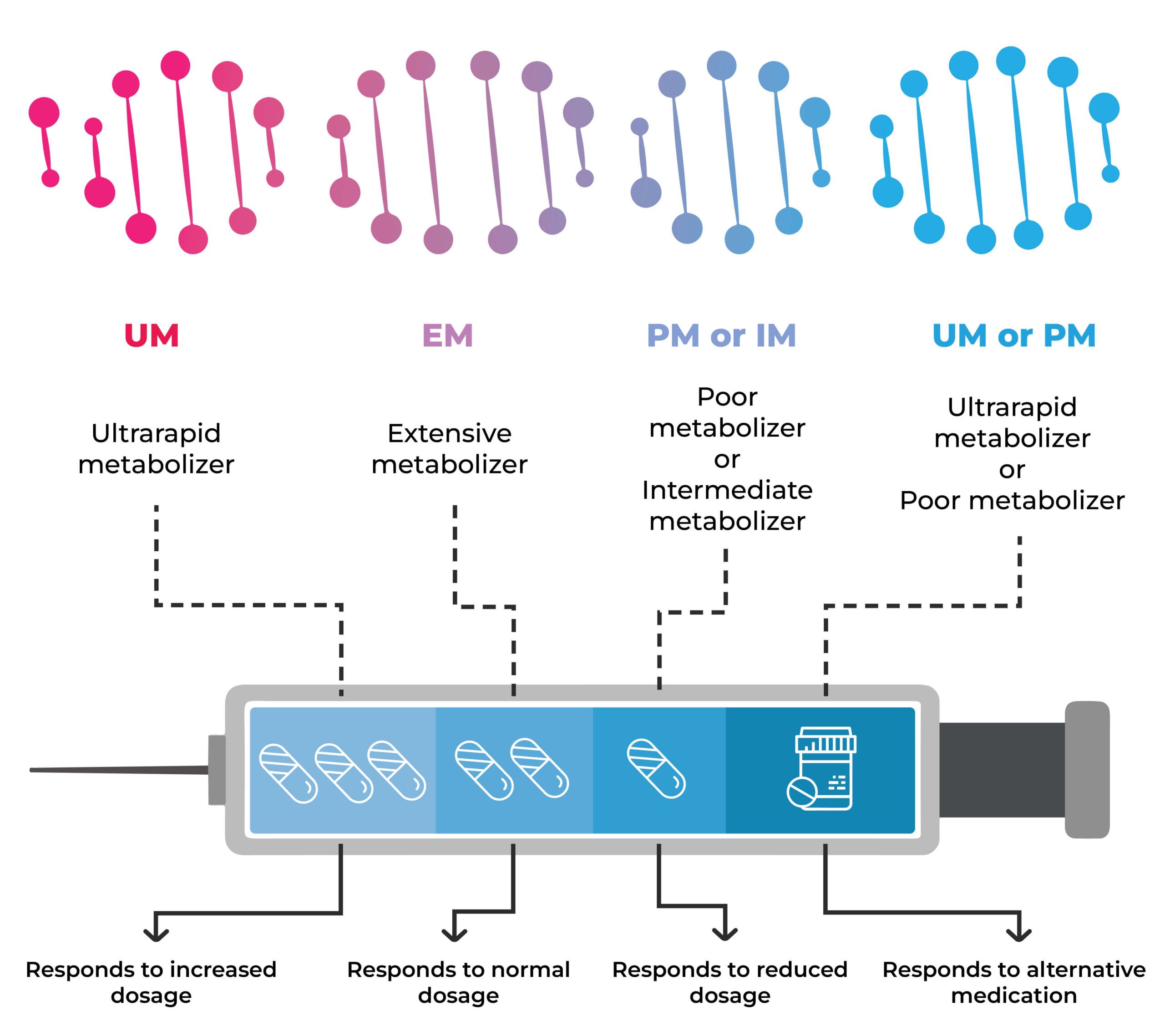
Pharmacogenomics is founded on the principle that genetic variations (single-letter changes in DNA that make everyone their unique self) among individuals influence their drug metabolism, transport, and response.
These genetic variations can impact an individual's drug effectiveness, safety, and dosage requirements.
For instance, some individuals possess genes that accelerate drug breakdown. Consequently, they may require a higher dosage to achieve the desired therapeutic effect than those who metabolize the drug more slowly.
Conversely, some individuals have genes that slow down drug metabolism. A lower dosage may be necessary to prevent adverse side effects.
Furthermore, a person's genetic makeup can affect their susceptibility to adverse reactions from certain medications, such as allergic responses, bleeding complications, or liver problems.
Pharmacogenomics utilizes pharmacogenetic tests to analyze an individual's DNA and identify variations in genes known to influence drug response.
These genetic factors play a pivotal role in several key aspects of the drug interaction process, including:
Pharmacogenomic testing, or pharmacogenetics, is a lab test typically done using saliva, blood, or cheek cell samples.
This testing is part of precision medicine, which integrates genetic, environmental, and lifestyle data to develop personalized disease treatment and prevention approaches.
Pharmacogenomic testing can serve various purposes, such as:
Pharmacogenomic testing might be suggested by your healthcare provider when initiating specific medications.
It is also considered if you are currently taking a drug that isn't giving the desired results or is causing severe side effects.
While not all medications have associated pharmacogenetic tests, some common examples include:
Xcode Life's Pharmacogenomic Test covers more than 500 genetic variants for drug responses.
Upon getting your pharmacogenomic test results, you may receive these key information:
Pharmacogenomic test results use a standardized nomenclature, ensuring consistent interpretation across different laboratories.
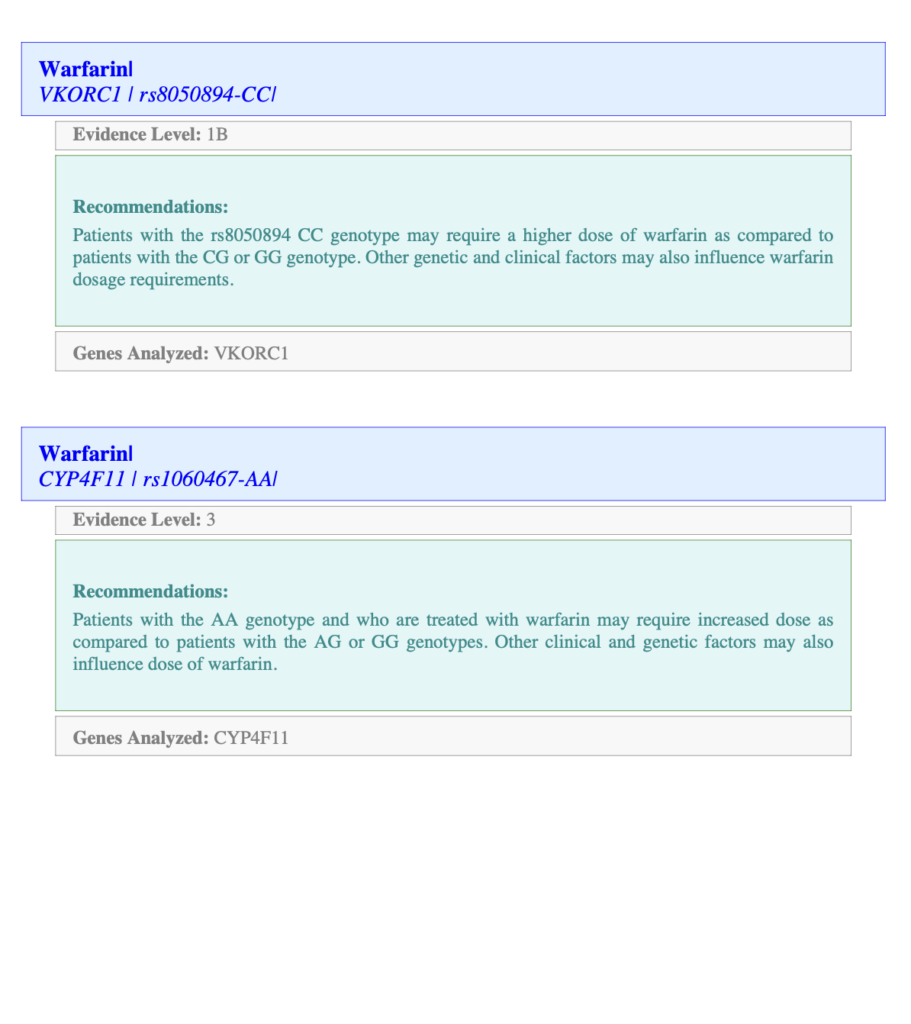
Xcode Life's report provides details on the genetic variant analyzed for each drug. In the image below, the first line after the drug name "Warfarin," you can see the gene and the variant analyzed, along with your genotype.
The Evidence Level stands for how strong the association is between the variant and the drug interaction. Level 1 is the strongest.
The Recommendations section provides information on the genotype in the context of drug interaction.
While pharmacogenomic testing is generally accurate in predicting drug responses for most genes, accuracy can vary based on the gene and test type.
It's essential to know that pharmacogenomics is a developing field that requires ongoing research to understand the complex interplay between genes and drug responses fully.
Pharmacogenomics has been applied to several areas of medicine, such as psychiatry, cardiology, oncology, neurology, and infectious diseases.
Some examples of drugs that have pharmacogenetic guidelines or labels include:
Pharmacogenomics' limitations include a variety of factors that go beyond genetic makeup and can impact the effectiveness of personalized drug therapy.
Some key limitations include:
After discussing it with your doctor and carefully considering its potential benefits and drawbacks, the decision to undergo a pharmacogenomic test should be made.
It would help if you considered the following questions:
Remember, the benefits of pharmacogenomic testing vary from person to person, as it personalizes medication management based on individual genetic characteristics.
It's important to consult your doctor to determine if pharmacogenomic testing is appropriate for you.
Pharmacogenomics aims for personalized drug therapy, exploring how genes influence how our bodies respond to medications.
Results provide genotype details, drug response implications, and medication management guidance. However, accuracy varies by gene and test type.
Pharmacogenomics has applications in various medical fields. Despite this, limitations exist, including incomplete genetic explanation, drug interactions, health conditions, lifestyle factors, cost, and complex data interpretation.
Whether to get a pharmacogenomic test depends on factors like medical conditions, family history, access to testing, and guidance from a qualified healthcare professional.
Pharmacogenomic testing isn't a magic fix; decisions should involve consulting your doctor and carefully considering the pros and cons.
https://medlineplus.gov/genetics/understanding/genomicresearch/pharmacogenomics/
https://medlineplus.gov/lab-tests/pharmacogenetic-tests/
https://www.cdc.gov/genomics/disease/pharma.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4000170/
https://www.fda.gov/drugs/science-and-research-drugs/table-pharmacogenomic-biomarkers-drug-labeling
https://clinicalinfo.hiv.gov/en/glossary/hla-b5701-test
https://my.clevelandclinic.org/health/articles/pharmacogenomics
From that late-evening espresso to the thrill of an impending holiday or the relentless pressures of a busy workweek, numerous factors can disrupt our nightly slumber. Yet, what often escapes our notice is the stealthy role that steroids, commonly taken for allergies or inflammation, may play in keeping sleep at bay. Gaining a deeper understanding of the intricate relationship between steroids and sleep is crucial in safeguarding ourselves against sleep disorders such as insomnia. This awareness is key to not only recognizing the potential impact of these medications but also to implementing strategies to ensure a peaceful night's rest.
Did You Know?
Your genes encode drug-metabolizing enzymes, drug targets, and other proteins related to the action of drugs. Each individual has a unique genetic makeup. Hence, they might respond differently to certain medications. While some genes may affect the efficacy of the drug, others may result in side effects like insomnia. That is why we want to help you and your physician understand your genetic changes to optimize treatment and outcomes. Xcode Life's Personalized Medicine Report profiles gene variants that influence your metabolic response to various drug therapies. The results of this report can be used as a supplement to the clinical decision-making process and reduce the cost and time associated with a trial-and-error treatment. Learn More
Corticosteroids or steroids are anti-inflammatory medicines that treat autoimmune and inflammatory conditions.
Corticosteroids reduce inflammation and weaken the immune system.
Steroids are prescribed to treat and manage conditions like the following.
Corticosteroids are different than anabolic steroids, which are used to increase muscle mass.
Steroid medications come in different forms.
Steroids usually don’t cause significant side effects if they are taken for a short time in smaller doses.
When used for more extended periods, steroids may cause the following side effects.
One of the very commonly noticed side effects of steroids is sleep disturbances, including insomnia.
Insomnia is the inability to fall asleep or stay asleep all night.
People with insomnia don’t get good quality sleep at night, making them groggy in the morning.
An older study looked at the effects of hydrocortisone (a type of corticosteroid) on brain function and sleep. This study reports that hydrocortisone decreased Rapid Eye Movement (REM) sleep, which is associated with poor sleep quality.
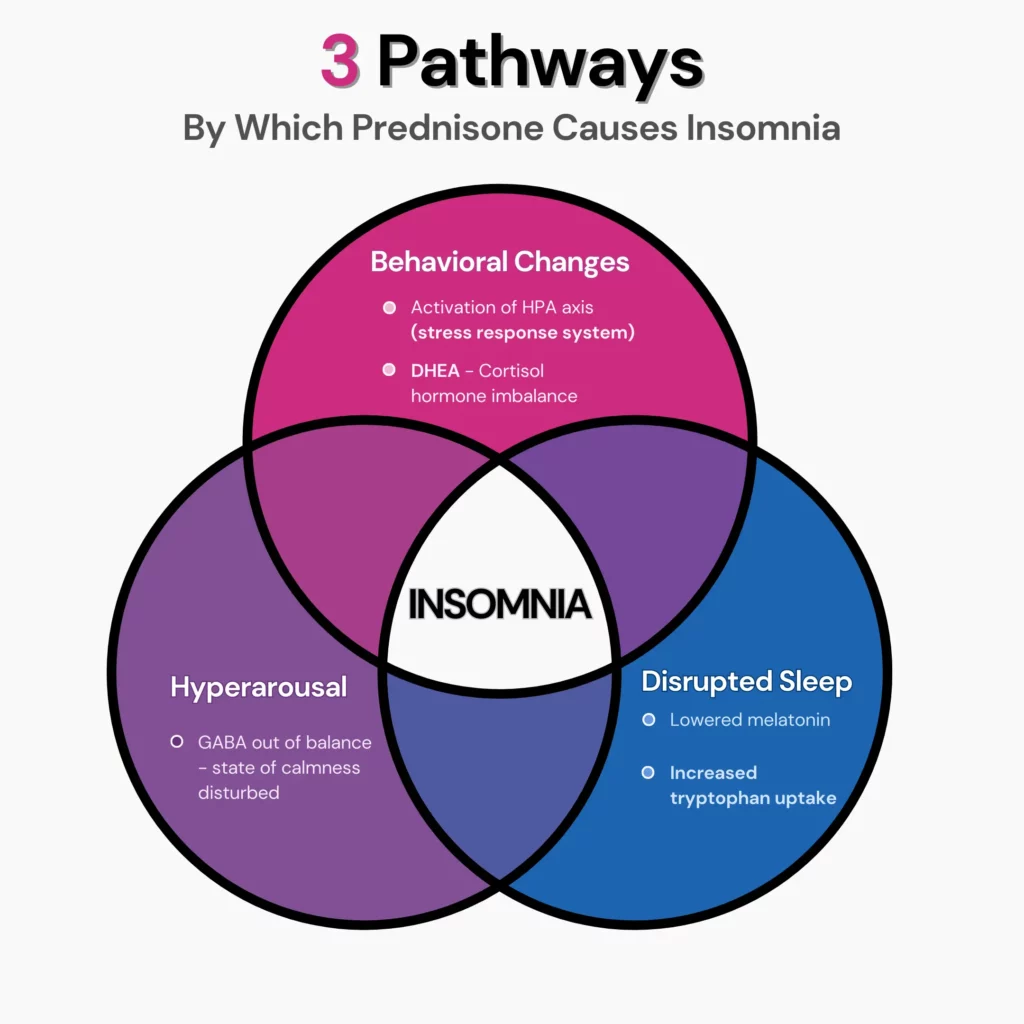
Studies suggest that steroids have similar structures to cortisol, the stress hormone.
The body makes cortisol when it is under stress. Usually, cortisol levels are high in the mornings and low at night to help the body rest.
Steroid medications disrupt the natural cortisol rhythm and keep the brain active at night.
Steroids may also reduce serum melatonin levels. Melatonin is a hormone produced by the brain during darkness.
Melatonin encourages the body to sleep. Steroids may cause sleep problems by reducing melatonin secretion.
All types of steroids may cause insomnia when the dosage is high or the period of usage is extended.
Corticosteroid tablets may show substantial side effects because the medication affects all parts of the body compared to injections or sprays that have more focused areas of action.
The following are the risk factors for steroid-induced insomnia.
While it is clear that corticosteroids may cause insomnia, for some people, these drugs can be important and cannot be avoided.
So, here are some tips from sleep experts on handling the drug's side effects.
All studies report that the higher the dosage and the more extended the period of use, the risk of insomnia is high.
A 2020 study reports that symptoms of insomnia may start from day three of corticosteroid therapy and continue for as long as the medication is taken.
Talk to your doctor about the dosage and period of use, and try lowering both if possible.
Taking steroids in the evening or before bedtime may increase the chances of staying awake. Morning doses seem to be better for this reason.
Since corticosteroids drain melatonin levels, replenishing lost melatonin may help fall asleep at night.
Talk to your doctor to see if you could start melatonin supplements while on corticosteroids.
Steroid Withdrawal Syndrome (SWS) is an unpleasant side effect of stopping steroids abruptly, especially if you have been using them for a longer period.
SWS can cause muscle stiffness, fatigue, joint pain, fever, or sleep disturbances. SWS could also be a contributor to insomnia.
Doctors recommend slowly waning off the dosage to help prevent SWS.
HELPME SLEEP is a nomogram created to help handle sleep problems in critically ill patients.
Individuals struggling with steroid-induced insomnia can also pick up pointers from this nomogram to help handle the issue.
Some tips that can help include:
Hand-picked Content For You: Can Lack Of Sleep Cause Nausea? How To Prevent It?
https://pubmed.ncbi.nlm.nih.gov/7829766/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7357890/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4008542/
https://pubmed.ncbi.nlm.nih.gov/29061489/
https://pubmed.ncbi.nlm.nih.gov/3614616/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4052587/
https://www.nhs.uk/conditions/steroids/
Imagine having a tiny architect inside every cell of your body, designing and defining everything from your smile to the way you laugh. These microscopic architects, the genes, play a fascinating role in making you, well, you!
Genes are segments of DNA packed within the cells of every living creature. Imagine a long, winding train with countless carriages; each carriage here represents a gene. These genes carry the instructions for making proteins, which are the fundamental components of our body, influencing everything from our eye color to how our body fights diseases.
Think of genes as information vaults. Each one stores detailed instructions for making the proteins necessary for your body's various functions. The human genome is an impressive collection of about 20,687 protein-coding genes, each a key player in your biological makeup. From determining your hair texture to influencing how you metabolize food, genes are the directors behind the scenes of your life's play. The way they are expressed, or 'turned on and off,' determines how these proteins are produced. Various factors, including environmental elements and lifestyle choices, influence this process.
Genes come in different versions, known as alleles, which bring variety and individuality to life. For instance, one allele may lead to curly hair, while another results in straight hair. It's the combination of these alleles, one inherited from each parent, that weaves your unique genetic tapestry. This diversity extends beyond physical traits; it includes differences like having dimples, blood type, or even susceptibility to allergies. Alleles are the essence of genetic diversity, playing a crucial role in both individual uniqueness and the broader scope of human evolution.
The study of genes and their functions has led to groundbreaking discoveries in medicine and biology. For instance, understanding genetic mutations has been crucial in identifying the risk of certain diseases and developing targeted therapies. Moreover, the versatility of genes is so profound that they can influence how we metabolize foods and medicines - a key factor in personalized medicine.
And that’s a wrap on genes! They're not just biological jargon; they're the essence of our physical and even behavioral traits. Join us next time in the "2-Minute DNA Digest" as we dive into another exciting aspect of genetics. Remember, every part of you tells a story written in the language of genes!
Are you looking for a natural way to support your liver's detoxification process? Folate, a B vitamin found in many foods, may be the answer you're searching for. Not only does it play a crucial role in DNA synthesis and cell division, but recent studies have shown that it can help with liver detox by washing the harmful toxins out of the body. Keep reading to find out if adding folate to your diet could be the key to a healthier, happier liver.
Did You Know?
Vitamin B9 needs to be converted into a form called tetrahydrofolate or THF to be effectively used by the body. The conversion of folic acid to THF is carried out by an enzyme called THF reductase. This conversion is a very crucial step in the MTHFR cycle. The MTHFR gene is a well-known gene associated with folate deficiency. This gene helps the conversion of inactive vitamin B9, such as folate or folic acid, to active B9, the THF. 30-60% of people have a change in this gene that ultimately leads to low vitamin B9 levels in the body. Other genes like MTYL1 also influence your vitamin B9 levels. A simple genetic test can reveal your genetic status of vitamin B9 deficiency. Learn more.
Detoxification is the metabolic filtration process by which the liver rids the blood and body of harmful and foreign substances.
It helps convert toxins into waste products, cleanses the blood, and metabolizes nutrients and medications to provide the body with essential proteins.
For this reason, it is of paramount importance to keep your liver healthy.
Folate or folic acid is a water-soluble vitamin in several foods, including leafy greens.
This essential vitamin plays a vital role in many biosynthetic processes, acting as a donor or carbon molecules like methyl groups (called methylation) to other organic compounds.
This process of methylation forms a part of the liver’s detoxification process.
The normal plasma folate levels in adults are 2 to 20 ng/mL.
Adults require about 200 micrograms of folate every day, while pregnant women are recommended to take 400 micrograms daily throughout their first trimester.
When the intake of folate is less, it can lead to folate deficiency. Common symptoms of folate deficiency are:
Elevated liver enzymes in routine liver function tests indicate a problem with the organ.
Eating a healthy, balanced diet and regular exercise are two effective and inexpensive ways to keep the liver enzymes within the normal range.
Adding folate to the diet or taking folic acid supplements is known to lower liver enzymes.
A 2016 study linked folate deficiency to increased alanine transaminase (ALT) (a type of liver enzyme) levels and liver damage.
The study also stated that folic acid intake lowered ALT levels in people with liver damage.
Several studies have found that folate can help slow down the progression of nonalcoholic fatty liver disease and reverse inflammation and fibrosis (thickening of scar tissue in the liver).
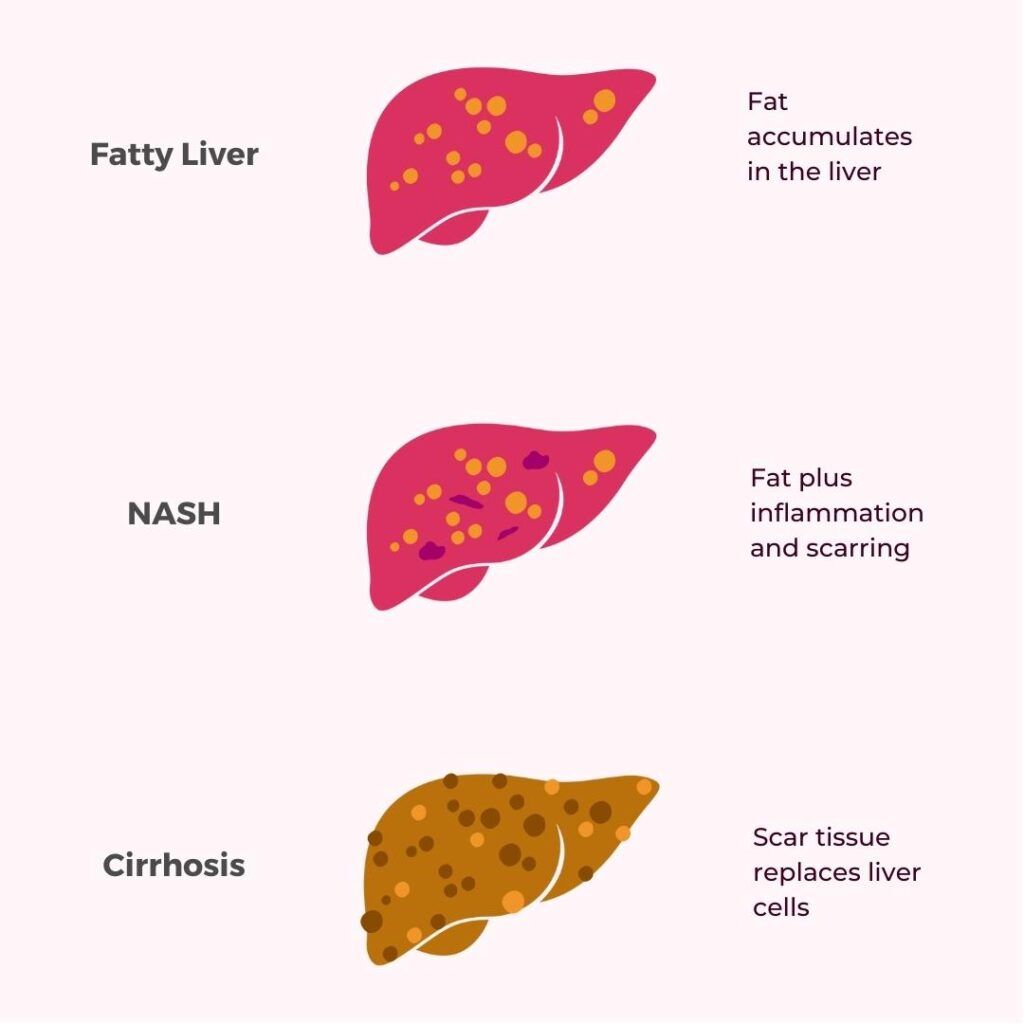
Nonalcoholic fatty liver disease (NAFLD) is a condition characterized by fat build-up in the liver.
1 in 4 Americans suffers from nonalcoholic fatty liver disease, resulting in cirrhosis and cancer over time.
Scientists at Duke-NUS Medical School in Singapore have discovered a mechanism that leads to fatty liver disease.
Their research found that vitamin B12 and folic acid supplements can reverse the process that leads to NAFLD.
Nonalcoholic fatty liver disease is an umbrella term for a range of liver conditions affecting people who drink little or no alcohol.
One of the study's authors highlighted that fat deposition in the liver is reversible in its early stages.
If the condition is allowed to progress, the excess fat results in liver inflammation. This is termed nonalcoholic steatohepatitis (NASH).
Unfortunately, there are no treatments for NASH, as scientists don’t completely understand the mechanics of the disease.
What is known is that NASH is associated with elevated levels of homocysteine (an amino acid).
Note: High homocysteine levels are toxic to the body; this amino acid is broken down by 2 vitamins - B9 and B12.
The authors found an association between homocysteine and NASH progression in preclinical models and humans.
When there’s an excess of homocysteine, it attaches to some liver proteins, thereby preventing them from doing their functions.
One such protein implicated in NASH is syntaxin 17, which is involved in the transportation, digestion, and removal of fats.
When homocysteine binds to syntaxin 17, it prevents the protein from removing fat from the body.
This drives the development and progression of fatty liver disease to NASH.
An Inexpensive Therapy For NASH
The study reported that two vitamins (B12 and B9) increase syntaxin 17 levels by breaking down excess homocysteine in the body.
The increased levels support the removal of fat cells.
This was found to slow down NASH progress and reverse liver inflammation and fibrosis.
The author says, “Vitamin B12/B8 could be an inexpensive way to prevent and delay NASH progression. Further, homocysteine levels can be used as a marker to assess NASH severity.”
Several foods are rich sources of vitamin B12 and folate.
A few common folate-rich foods to include in the diet:
Adults need about 1.5 micrograms of vitamin B12 daily.
Foods that are excellent sources of vitamin B12 are
Many factors like unhealthy lifestyles, exposure to pollution, and hard metals in diets can impair detoxification, resulting in several chronic conditions.
While the liver is the primary detoxification center in the body, other organs like the intestines, kidneys, and skin also play significant roles.
Here are some ways to support your liver detox:
We are exposed to toxins and harmful chemicals every day.
Eating a clean diet and drinking hygienic water are the best ways to reduce your toxic load.
Here are some ways to lower your toxin load:
While a glass of alcohol or a smoking session may seem relaxing at the end of a tiring day, they surely pump your body with harmful chemicals and toxins.
Limiting your alcohol and caffeine consumption and staying clear of any kind of smoke (active or passive) do a big favor to your liver.
Replacing smoking and drinking with healthy de-stress activities like walking, going to the gym, or doing yoga can support your liver detox.
Glutathione is an antioxidant found in plants and is made up of the amino acid glycine, cysteine, and glutamic acid.
It is one of the major substances responsible for detoxification.
Glutathione can be taken as a supplement to boost liver detox.
Disclaimer: Nutritional supplements should be taken only after consulting a qualified medical practitioner. This article is for informational purposes only and doesn’t serve as a prescription for any drug/supplement.
Gut health is important for immunity and overall health, and well-being.
When there is inflammation in the gastrointestinal tract, it makes eliminating toxins in the intestines and the liver difficult, increasing the load on the kidneys.
Eating foods that cause inflammation, imbalance of healthy bacteria and yeast, and accumulation of harmful heavy metals can affect detoxification.
A clean diet rich in antioxidants and healthy nutrients can support the liver’s detoxification process.
Changes in certain genes can result in impaired detoxification.
A genetic mutation (abnormal change) that commonly affects detoxification is the MTHFR mutation.
The MTHFR gene produces an enzyme that converts inactive vitamin B9 to the active form.
Certain changes in this gene can result in MTHFR enzyme deficiency; this can decrease the levels of active vitamin B9, leading to homocysteine buildup.
This impaired gene functioning is said to cause chronic conditions like cardiovascular diseases, diabetes, cancer, asthma, multiple sclerosis, Alzheimer’s, and autism.
Knowing about your genes and the presence of mutations can help you and your doctor take appropriate measures to restore normal detoxification.
A glass of wine after a long day may be a great way to unwind. In some people, though, drinking this alcoholic beverage can cause a headache and facial flush after. If you have been that person who has never been able to tolerate red wine, then recent studies report that quercetin, a type of polyphenol in red wine, could be the culprit. Keep reading to learn more about the study and what it concludes. If you love red wine but just can’t handle the headaches, we also have tips on enjoying your favorite drink without struggling with the after-effects.
Did You Know?
Our genes play a big role in how we respond to alcohol. Two key enzymes are involved in breaking down the alcohol we consume. A genetic deficiency in either of those enzymes can result in unpleasant side effects like red flush, nausea, vomiting, hangovers, or even severe toxicity! Learn more.
According to a 2021 report, the total wine sales in the United States in 2021 was $78.4 billion.
This number is only projected to increase in the coming years.
Multiple studies suggest that drinking moderate amounts of wine may help decrease the overall mortality rate, rate of cardiovascular diseases, and premature aging.
Red wine, especially, has higher amounts of antioxidants, essential vitamins, and minerals.
Unfortunately, not all people react well to red wine.
In some, consuming even small amounts of red wine can lead to headaches.
Red wine contains high amounts of certain polyphenols (pigments naturally found in plant-based foods) like tannin and quercetin.
Alcohol is also a rich source of histamines, chemicals that cause allergic symptoms in the body.
For a while now, researchers have been blaming histamines for causing headaches.
Histamine affects the hypothalamic activity in the brain, triggering migraines or contributing to their severity.
However, people who developed headaches after consuming red wine were usually fine with other types of alcohol.
So, the interest has now turned to the polyphenols in red wine.
Once you consume alcohol, the enzyme alcohol dehydrogenase (ADH) in the liver breaks down alcohol into acetaldehyde and other compounds.
Now, another enzyme, aldehyde dehydrogenase (ALDH), rapidly converts acetaldehyde into acetate.
Acetaldehyde is an active metabolite affecting the body and brain, causing various toxic, behavioral, and pharmacological effects.
Recent studies suggest that quercetin may affect the functioning of the aldehyde dehydrogenase 2 (ALDH2) protein.
Quercetin can slow the conversion of acetaldehyde into acetate and, as a result, increase acetaldehyde levels in the body.
One of the side effects of high acetaldehyde levels could be headaches.
A 2023 study published in the open-access Scientific Reports journal proposed a new hypothesis on why red wine causes headaches in certain individuals.
This was not a human-subject testing study.
The researchers picked up chosen samples of red wine for analysis.
HPLC-grade phenolics were procured from Lifescience and pharmaceutical companies in the United States.
The researchers also procured Human recombinant ALDH2 enzyme and other reagents for the study.
The researchers used QuantiChrom™ aldehyde dehydrogenase inhibitor screening kits to measure how different phenolic compounds inhibited ALDH2.
This kit converted acetaldehyde in the red wine into acetic acid and nicotinamide adenine dinucleotide (NADH).
The NADH interacted with a formazan agent, creating a colored substance.
The amount of colored substance absorbed was directly proportional to the enzyme activity, helping researchers understand the relationship between quercetin and the rate of ALDH2 inhibition.
The study observed the effects of different wine phenolics on the rate of ALDH2 inhibition.
The following were the results observed.
| S.no. | Compounds (20 μM) | ALDH2 inhibition (%) |
| 1 | Quercetin glucuronide | 78.69 ± 1.21 |
| 2 | Quercetin | 27.69 ± 0.61 |
| 3 | Tamarixetin | 25.83 ± 1.31 |
| 4 | Quercetin dihydrate | 25.71 ± 2.19 |
| 5 | Myricetin | 21.78 ± 1.56 |
| 6 | Quercetin-3-rhamnoside | 21.46 ± 1.90 |
| 7 | Quercetin galactoside | 20.61 ± 0.79 |
| 8 | Quercetin-7-rhamnoside | 19.58 ± 0.32d |
| 9 | Rutin | 18.53 ± 0.06 |
| 10 | Quercetin glucoside | 17.56 ± 1.84 |
| 11 | Kaempferol | 15.62 ± 0.78 |
| 12 | Catechin | 14.77 ± 0.39 |
| 13 | Epicatechin | 0.34 ± 0.12 |
According to the study, quercetin glucuronide, one of quercetin’s liver metabolites, showed the highest levels of ALDH2 inhibition.
The lowest inhibition was by epicatechin, a flavanol that belonged to the catechin family.
The primary limitation of the study was that it wasn’t human-tested since the study used a standard red wine sample for analysis.
However, there are different kinds of red wines in the world, each with varied quercetin levels. A larger sample could have led to more accurate results.
In human test subjects, specific gene polymorphisms could also affect acetaldehyde metabolism, which wasn’t considered in this study.
This is still a hypothesis, and human studies in the future may be able to verify this more precisely.
Hand-picked Article For You: Could You Have A Wine Allergy?
Thanks to genetic abnormalities, some people’s bodies may be unable to break down acetaldehyde effectively.
This can result in acetaldehyde buildup over time. Red wine contains much higher levels of quercetin.
As a result, drinking even small quantities of red wine can lead to excess acetaldehyde accumulation, leading to headaches.
For instance, studies report that 40% of Asians are born with a dysfunctional gene that does not produce enough ALDH enzyme to convert acetaldehyde into acetate.
In those consuming red wine in excess, quercetin may lead to severe ALDH2 inhibition over time, causing excess acetaldehyde circulation and headaches.
People with existing migraines may also be more susceptible to headaches when consuming red wine.
https://pubmed.ncbi.nlm.nih.gov/10940346/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10218803/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10218803/
https://pubmed.ncbi.nlm.nih.gov/37985790/#
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10662156/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6527032/#
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6527032/
https://www.ucdavis.edu/health/news/why-do-some-people-get-headaches-drinking-red-wine
https://www.nature.com/articles/s41598-023-46203-y
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4821937/
While a skin rash is common and probably affects millions, when accompanied by severe and prolonged muscle weakness, it could be a cause for concern. Dermatomyositis is an inflammatory condition that causes a distinctive skin rash accompanied by chronic muscle inflammation and weakness. Amyopathic dermatomyositis (ADM) is a subtype of this condition, where the muscle weakness is absent or barely present. Genetic testing is a useful tool in diagnosing conditions, understanding the cause better, and potentially pave the way to personalized treatments and better management. This article explores whether those suffering from ADM can benefit from genetic testing.
Did You Know?
The DNA data from your genetic ancestry test can be used to learn important things about your health, from your risk for heart disease and stroke to food intolerances and sleep disorders. You can upload your DNA data to learn 1,500+ things about your health. Learn more.
Genetic testing analyzes a person's DNA to find gene changes (mutations) that may impact their health.
It tells us about the risk of certain diseases, how someone might respond to treatments or the outlook for their condition.
It also helps understand how children inherit diseases or traits from their biological parents.
For example, it can diagnose diseases caused by a change in a single gene, such as cystic fibrosis (CF).
The key point is that while genetic testing is most definitive for simple single-gene diseases, it can still be useful for decoding complex conditions like ADM, which are a result of changes in several genes.
ADM is a subtype of dermatomyositis (DM) that falls under the category of IIM.
IIMs are rare autoimmune diseases that cause inflammation and damage muscle and other body systems.
DM typically involves both skin rashes and muscle weakness due to inflammation.
ADM is a variation that only affects the skin, causing a distinctive rash without signs of muscle inflammation or weakness.
ADM reveals its unique identity through several characteristics and symptoms that distinguish it from other types of myositis, such as:
Characteristics of ADM
Symptoms of ADM
Violaceous erythema
Macular rash
Papules
Gottron's papules
Gottron's sign
Shawl sign
V-sign
Scalp inflammation
Thinning of the hair
In addition, some patients with ADM may also experience other symptoms, such as:

The exact causes of ADM are unknown. But, it is believed to be an autoimmune disease, where the immune system wrongly attacks healthy cells and tissues, causing inflammation and damage.
Factors like infections, medications, hormones, stress, or genetics might trigger this immune system malfunction.
ADM doesn't follow a straightforward Mendelian inheritance pattern, meaning that a single gene mutation does not result in its inheritance from parent to child.
Instead, ADM is likely influenced by multiple genes interacting with each other and environmental factors.
These genes may impact how the immune system functions or responds to certain Stimuli.
Genetic testing isn't currently the usual practice in clinics for ADM. However, ongoing research suggests that genetic testing may be helpful in the future for:
Understanding the root causes of ADM can be significantly helped by genetic testing.
Identifying genetic risk factors and dysregulated gene expression provides insights into disease mechanisms.
Risk factors are variations in DNA that increase or decrease a person's likelihood of developing a disease.
Dysregulated gene expression is when genes are turned on or off at inappropriate times or levels.
Genetic testing can help identify genetic risk factors and dysregulated gene expression by analyzing different DNA samples from patients with ADM.
These samples may include blood cells (such as white blood cells), skin cells (such as skin biopsies), or muscle cells (such as muscle biopsies).
According to the study, several genetic risk factors and dysregulated gene expression patterns are associated with ADM.
These findings suggest that multiple genes and pathways are involved in the development of the disease.
Some of the key results from the study include:
Genetic testing offers several potential benefits for those at risk of or living with ADM.
It can confirm or eliminate an ADM diagnosis when symptoms are unclear.
Identifying disease-related genes also provides insight into one's prognosis and disease course.
This helps guide treatment plans to improve outcomes and reduce treatment toxicity.
Additionally, testing at-risk relatives allows early screening and counseling to delay or prevent ADM altogether.
Overall, genetic testing helps patients and clinicians understand, manage, and reduce the burden of this complex disease.
Personalized treatments for complex conditions like ADM are crucial to achieve maximum results and minimize potential side effects.
Treatments may involve:
Precision medicine utilizes an individual's genetic, biomarker, and environmental data to develop personalized treatment and prevention strategies. This approach is particularly promising for ADM.
Genetic markers are DNA variations that identify individuals at risk for ADM.
Studies have identified several genetic markers associated with ADM, including variations in HLA-DRB1 and HLA-DQB1.
These genetic markers can help predict the likelihood of developing ADM and may also help guide treatment decisions.
Recent multi-omics research has significantly advanced our understanding of rare autoimmune diseases, particularly focusing on ADM within the broader spectrum of IIM.
IIM, including subtypes like DM and polymyositis (PM), are complex conditions characterized by muscle weakness and elevated muscle enzymes.
These studies use multi-omics data (genomics, transcriptomics, epigenetics, proteomics, and autoantibodies) to understand the complex mechanisms of DM/PM.
Integrating these multi-omics data provides valuable insights into ADM's underlying immune and nonimmune factors, where muscle inflammation is absent.
This comprehensive approach helps identify biomarkers and therapeutic targets, facilitating rapid and accurate diagnosis of rare conditions like ADM.
Advances in high-throughput technologies and systems biology help us understand the details of how genes and molecules work together.
This understanding guides the creation of specific treatments and tools for diagnosing rare autoimmune diseases.
Pharmacogenomics is a rising method in precision medicine, aiming to customize drug selection and dosage based on a patient's genetic characteristics.
Although international scientific groups have issued guidelines, the integration of pharmacogenomics into clinical practice is limited. Ongoing global efforts are working to overcome these challenges.
However, the current established pharmacogenomic markers can only explain a small part of the differences seen in how patients respond to treatment.
New research explores the role of immune system genetics and rare genetic variations in drug metabolism to enhance our understanding.
These advancements are vital to customizing treatments for individuals with ADM, considering their unique genetic makeup for more effective and safer outcomes.
In parallel, studies examined standard treatments for various DM types, including clinically amyopathic DM (CADM), DM with lung issues, and classic DM (CDM).
Results indicate that many patients with DM and lung problems might not respond well to the usual medications.
For classic DM, where oral glucocorticoids are common, researchers are looking into other treatments like methotrexate and calcineurin inhibitors.
Additionally, they are working on new treatments that target cytokines or cell populations assumed to be the disease's origin.
Amyopathic dermatomyositis is a subtype of dermatomyositis that affects only the skin and not the muscles.
Genetic testing is not yet standard practice for ADM, but holds potential benefits for future use.
It could help diagnose at-risk individuals, predict disease progression, and customize treatment decisions based on genetic makeup.
Understanding the root causes of ADM through genetic testing offers valuable insights, identifying genetic risk factors and dysregulated gene expression.
These findings contribute to personalized treatment approaches for achieving effective and safe outcomes.
The integration of multi-omics data and advancements in pharmacogenomics further enhance the understanding and ability to develop treatments for individuals with ADM.
https://www.mayoclinic.org/tests-procedures/genetic-testing/about/pac-20384827
https://www.mayoclinic.org/diseases-conditions/cystic-fibrosis/symptoms-causes/syc-20353700
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10425161/
https://www.mayoclinic.org/diseases-conditions/dermatomyositis/symptoms-causes/syc-20353188
https://www.ncbi.nlm.nih.gov/books/NBK558917/
https://pubmed.ncbi.nlm.nih.gov/14689822/
https://nij.ojp.gov/topics/articles/dna-evidence-basics-types-samples-suitable-dna-testing
https://medlineplus.gov/lab-tests/white-blood-count-wbc/
https://medlineplus.gov/lab-tests/skin-biopsy/
https://www.healthline.com/health/muscle-biopsy
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7522761/
https://medlineplus.gov/genetics/understanding/testing/benefits/
https://pubmed.ncbi.nlm.nih.gov/29106035/
https://www.sciencedirect.com/science/article/abs/pii/S1568997217302045