Did you know that hemophilia is a rare genetic disorder that affects approximately 1 in 10,000 people worldwide? If you're a woman or assigned female at birth, you may not even know you're a carrier until you have a son with hemophilia, as it's passed down through the X chromosome. In this article, we'll explore the inheritance patterns of hemophilia and how you can determine if you're a carrier.
Hemophilia is a rare genetic disorder that affects the body's ability to form blood clots, which are necessary to stop bleeding after an injury.
People with hemophilia have a deficiency or dysfunction of specific proteins in their blood called clotting factors, which can cause prolonged bleeding and slow or incomplete healing.
Uncontrolled bleeding into the joints, muscles, brain, or other internal organs can result in serious complications.
Severe forms of hemophilia can result in spontaneous bleeding. However, milder conditions may not result in spontaneous bleeding and thus may be difficult to diagnose until surgery or a severe injury.
The two major types of hemophilia are:
Even though both types present with similar symptoms, they are caused by mutations in different genes.
Those with hemophilia have a deficiency of either factor VIII or factor IX, critical proteins required for blood clotting.
The F8 and F9 genes contain instructions to produce these two proteins.
Factor VIII and factor IX proteins work together to seal off blood vessels damaged during an injury to minimize blood loss.
Changes or variants in the F8 and F9 genes can result in the production of abnormal versions or insufficient levels of the coagulation proteins.
This can lead to problems in the blood clotting process and result in uncontrolled bleeding.
In severe hemophilia, the coagulation proteins are completely absent; in mild hemophilia, the activity of the proteins is reduced.
Acquired hemophilia is not a result of genetic variants. It occurs when the body’s immune system starts attacking factor VIII - an autoimmune disorder.
Hemophilia A and hemophilia B are inherited in an X-linked recessive pattern.
The F8 and F9 genes are located on the X chromosome, one of the sex chromosomes.
People assigned males at birth have one copy of the X chromosome and one copy of the Y chromosome.
Due to this, even one copy of the altered F8 or F9 gene can result in hemophilia in males.
People assigned females at birth have two copies of the X chromosome.
So even if they have one copy of the altered genes, the normal copies on the other X chromosome can compensate for the lowered activity.
Hence, in most cases (except for X-inactivation), they may not have hemophilia, even if they have a copy of the altered gene. Therefore they are “carriers” of hemophilia.
However, there’s a 50% chance they pass the altered gene copy to their offspring.
If the daughter receives it, she continues to be a carrier; if the son receives it, he will be affected by hemophilia.
Hemophilia is typically inherited from the mother.
Hemophilia-causing genes are located on the X chromosome, one of the two sex chromosomes.
If a female carrier has a son, there is a 50% chance that he will inherit the mutated gene and develop hemophilia and a 50% chance that he will inherit the normal gene and not have hemophilia.
If the female carrier has a daughter, there is a 50% chance that she will inherit the mutated gene and be a carrier and a 50% chance that she will inherit the normal gene and not be a carrier.
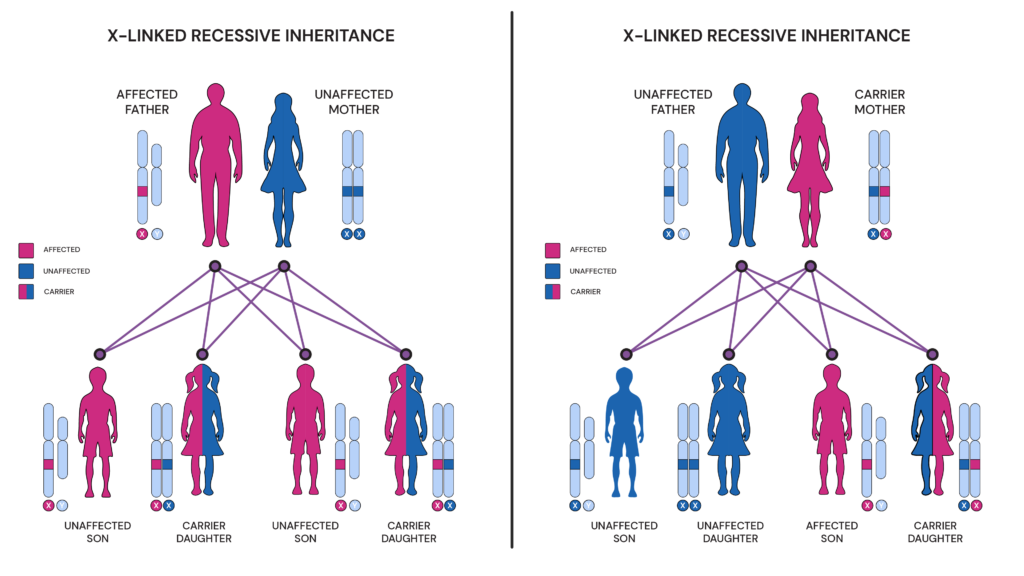
Conditions inherited in an X-linked recessive manner more commonly affect males than females since males only have on the X chromosome.
A daughter will get affected only when an affected father and a carrier mother each pass only the faulty gene copy to the daughter.
Being a carrier of hemophilia means that a person has a mutated hemophilia gene on one of their X chromosomes but not on the other.
As a result, carriers typically do not experience symptoms of hemophilia themselves.
However, they can pass the mutated gene on to their children.
Female carriers have a 50% chance of passing the mutated gene to each of their children, regardless of their gender.
Since they can pass either their normal X chromosome or their mutated X chromosome to their offspring.
It is important for carriers to be aware of their status, as they may have a higher risk of having a child with hemophilia.
Carriers can be identified through genetic testing, which can detect the presence of the hemophilia gene mutation in their DNA.
Genetic counseling may also be recommended for carriers and their families to help them understand the risks associated with hemophilia inheritance and to make informed decisions about family planning and medical management.
A genetic test analyzes a small sample of your blood or saliva to look for changes in the hemophilia genes.
Different types of genetic tests can be used to diagnose hemophilia carrier status.
One common method is called DNA sequencing. This involves reading the entire genetic code of the hemophilia genes to detect any mutations.
Genetic testing can be done before or during pregnancy to determine the risk of having a child with hemophilia.
For example, suppose a woman knows she is a carrier of the hemophilia gene mutation. In that case, she may choose to undergo prenatal testing during pregnancy to determine whether the developing fetus has inherited the mutated gene.
This information can help the parents make decisions about medical management and family planning.
Hemophilia is caused by gene mutations that provide instructions for making proteins necessary for blood clotting. They are located on the X chromosome. As a result, hemophilia is more commonly inherited by males than females since males have only one X chromosome. Females are usually carriers of hemophilia and can pass the mutated gene on to their children. Genetic testing is a reliable way to determine carrier status and can be done before or during pregnancy. This can help parents make decisions about medical management and family planning. It is often recommended that genetic testing be done in the context of genetic counseling to help individuals and families understand the implications of the results.
Imagine a single vitamin that not only benefits your skin and immune system but also has the potential to prevent blood clots and reduce your risk of heart attack or stroke. Is Vitamin E the ultimate multitasking nutrient, or is its blood-thinning reputation another myth? Let’s find out!
Vitamin E is a fat-soluble nutrient found in oils and fats. It is an essential nutrient for the body.
It is also an antioxidant that reverses free radical damage in the body.
Vitamin E is vital for normal vision. It is essential for maintaining fertility.
Vitamin E helps in the uptake of vitamin K by helping form red blood cells in the body.
Since vitamin E is an antioxidant, it protects the body from free radical damage.
Free radicals are released due to exposure to tobacco smoke or radiation.
They can cause severe problems like cancer and heart disease.
Vitamin E deficiency is rare in adults.
Healthy people rarely show any symptoms of deficiency.
However, when a diet contains low amounts of vitamin E, a person might start showing symptoms.
Symptoms
Some common symptoms of vitamin E deficiency include
Causes
Vitamin E deficiency is usually not caused by a diet low in vitamin E content.
It is usually caused by conditions where fat is not digested or absorbed properly.
Risk Factors
Vitamin E deficiency usually occurs in people suffering from a disease where fat is not metabolized properly.
Such diseases are Crohn’s disease, cystic fibrosis, and certain genetic disorders like ataxia.
Vitamin E deficiency can increase the risk of cancer and heart disease.
Vitamin E toxicity is usually rare.
Adults can continue to take excess vitamin E without any apparent harm.
But too much vitamin E can increase the risk of excess bleeding.
It is especially pronounced in people who already take a blood thinner like warfarin.
Studies show that people already taking blood thinners should avoid too much vitamin E.
Although it is unclear how much vitamin E can cause toxicity, it is recommended not to take more than 400 IU per day.
High doses of vitamin E, around 1500 IU daily, can cause adverse effects, such as blood thinning.
Getting all your vitamin E from your diet is a good idea rather than taking vitamin E supplements.
Vitamin E toxicity is usually a result of taking excessive supplements.
It is because too much vitamin E can reduce blood clotting.
It might increase the risk of bleeding and make a person prone to cardiovascular disease and heart attacks.
Other symptoms of vitamin E toxicity include
If high doses of vitamin E are taken for a long time, a person might suffer a hemorrhagic stroke.
Excess vitamin E can have blood thinning effects.
Besides interfering with vitamin K metabolism, it can also inhibit platelet aggregation.
Excess vitamin E can cause fatal bleeding and hemorrhagic stroke.
Excess vitamin E, when taken as supplements, can result in blood thinning.
However, little evidence proves that this vitamin can be used instead of a blood thinner.
When taken as a part of the diet, vitamin E does not cause blood thinning.
But when taken as supplements, they can act as blood thinners.
300mg or more of vitamin E daily can interfere with blood thinners like aspirin and warfarin.
When blood moves too slowly through the blood vessels, it can cause a disorder called deep vein thrombosis.
In this disorder, blood clots can break away and reach your lungs, where they can get stuck in a blood vessel.
Some research shows vitamin E can prevent deadly blood clots in people, not on any medication, but this claim needs to be backed by more studies.
The amount of vitamin E that your body need depends on your age.
Adults and pregnant women need around 15mg of vitamin E daily.
Breastfeeding women need 19mg of vitamin E.
People who cannot metabolize fat may need more than the standard recommended levels of vitamin E.
The Food and Nutrition Board of the Institute of Medicine prescribes no more than 1500 IU of vitamin E daily.
For people deficient in vitamin E, usually, a dose of 400 IU to 800 IU is prescribed by doctors.
You should always consult your doctor before starting any supplements.
Foods naturally rich in fat usually contain vitamin E.
In addition, certain fishes, fruits, and vegetables also contain vitamin E.
Some common foods that are rich in vitamin E are:
Vitamin E is an essential nutrient for the body.
It helps in metabolism and reduces oxidative stress.
However, excess vitamin E can act as a blood thinner.
It can cause fatal bleeding and interfere with other blood-thinning medications such as aspirin and warfarin.
It is essential to consult your doctor before starting any supplements as they might interfere with any preexisting health conditions.
Are you among the many people who think milk is the ultimate source of calcium? Think again. Broccoli might give the milk a run for its money regarding calcium content.
Let’s dive in and find out which comes on top.
Calcium is one of the essential minerals for your body. It is common knowledge that calcium is important for bone and teeth health. But calcium also plays many other vital roles in the body. Let’s have a look at some:
Calcium can be found in a variety of foods, including:
Getting enough calcium through food is essential for maintaining strong bones and overall health, and incorporating a variety of calcium-rich foods into your diet can help ensure you're meeting your daily need
Both milk and broccoli are good sources of calcium
However, milk contains 155% more calcium than broccoli!
From 100 grams of milk, we get 120 mg of calcium; from 100 grams of broccoli, we get only 47 mg of calcium.
Calcium is a mineral with many vital roles in human health. While dairy products make excellent sources of this mineral, many other food sources can help you meet your calcium needs - many of them are plant-based as well!
At Xcode Life, we are committed to providing you with accurate, reliable, and high-quality genetic reports. To maintain this standard of excellence, we continuously review and update our products and services.
We would like to inform our valued customers that we have temporarily suspended the sale of our Carrier Status and Pro Athlete Reports. This decision has been made to carry out a comprehensive technical review and quality check, ensuring that our reports meet the highest industry standards.
As part of our commitment to excellence, our expert team is currently conducting an in-depth analysis of the Carrier Status and Pro Athlete Reports. This review will include:
Please note that, during this period, the Carrier Status and Pro Athlete Reports will also be excluded from our mega and premium report packs. We apologize for any inconvenience this may cause and assure you that we are working diligently to bring back these reports as soon as possible.
We understand the importance of timely and accurate genetic information, which is why our team is working diligently to complete the review process. We expect the Carrier Status and Pro Athlete Reports to be back on sale and included in our combo report packs within the next few weeks.
In the meantime, our other genetic reports and services remain available for purchase. We encourage you to explore our extensive range of products designed to help you better understand your genetics and optimize your health.
To stay updated on the progress of our Carrier Status and Pro Athlete Reports review and be the first to know when they are available again, we invite you to sign up for our newsletter or follow us on social media. We will also be posting regular updates on our website.
Thank you for your understanding and continued support. If you have any questions or concerns, please do not hesitate to reach out to our customer support team via the chat option. We are always here to help.
Sincerely,
The Xcode Life Team
Researchers have identified several genes associated with Parkinson’s disease.
In the sample report below, we've attempted to analyze some essential genes that increase the risk for Parkinson’s.
You can identify your genetic risk of Parkinson’s by using your 23andMe DNA data and placing an order for the Gene Health Report.
Alt text: Lewy Body Dementia and Parkinson’s - Xcode Life’s Parkinson’s Genetic Report
Parkinson’s disease is a brain disorder that causes uncontrollable and unintended movements like shaking, stiffness, and difficulty balancing and coordinating.
It is a neurodegenerative disorder due to the degeneration of dopamine-producing nerve cells (neurons).
Dopamine is a common brain chemical or neurotransmitter responsible for nerve signal transmission.
Parkinson’s affects one in every 500 people.
Most people who develop symptoms of Parkinson’s are usually over 50.
People assigned male at birth (MAB) are likelier to develop Parkinson’s than those assigned female at birth (FAB).
When the nerve cells in the basal ganglia (part of the brain that controls movement) are damaged, they produce less dopamine than usual.
Lesser than usual dopamine results in movement-related problems that are characteristic of Parkinson’s.
Though the mechanism behind Parkinson’s is fairly known, what causes the degeneration or death of the neurons is unknown.
People with Parkinson’s also lose nerve endings that produce another neurotransmitter called norepinephrine. This chemical controls functions like heart rate and blood pressure.
Lower than usual level of norepinephrine gives rise to other Parkinson’s symptoms like:
Common symptoms of Parkinson’s disease include:
The symptoms of Parkinson’s are different in people, and the rate at which they progress also differs among individuals.
While early symptoms of the condition are subtle, they aggravate as the disease progresses.
Family members are often the first to notice changes in people who develop symptoms of Parkinson’s.
Several types of Parkinson’s disease exist. The three most common ones are:
According to the Alzheimer’s Association, 50% to 80% of people with Parkinson’s disease will develop dementia.
Several brain cells of people with Parkinson’s contain unusual clumps of the protein alpha-synuclein. These cells are called Lewy bodies.
Researchers are still trying to understand the normal and abnormal functions of the alpha-synuclein protein and its effect on dementia.
Some existing research states that Lewdy bodies play a role in many conditions that cause dementia.
Lewy body dementia is a condition that occurs when Lewy bodies build up in the brain, eventually damaging the brain cells and causing dementia.
It is challenging to diagnose Lewy body dementia as its symptoms are easily confused with those of other brain disorders and psychiatric conditions.
Lewy body dementia (LBD) is of two types.
In both these types, the underlying changes occurring in the brain over time in people give rise to similar symptoms.
Cognitive symptoms develop more than a year after the movement symptoms like tremors and muscle stiffness set in.
PDD starts as a movement disorder with symptoms like slowed movements, shuffling walks, muscle stiffness, and tremors.
Cognitive symptoms of dementia and mood and behavioral changes may set in later.
It is important to note that not all individuals with Parkinson’s develop dementia, and it is difficult to predict who will.
Some older patients with Parkinson’s may develop some degree of dementia.
Cognitive symptoms in people with DLB develop within a year of the movement of symptoms.
People with DLB also show a decline in their thinking ability, making it look similar to Alzheimer’s.
However, they also develop movement issues and other symptoms of LBD with time.
Happy World Liver Day!
The liver is the largest organ in the body. It is also one of the busiest and most underrated organs. If it weren't for the liver, your body would be unable to distinguish between toxic and useful chemicals. Your liver helps detoxify your body and maintain healthy metabolic pathways.
Today, on World Liver Day, we help you recognize its immense significance in the body and how you can help protect its health.
Choline was declared an essential nutrient by the Institute of Medicine in 1998. Essential nutrients are compounds that the body cannot produce or produces in insufficient amounts and need to be supplemented through diet.
Choline is required for several important functions in the body, including the regulation of the muscular system, nervous system, and liver function. It also helps maintain an active metabolism.
Choline is a part of a type of fat called phospholipids, which are essential to protect the structural integrity of the cell membranes. It produces compounds that aid the transportation of lipids, thereby preventing their accumulation in the liver.
Choline is also needed to produce acetylcholine, which is a neurotransmitter. Neurotransmitters help transmit signals from the brain to the target cells.
Along with vitamin B9 and B12, choline is involved in the synthesis of DNA.
Small amounts of choline are produced in the liver, insufficient to meet daily requirements. This essential nutrient needs to be supplemented through diet. The requirements vary from person to person based on their age, genetic makeup, and various other factors.
The Institute of Medicine recommends a daily intake of 550 milligrams and 425 milligrams of choline for adult men and women, respectively.
Pregnant and breastfeeding women should increase their daily intake to 450 milligrams and 550 milligrams, respectively.
Choline deficiency is rare, but specific individuals are at a higher risk. A 2018 study shows men are at a higher risk for choline deficiency than women!
However, post-menopausal women are at a higher risk than pregnant women. Higher choline intake can help prevent birth anomalies like neural tube defects.
Other at-risk groups for choline deficiency include:
Choline deficiency can also increase the risk of developing certain health conditions like non-alcoholic fatty liver disease, obesity, hypertension, and liver damage.
A choline-rich diet is very effective in preventing choline deficiency. Eggs and organ meat such as chicken liver, salmon, and cod are good sources of choline.
Plant-based sources include vegetables like broccoli, and cauliflower, fruits like apples and tangerines, and vegetable-based oils like soybean oil. Soy lecithin is a food additive containing about 3-4% choline content.
Image: Dietary sources of choline
*DV - Daily Value
Source: National Institutes of Health
Specific genes also influence your choline requirements.
The PEMT gene is one such example. This gene contains instructions for making an enzyme that is involved in the production of choline.
Variants or changes in this gene affect choline levels in the body.
If you are at risk for choline deficiency, talk to your doctor. You might need to take choline supplements from a diet rich in choline.
A genetic test can help determine if you have any genetic variations affecting your choline levels.
Most genetic tests provide your DNA information as a text file known as the raw DNA data. This data may seem like Greek and Latin to you.
At Xcode Life can help you interpret this data. You must upload your raw data and order a nutrition report. Xcode Life then analyzes your raw data to provide comprehensive nutrition analysis, including information on your choline levels.