Glucagon-like peptide-1 agonist (GLP-1 agonist) is a class of drugs used in treating type II diabetes and helping with weight loss.
According to the American Diabetes Association, metformin remains the most preferred drug to treat type II diabetes.
However, in the case of metformin intolerance or if diabetes is combined with obesity, GLP-1 agonist drugs may help.
There are two categories of GLP-1 agonist drugs available in the market.
Drugs in this category include:
Drugs in this category include:
People with type 2 diabetes have lower levels of insulin secreted in the body.
As a result, glucose from the food is not broken down.
This leads to higher blood glucose levels.
GLP-1 agonist drugs imitate a naturally produced hormone in the body called glucagon-like peptide 1 (GLP-1).
This hormone may help improve insulin secretion in the pancreas.
Therefore, this drug can reduce blood sugar levels and control type 2 diabetes.
Recently, researchers have identified an added benefit of using GLP-1 agonist drugs - weight loss.
The GLP-1 hormone may help regulate hunger and appetite.
It helps in the following ways.
Studies show that this drug class helped people lose an average of 2.9 kg compared to people who did not take it.
According to experts, GLP-1 agonist drugs also help decrease the overall mortality rate in people with type 2 diabetes.
Post Food and Drug Administration’s (FDA) approval, the drug is prescribed for people with BMI > 30 or those with type 2 diabetes and BMI > 27.
Please note: GLP-1 agonists can only be used under the supervision of a qualified medical practitioner. Xcode Life doesn’t promote using GLP-1 or any other medication for weight loss.
Some of the common side effects of GLP-1 agonists are:
In rare cases, the patient’s body can form antibodies against GLP-1 analogs, leading to reduced efficacy.
Long-term use of these drugs may increase the risk of gastrointestinal issues.
Other rarer side effects of the drug include the following.
Doctors may prescribe GLP-1 agonist drugs for people with a BMI of more than 30 who can’t lose weight with lifestyle changes.
The drugs may also benefit those over a BMI of 27 and with type 2 diabetes.
The first oral GLP-1 agonist drug approved by the FDA for type 2 diabetes and weight loss is oral semaglutide. The drug was approved in 2019.
The following people are not recommended to take GLP-1 agonist drugs.
GLP-1 agonist drugs help suppress hunger and help people feel fuller for longer after a meal.
However, the drug needs to be backed by moderate exercise and dietary changes for it to work.
A molecule that binds to an enzyme and inhibits its activity is called an enzyme inhibitor.
Enzyme inhibitors have a vital role in all cells because of their target action.
COMT inhibitors are one of the most prominent enzyme inhibitors in Parkinson’s treatment.
Catechol-O-methyltransferase (COMT) inhibitors are a group of medications in the therapeutic approach to Parkinson’s treatment.
It inhibits the enzyme COMT, which methylates catecholamines such as epinephrine, dopamine, and norepinephrine.
Catecholamines are hormones responsible for modulating our stress responses.
COMT also methylates levodopa and carbidopa (a class of medications in Parkinson’s treatment) before entering the target site.
COMT inhibitors prevent this methylation and offer complete therapeutic benefits in treating Parkinson’s disease.
The depletion of the neurotransmitter dopamine in the brain is the major cause of Parkinson's disease.
The precursor to dopamine is provided by levodopa medication.
When the COMT enzyme degrades dopamine, COMT inhibitors prevent its action by working against the process.
It works by blocking the peripheral degradation of levodopa, enabling the drug to cross the blood-brain barrier.
This increases its effects by allowing more of it to enter the brain. Thereby increasing the bioavailability and half-life of levodopa.
The purpose of antiparkinson drugs is to extend the brain's absorption of dopamine through:
COMT inhibitors work best in combination with levodopa by blocking the drug's breakdown and prolonging its efficacy.
This saves people with Parkinson’s disease during the phase of motor fluctuations.
Motor fluctuations are caused when dopamine levels decrease in the brain. That’s when levodopa is taken, and the person functions well.
When the drug effect wears off, the person finds it difficult to move.
COMT inhibitors delay the body's ability to break down levodopa and maintain dopamine concentration even when the effect wears off.
A study reported that COMT inhibitors have potential antidepressant properties on chronic mild stress (CMS)-induced anhedonia in rats.
The findings indicate that selective, reversible COMT inhibitors have been used therapeutically to treat depression in addition to Parkinson's disease.
The most typical adverse effects of COMT inhibitors are as follows:
Humans have 23 pairs of chromosomes. Of these, 22 are called autosomes, and one pair in each cell is called the sex chromosome.
There are two sex chromosomes - the X and the Y.
People assigned females at birth (FAB) have two X chromosomes, whereas those assigned males at birth (MAB) have one X and one Y chromosome.
These sex chromosomes play many roles in the body, though they are primarily responsible for the development and functioning of the reproductive system in men and women.
Loss of the Y chromosome (LOY) is a genetic condition detected in blood samples of people assigned MAB.
LOY has been associated with several diseases, like cancer.
Though the primary function of the Y chromosome is the normal development of males, it has several roles beyond this.
A few decades ago, doctors began noticing that blood cells in older men were missing the Y chromosome.
The exact cause for this disappearing chromosome is unclear even today.
However, researchers suspect that men allow genetic mutations (abnormal changes in the genes) to accumulate, eventually leading to diseases like cancer and heart disease.
Loss of the Y chromosome is now believed to be a part of the normal aging process.
It is called a ‘mosaic’ LOY because the loss is observed only in a fraction of the cells.
Research states that LOY is part of the normal aging process in healthy men, and the number of cells affected increases with time.
A 2014 study reported that LOY caused an average 5.5 years decrease in the lifespan of men affected with the condition.
For this reason, LOY can be used as a biological marker and helps predict the development of male age-related diseases.
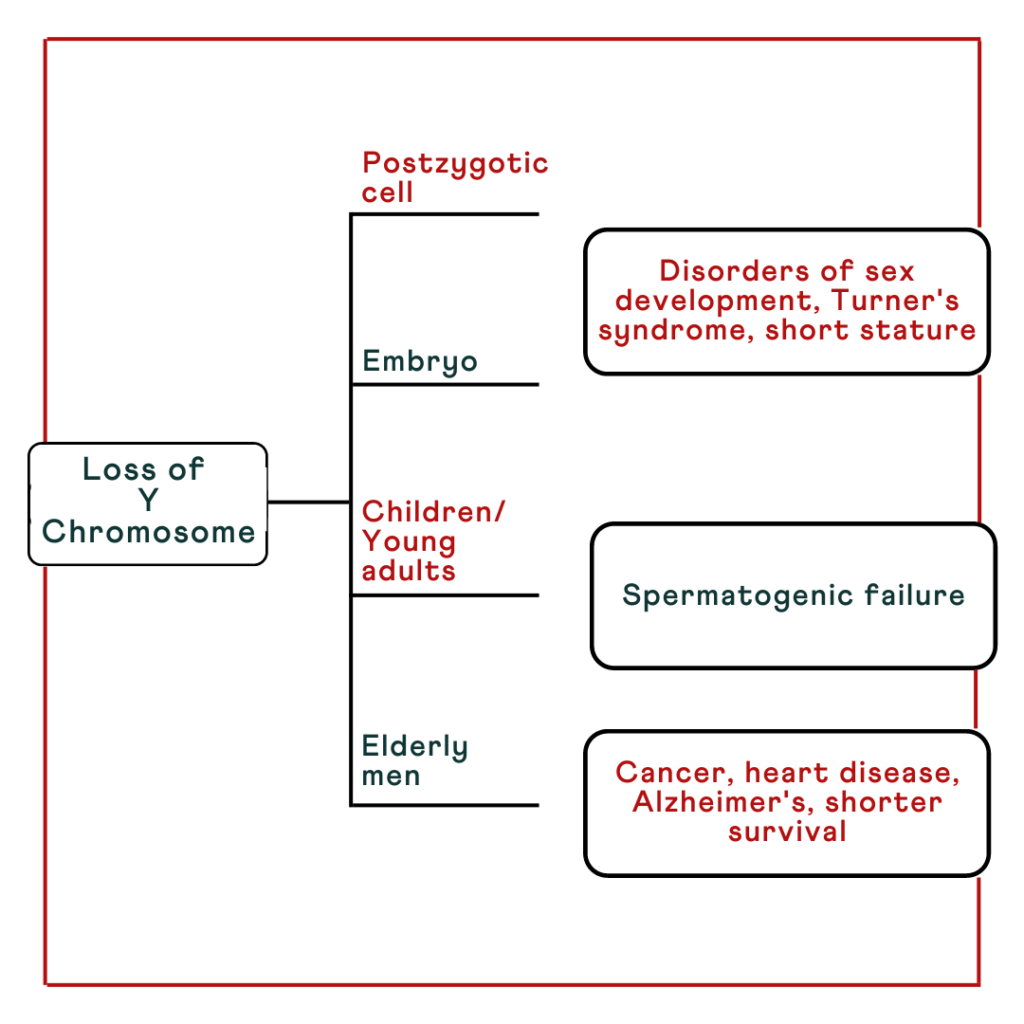
LOY has been associated with the development of cardiovascular diseases.
A study on male mice found that those who lost their Y chromosome had weaker hearts.
Researchers also noticed a build-up of fibrous connective tissues in the heart of mice with a missing Y chromosome.
This stiffening of heart muscles makes it difficult for the organ to pump blood effectively.
A similar study was conducted in humans, and it was found that men who had lost the Y chromosome from at least 40% of their white blood cells were 31% more likely to die from circulatory system disease than those with abundant Y chromosomes.
Apart from cardiovascular disease risk, loss of the Y chromosome also has other health implications, which include:
The medical and research community do not yet have a complete understanding of what exactly causes migraine. Certain activities, environmental exposure, and emotion can trigger a severe migraine attack. Having to deal with pain is not just debilitating but also leads to a loss of productivity. This begs the question - why migraine happens? Are migraines hereditary? Do certain genes cause migraine?
Researchers have identified several genes associated with migraine.
In the sample report below, we've attempted to analyze some important genes that increase the risk of migraine.
You can identify your genetic risk of migraine by using your 23andMe DNA data and placing an order for the Gene Health Report.
Genetics play a big role in migraine.
Certain genes associated with migraine explain up to 60% of the reason people get migraine headaches.
While they may not directly “cause” migraine, they make the person more sensitive to environmental and lifestyle triggers that can cause migraine.
There’s no single “migraine gene.”
Studies suggest that mutations in a group of genes can contribute to migraine headaches.
A study examining 8,319 individuals across 1,589 migraine families found more than 40 genetic regions associated with migraine.
The researchers found that these families had more genetic changes associated with migraine than the general population.
Certain characteristics may indicate a strong family history of migraines.
Some important genes studied in association with migraine include:
It has long been established that migraine has a significant genetic component.
Migraines do not have a clear inheritance pattern; however, more than half the people with migraine have at least one family member with the same condition.
Further, if one or both of your parents have migraines, you have a 50-75% chance of having them.
According to family and twin studies, a first-degree relative of a person with migraine without aura (MO) has a 2x increased risk of having MO and 1.4x increased risk of having migraine with aura (MA).
A first-degree relative of a person with MA has a 4x increased risk for the same condition but no increased risk for MO.
Familial hemiplegic migraine (FHM) is a type of migraine that runs in families.
FHM can result in severe migraine episodes, which can include fever, seizure, prolonged weakness, and, rarely, coma, and death.
20% of people with FHM may develop permanent difficulty coordinating movements, a condition called ataxia.
Some genes implicated in FHM are
The first three genes regulate the movement of ions across cells, which is important for signaling in the brain.
FHM is inherited in an autosomal dominant pattern.
What does this mean?
A biological parent with FHM has a 50% chance of passing it on to their child.
So, in most cases, an affected individual has at least one affected parent.
Except in rare cases, inheriting a single specific mutation does not result in migraine.
Most migraine headaches are caused due to a combination of genetic and environmental factors.
Knowing your genetic risk for migraine in advance can help manage triggers and plan effective management strategies.
Identifying specific gene variants helps in knowing the possible cause of migraine.
This, in turn, helps plan treatments that focus on that particular pathway.
Further, it can also give guidance to testing other family members.
Genes can explain 60% of the reasons behind migraine.
KCN18 and CKIdelta are two important genes associated with migraines. The former produces a protein that regulates ion transport in cells, and the latter influences circadian rhythms.
Mutations in these genes can increase the risk of migraine with aura.
Biological parents with migraines have a 50-75% chance of having a child with migraine in each pregnancy.
Familial hemiplegic migraine is a specific type of migraine that runs in the family and is inherited in an autosomal dominant pattern.
Genetic testing can help you understand your risk for migraine, avoid the triggers, plan effective management strategies, and opt for effective treatment.
Researchers have identified several genes associated with multiple sclerosis.
In the sample report below, we've attempted to analyze some important genes that increase the risk of multiple sclerosis.
You can identify your genetic risk of multiple sclerosis by using your 23andMe DNA data and placing an order for the Gene Health Report.
Multiple Sclerosis (MS) is an autoimmune condition where the immune system attacks the myelin sheath of the nerve cells in the Central Nervous System (CNS).
Myelin sheath is the outer covering of the nerve cells, allowing electrical impulses to transmit between the nerve cells.
When the myelin sheath gets damaged, the nerve cells in the CNS cannot pass on information.
MS can cause the following symptoms.
The signs of MS usually sets in between ages 20 and 40. Just like other autoimmune conditions, MS is more common in women than men.
A nationwide study in Denmark concludes that the female-to-male ratio of MS is 2.35:1.
The same study suggests that people in the northern latitudes are at higher risk for developing MS.
There are four types of MS identified.
The RRMS is the most common type, affecting more than 80% of patients.
While it is not easy to identify the exact cause of Multiple Sclerosis, experts agree that a combination of genetics and environmental factors play a role in increasing the risk.
That is why Multiple Sclerosis genetic testing is becoming popular in identifying one’s risk of developing the condition. We will discuss more of this in the coming sections.
Lack of Vitamin D
Some studies suggest that a lack of vitamin D could be associated with a slightly increased risk of developing MS. This could be why people in the northern hemisphere experience MS more.
Smoking
Smoking is one of the biggest preventable environmental causes that lead to MS. Smoking causes DNA-level changes in the body, leading to autoimmune conditions.
Dietary salt intake
In the recent past, there have been studies that relate high dietary salt intake with an increased risk of MS.
Salt may encourage the activity of a type of cell in the immune system called the pathogenic T-helper 17 (Th17).
These cells can stimulate the immune system and encourage the development of an autoimmune condition like MS.
Epstein-Barr Virus infection (EBV infection)
EBV infection is widespread in human beings and is mostly asymptomatic. About 95% of all adults experience this infection at least once in their lifetimes.
EBV infection during adolescence or adulthood may increase the risk of developing MS by over-activating the immune system.
Genetics play a role in causing MS. A study shows that the family recurrence rate of MS can be up to 15%.
Individuals with first-degree relatives with MS have a 3-5% chance of developing the condition themselves. This increases to up to 30% in the case of monozygotic twins.
While multiple genes can increase the risk of MS, an important one is HLA-DRB1 (major histocompatibility complex, class II, DR beta 1).
This gene produces a protein called the beta chain that plays a role in immune functioning. This protein combines with another protein called HLA-DR antigen-binding heterodimer and helps identify foreign particles in the body.
According to studies, the HLA DRB1*1501 variant of this gene is found more in people with MS, suggesting that it may contribute to the risk.
Multiple Sclerosis genetic testing is a way of understanding a person’s potential risk for developing MS in the future.
While this is not a diagnosis or a confirmed identification of the condition, genetic testing may prove beneficial in the following individuals.
In all these cases, Multiple Sclerosis genetic testing may help point to or rule out MS or similar conditions that affect the myelin sheath.
Multiple Sclerosis genetic testing is still a field that’s being researched.
You can choose to get yourself tested. However, the presence of the risk alleles may not 100% mean the person will develop the condition.
In the same way, some people’s tests may not show the risk variant, but they could develop the condition because of other factors.
Researchers have identified several genes associated with ulcerative colitis.
In the sample report below, we've attempted to analyze some important genes that increase the risk of ulcerative colitis.
You can identify your genetic risk of ulcerative colitis by using your 23andMe DNA data and placing an order for the Gene Health Report.
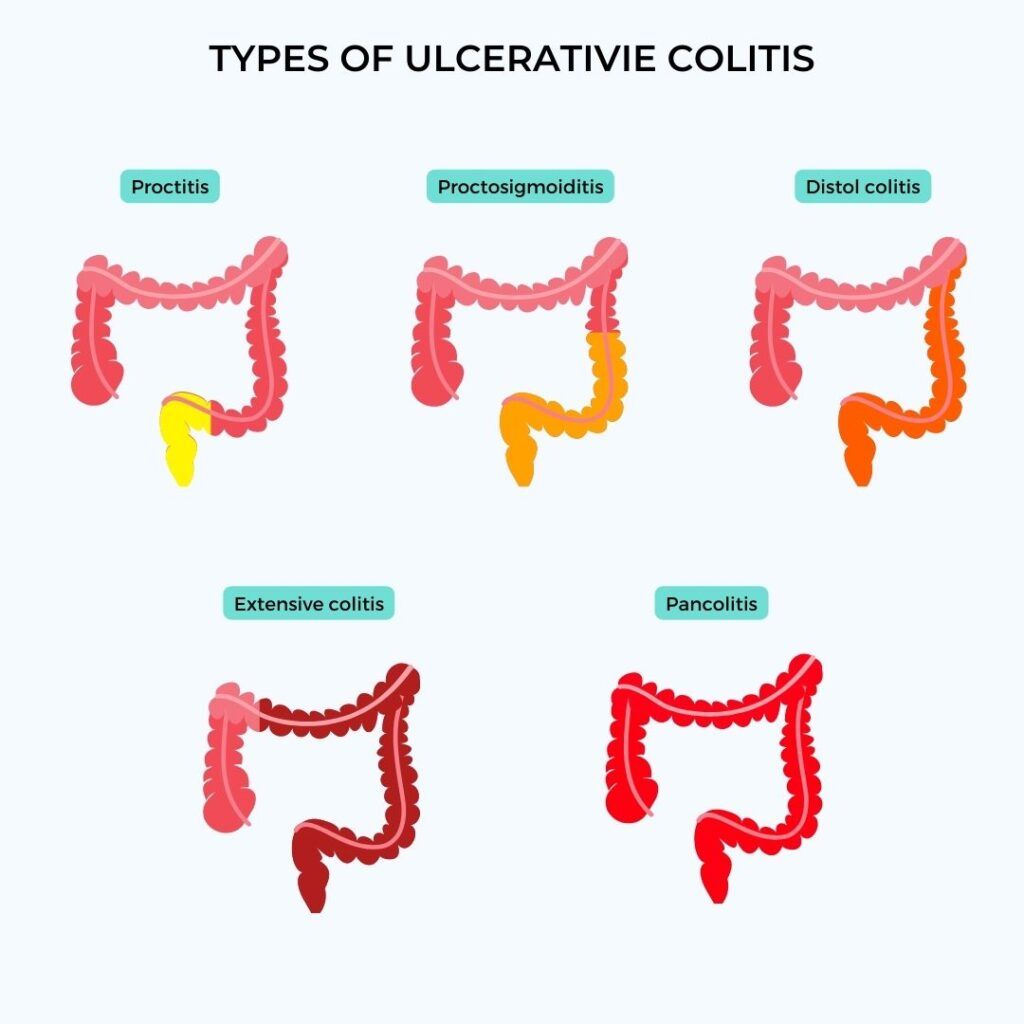
Ulcerative colitis is a chronic condition of the digestive system. It is characterized by abnormal inflammation of the inner layer of the colon and the rectum.
This inflammation in ulcerative colitis often results in ulcers in the large intestine.
It is said to be a type of inflammatory bowel disease (IBD) and is most common in North America and Western Europe.
Anyone can develop ulcerative colitis, but it is more common in people between 15 and 30 years of age.
People with ulcerative colitis experience flare-ups several times throughout their lifetime.
The exact cause of ulcerative colitis is unknown, but doctors and researchers believe the condition develops due to a complex interplay of several factors.
A few common causes of ulcerative colitis include:
Since ulcerative colitis does run in families, researchers suggest that some genes may increase an individual’s risk of developing this condition.
Abnormal immune system reactions may lead to inflammation of the large intestine and may be responsible for ulcerative colitis in some individuals.
The microbes that live in the digestive tract, including bacteria, viruses, and fungi, help digestion and constitute the gut microbiome.
Studies have found that a disruption or abnormal change in the gut microbiome can result in IBDs like ulcerative colitis.
A complex interplay between an individual’s environment and how their body reacts to it may play a role in the development of ulcerative colitis.
However, further research is underway to understand how people’s genes, immune system, and gut microbiome interact with the environment to cause ulcerative colitis.
The symptoms of ulcerative colitis can vary among individuals.
A few common symptoms include:
The severity of the symptoms is directly related to the degree of inflammation of the rectum and the colon.
In some individuals, the severity of the inflammation may interfere with their regular routines and lives.
Ulcerative colitis is known to flare up and go into remission several times during an individual’s lifetime.
Common symptoms of a flare-up include:
Recent studies have identified several genes that may be linked to ulcerative colitis, but their exact roles still need to be understood.
Ulcerative colitis is thought to occur due to changes in the protective lining of the intestine or by an abnormal immune reaction, both of which occur due to genetic variations.
So, few genes involved are associated with the protective function of the intestinal lining, while others protect the body’s tissues from bacterial toxins.
A few abnormal genetic changes (mutations) may also cause the immune system to malfunction, resulting in chronic inflammation and ulcerative colitis.
Though there is no single ulcerative colitis gene, a few that have been associated with this condition include;
Of these, two genes that are of particular interest are IL23R and IRF5.
This gene provides instructions for making a protein called interleukin 23 receptor (IL-23).
This protein is present on the outer surface of immune system cells, including the T cells, and participates in defending the body against foreign substances.
The IL23R protein is also responsible for inflammatory reactions and is said to play a role in the development of ulcerative colitis.
Interferon regulatory factor 5 (IRF5) gives instructions for making the IRF5 protein.
This protein regulates proteins called cytokines, which participate in inflammatory immune reactions.
This gene may have a role to play in the development of ulcerative colitis.
The inheritance pattern of ulcerative colitis is unknown as many genetic and environmental factors are involved in its development.
However, having a family member, especially first-degree relatives, increases one’s risk of developing the condition.
Many factors can increase the risk of developing ulcerative colitis or cause a flare-up in people with the condition.
While factors like age and genes cannot be modified, lifestyle changes can help control and prevent the condition.
Here are a few common risk factors for ulcerative colitis:
Other factors associated with ulcerative colitis include a sedentary lifestyle and smoking.
Having a risk factor does not mean one will develop the condition.