Beyond vitamin C serums and retinoid creams, we are now stepping into another realm of skincare: LED light therapies. If you are someone who keeps up with skincare trends, you’ll probably already know that LED masks have quickly become celeb faves. Among the different color light therapies, red and blue are the ones commonly used. So, how do these work? Let’s dive right into the red light vs blue light therapy battle and see which one may suit your needs.
LED light therapy is a new-age technology used to treat various skin conditions.
LED light therapies come in different types, with red and blue light therapy being the most common.
LED Light therapy uses low-level light in different wavelengths and colors.
Each color targets skin issues at different depths.
For instance, blue light treats the uppermost layer of the skin, while red light travels deeper into the skin.
LED light therapy is helpful in treating many health conditions, such as:
LED light therapy has been found to be helpful in the treatment of superficial basal cell carcinoma in some people.
Depending upon the type of condition and the depth of penetration required to treat it, doctors choose an appropriate wavelength of light.
The wavelength of light corresponds to visible colors.
Based on this, there are different types of LED light therapies:
Red and blue LED light therapy are the most commonly used.
Collagen is responsible for younger-looking skin that reduces with age.
During treatment, most specialists use a combination of LED light therapies.

Red light therapy is a type of phototherapy that uses the red light spectrum.
Red light therapy promotes cell response in the body and increases cellular turnover.
It also boosts collagen production.
Red light is said to penetrate the mitochondria in the cells, increasing their function.
As a result, cell energy increases, bringing about cell rejuvenation and damage repair.
Red light therapy stimulates the body’s natural healing process, making skin cells healthier.
Red light therapy has been used in dermatology for years to treat many skin conditions.
It is effective in treating
Red light therapy also promotes wound healing.
Since red light therapy promotes collagen production, it may help reduce fine lines, wrinkles, and other signs of aging (dark spots, hyperpigmentation, etc.)
Blue light therapy uses the purple-blue light from the spectrum to treat skin conditions.
Blue light LED is used to treat superficial skin conditions as it does not penetrate the deeper layers.
It is usually combined with other skin treatments like microdermabrasion and chemical peels for increased effectiveness.
Blue light therapy is sought after as it can kill acne-causing bacteria P. acnes, which live on the skin's surface.
Blue light therapy helps treat
(tabulate the differences on what it treats, how it works, benefits, cons, costs, etc.
| Red Light Therapy | Blue Light Therapy | |
| Depth | Longer wavelength of light, therefore, reaches deeper layers of the skin Between 630 to 670 nanometers (nm) | Shortest wavelength, therefore, treats superficial skin conditions Between 400-495 nanometers (nm) |
| What does it treat? | Improves skin tone and texture Reduces skin irritation and redness Fades scars Minimizes pores | Treats and prevents acne Reduces inflammation Treats and minimizes skin discoloration Minimizes pores |
| How it works | Boosts blood flow Stimulates collagen production Increases cell energy, stimulating cell rejuvenation | Reduces inflammation in the keratinocytes (common in the outer layers of the skin) Kills acne-causing P.acnes |
| Benefits | Best to rejuvenate aging skin Has a wide range of applications | Best for treatment and prevention of acne |
| Drawbacks | Some people may develop burns, blisters, or lesions if the red light therapy device is used for longer than 30 minutes or if the device is damaged. | It is currently being studied to reduce acne breakouts. Overexposure may contribute to accelerated skin aging, uneven pigmentation, and melasma. |
| Cost | $25-$175 per session At-home device cost: $300-$3,000 | $400-$1,000 |
Ted and blue light therapies have their benefits and drawbacks.
Both these therapies have similar efficacies in treating mild-to-moderate acne vulgaris.
Red light therapy has advantages, with fewer adverse reactions compared to blue light.
Which is better? Well, combining red and blue light therapies can produce the best results.
Most dermatologists will use a combination of red and blue light therapy.
While blue light can take care of the conditions on the outermost layer of the skin, red light penetrates deeper into the skin to reduce oil or sebum production.
So, combining both red and blue light therapies is more effective in treating skin conditions.
Red and blue light therapies are safe and relatively risk-free. However, some people may experience a few side effects, such as
Now and then, social media comes up with hacks and tricks claimed to be "life-changing." Usually, there is no credible research to back up such wild claims. Worse, sometimes, these hacks end up harming people more than doing anything beneficial. A recent hack is a mocktail that claims to help you sleep better, made famous on TikTok. Called the Sleepy Girl Mocktail, it has garnered millions of views on this platform, and users claim this magic potion helps you sleep better. While the ingredients seem promising, experts are skeptical. So, what is the truth? Does the Sleepy Girl Mocktail really help you sleep better?
Did You Know?
Genetics is one of the biggest influencers of sleep. Certain genes affect the sleep cycle, time taken to fall asleep, tendency to nap risk of snoring or apnea, sleep duration, deep sleep, and much more. It is now possible to understand the genetic intricacies of sleep and improve your sleep health for good using your existing ancestry genetic test DNA data.
Learn more.
The Sleepy Girl Mocktail is the newest sleep aid that is doing the rounds on TikTok.
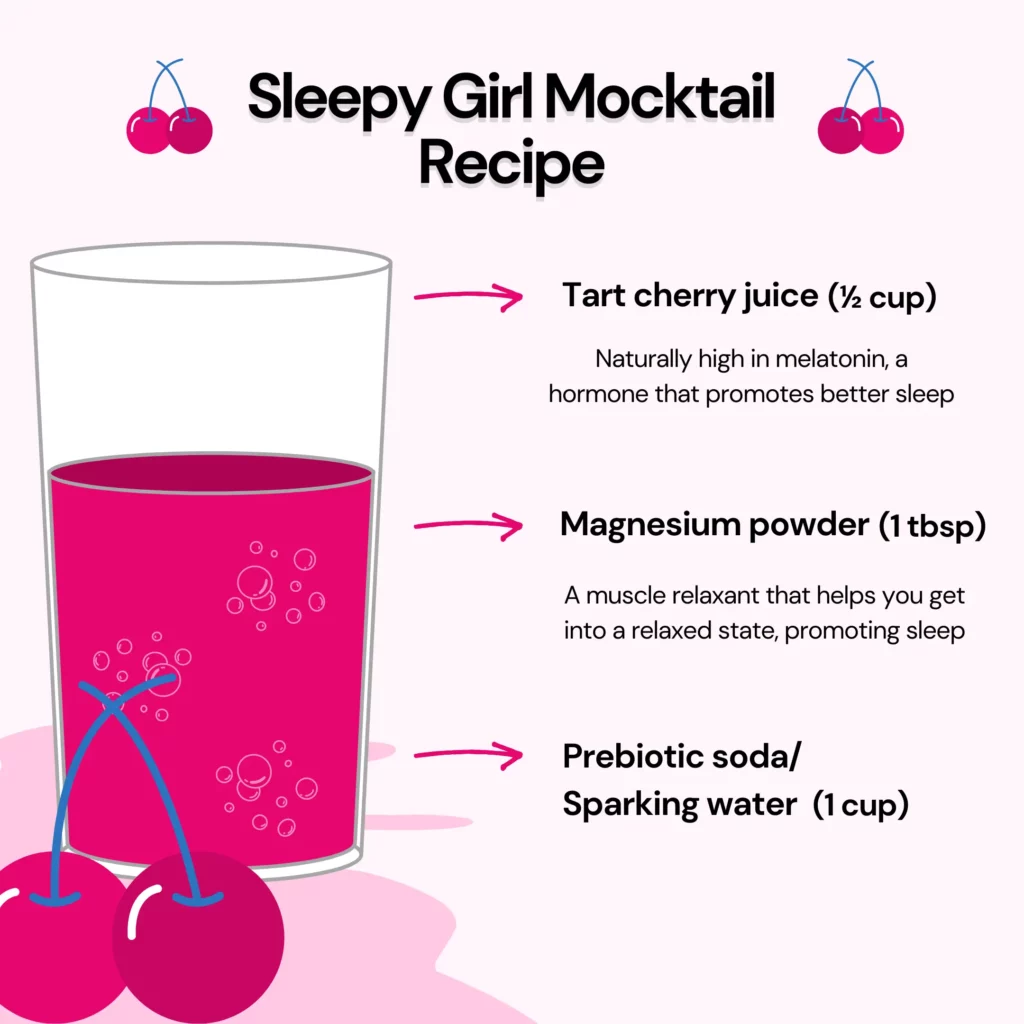
It's a drink made from magnesium powder, tart cherry juice, and soda that users say lets them sleep better.
The recipe was first posted on TikTok by Gracie Norton in 2023.
Since then, it has gained 58 million views on that platform.
The two main ingredients in the Sleepy Girl Mocktail, tart cherry juice and magnesium powder, have been shown to promote sleep.
The Sleepy Girl Mocktail might be beneficial for sleep.
Both magnesium and tart cherry juice, the main ingredients of the Sleepy Girl Mocktail, have some benefits for good sleep.
However, more evidence is required to support the claim.
Another Interesting Read For You: The Top 3 Methods To Fall Asleep Faster
The ingredients in the Sleepy Girl Mocktail may help you sleep better.
The magnesium in this mocktail might help counter deficiencies and increase the production of GABA, a neurotransmitter that helps keep anxiety and stress at bay.
The melatonin in tart cherry juice can help induce sleep.
However, experts are not sold on the idea of this mocktail being an effective sleep aid.
In fact, some amount of the placebo effect may play into this.
If you regularly make this mocktail and consume it before bedtime, your brain may be tricked into making an association between both.
So whenever you make this mocktail, your brain starts sending signals to the, you signal to your body that it's time to fall asleep.
It becomes a part of your bedtime routine that relaxes and helps you unwind.
This eventually leads to sound sleep rather than the drink itself.
Here's the recipe for the "Sleepy Girl Mocktail.":
Despite its apparent health benefits, doctors and experts don't recommend relying solely on the Sleepy Girl Mocktail for sleep.
This is because numerous factors like diet, physical activity, stress levels, hydration, etc. can affect sleep.
While the magnesium and tart cherry juice might help some of these, not all can be solved with this mocktail.
Further, there is little only scientific evidence to back the claims being made on social media about this miracle concoction.
Pairing it with other good sleep habits, such as staying away from devices just before sleep or creating a calm environment in the bedroom, can help you sleep better.
Although the effectiveness of the Sleepy Girl Mocktail is questionable, the concoction is unlikely to cause any harm.
However, that does not mean you can consume large quantities of it without any side effects.
There are no serious health risks associated with the Sleepy Girl Mocktail.
So it can be safe to use everyday.
However, if you have a health condition that makes consuming either magnesium or tart cherry juice risky, we advise consulting your doctor first.
It's a good idea to drink the Sleepy Girl Mocktail 2 hours before going to bed.
Remember to pair it with a bedtime routine to increase its effectiveness.
Besides the Sleepy Girl Mocktail, here are a few healthy habits to follow if you are trying to get better sleep:
The Sleepy Girl Mocktail is a concoction of tart cherry juice and magnesium powder that helps you sleep better.
Magnesium is a muscle relaxant and might help promote sleep.
Tart cherry juice contains small amounts of melatonin, a hormone that regulates the body's sleep cycle.
However, experts have differing views that this mocktail alone might solve your sleep problems.
They recommend pairing it with other good sleep habits.
If you have a medical condition that restricts you from consuming either magnesium or tart cherry juice, make sure to consult your doctor before drinking this mocktail.
https://health.clevelandclinic.org/sleepy-girl-mocktail
https://pubmed.ncbi.nlm.nih.gov/28901958/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4303399/
An astonishing 90% of adults in the United States have experienced at least one cavity in their lifetime. While factors such as oral hygiene practices and consumption of sugary beverages are commonly blamed, the roots of dental issues often delve much deeper. Research indicates that a variety of dental conditions, including cavities, tooth decay, and misaligned teeth, may have familial ties. This suggests that inheriting "bad teeth genes" from your parents could significantly elevate your susceptibility to a range of dental problems.
Humans inherit 50% of their DNA from their biological mothers and the other 50% from their biological fathers.
That’s why we all share features with our biological parents - blue eyes, curly hair, food preferences, etc.
In the same way, we also may share disease risk - how likely we are to develop heart disease or diabetes - though it’s not as straightforward.
Even dental issues fall into this pattern.
Here are some oral health attributes that may be inherited:
Crooked teeth or misaligned teeth are conditions that affect many children and adults.
In severe cases, it can cause problems with speech.
It is usually corrected using braces.
You can have crooked teeth due to genetic and environmental factors.
Teeth alignment depends on the number and size of teeth, size of jaw, and occlusion (how the teeth come together when we chew).
Your genes determine all these factors.
However, some other factors, like sucking your thumb and thrusting your tongue towards your teeth, also result in crooked teeth.
Interestingly, these behaviors, too, have genetic predispositions.
So, if you have crooked teeth, chances are that it runs in your family.
Periodontitis or gum inflammation is one of the most common types of periodontal disease.
There are two types of periodontitis: chronic periodontitis (CP) and aggressive periodontitis (AgP).
Studies have found that AgP is more likely to be genetic than CP.
Another study has shown that a gene named FAM5C is most likely to contribute to AgP, especially in older adults.
Cavities are usually caused by poor oral hygiene, smoking, and eating sugary and starchy foods.
However, you might become more susceptible to cavities if it runs in your family.
Less saliva production is a genetic risk factor for developing cavities.
A thin or weak enamel might also make you prone to developing cavities.
Tooth decay is caused by the formation of dental plaque, a sticky, bacteria-filled film that forms on the tooth.
This plaque changes into a hard substance called dental calculus when you don't brush your teeth.
Sugary foods are the most common cause of tooth decay.
However, genes might make you more susceptible to tooth decay.
You might be prone to tooth decay if you have underdeveloped or weak enamel.
A lowered immune response will also give free rein to the oral bacteria, which might lead to tooth decay.
Tooth color is determined by several factors, some of which are intrinsic while others are extrinsic.
Enamel, the outermost layer of teeth, is opaque white, while the underlying dentin is yellow.
People who are born with thin enamel have teeth that look yellow.
But this can also happen due to age when the enamel wears off, exposing the underlying yellow dentin.
Tooth color is determined by how your teeth develop in your fetal life.
If exposed to the antibiotic tetracycline in the womb, you will likely have yellow teeth.
Teeth can also become stained due to smoking or drinking coffee.
All these reasons show that you can have yellow teeth due to genetic and environmental factors.
The most prevalent risk factor for oral cancer is tobacco use.
However, this cancer might run in families.
Squamous cell carcinoma (SCC) is the most common type of oral cancer.
You are more likely to develop SCC in your mouth or head region if your close relatives, such as a parent or a sibling, have this condition.
If you have more or less than the normal number of teeth in your mouth, it might lead to misalignment and crowding.
The genes that usually cause this anomaly are MSX1, PAX9, EDA, and AXIN2.
Hand-picked Content For You: How Does Calcium Deficiency Affect Teeth?
You can't control your genes and their effect on your oral health.
However, you can always be more vigilant about your oral hygiene routine to overcome the effects of bad teeth genes.
Dental issues can be a result of both genetic as well as environmental factors.
You might be born with bad teeth genes, but it does not mean caring for your teeth is pointless.
Common dental problems like tooth decay, cavities, and gum inflammation are all influenced by genetic risk factors.
However, sugary foods and smoking can also increase the risk of developing these conditions.
So, being vigilant about your oral health is always a good idea.
If you have bad teeth genes and dental problems run in your family, consult your dentist.
You might need some extra products or care to maintain your oral health.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9192175/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4449725/
https://www.news-medical.net/health/Are-Genes-Involved-in-Tooth-Decay-and-Gum-Disease.aspx
https://www.nature.com/articles/s41421-019-0126-6
https://pubmed.ncbi.nlm.nih.gov/23318742/
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0010053#s2
WATCH: How to interpret your MTHFR report
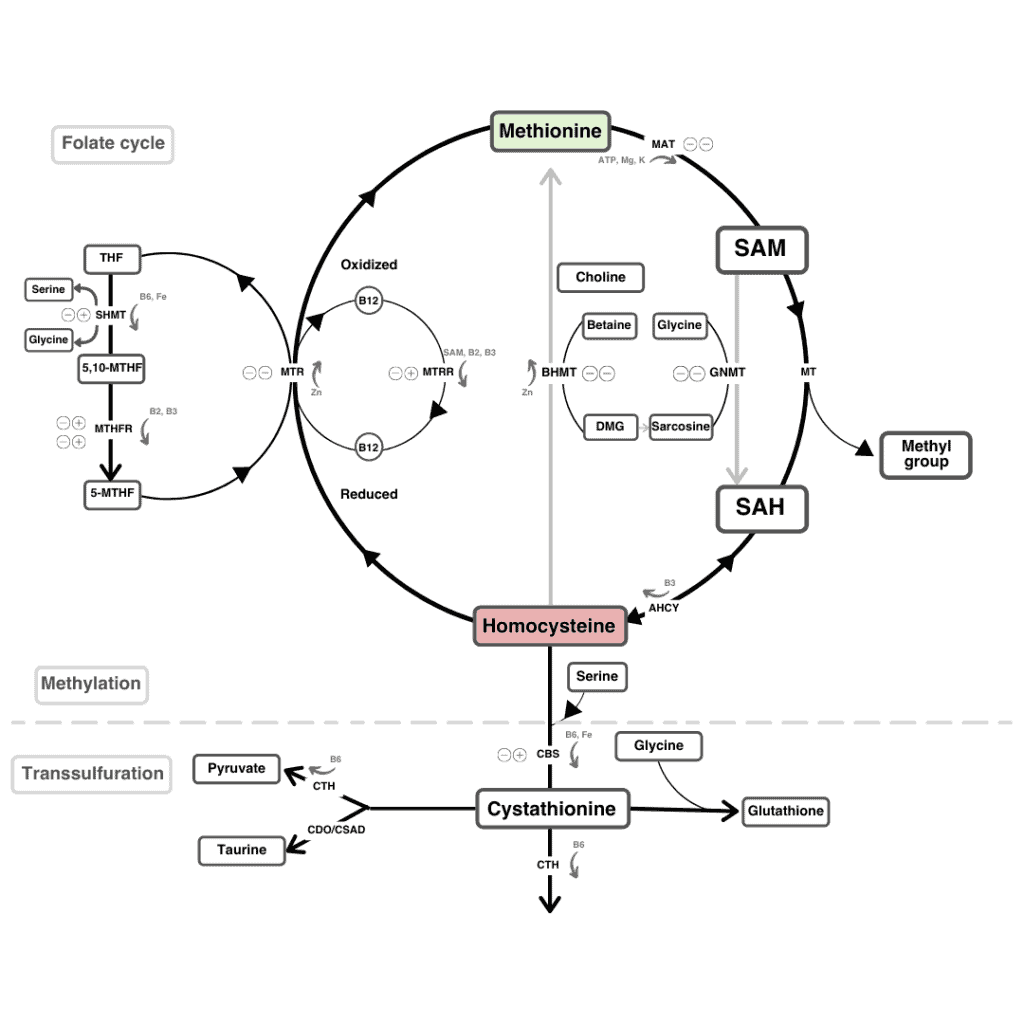
MTHFR stands for methylenetetrahydrofolate reductase and is produced by the MTHFR gene.
MTHFR enzyme performs the function of adding chemical (methyl) groups to folic acid (Vitamin B9) in order for the body to utilize it efficiently.
This process is also necessary for the process that converts the amino acid homocysteine to another amino acid, methionine.
With your 23andMe raw data, you can learn a lot about your MTHFR gene through the Methylation test.
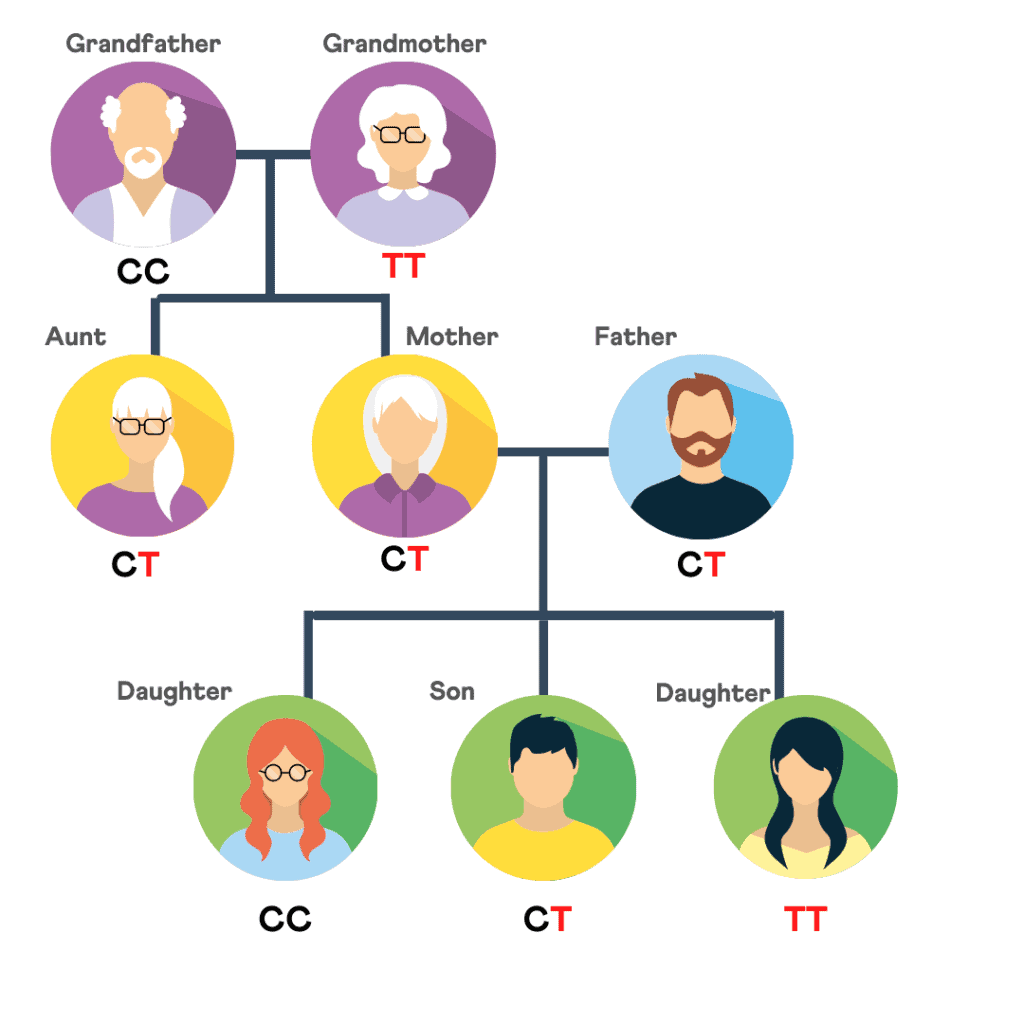
All of us have two copies of the MTHFR gene, one from each biological parent. However, the type of MTHFR gene differs from person to person.
To explain this better, let’s take the example of blood groups. All of us have red blood. But you may have an O+ve blood type, while the other person may be A-ve - and these different blood groups have different health implications.
Like how O+ve and A+ve are the most common blood types, the MTHFR gene also has 2 common variants (type): C677T and A1298C, the former being more common than the latter. These are called the MTHFR gene mutation.
About 40% of the American population have the C677T type, which has been associated with up to 80% reduction in the enzyme’s efficiency
When the MTHFR enzyme levels are reduced, it can lead to various health complications due to homocysteine (harmful amino acid) buildup.
They include:
Once you learn about the type of MTHFR gene you carry, the effects of it can be made better by simple fixes such as dietary changes and folic acid supplements.
An MTHFR gene test examines variations in the MTHFR gene.
This test does not need a medical prescription. It can be performed in a major genetic diagnostic lab such as Quest or LabCorp.
The aforementioned mutations (along with other smaller ones) are tested for in the MTHFR gene to provide the MTHFR gene status
More readily, the 23andMe MTHFR status can be learned from your 23andMe raw data. Anyone with 23andMe raw data can upload their DNA raw data to xcode.life to learn about their 23andMe MTHFR status.
So, the MTHFR “test” does not necessarily have to be a test but can be as simple as uploading your 23andMe raw data (if you already have it) and downloading your results.
There are many service providers and online tools that help you find out about your 23andMe MTHFR status. Some of them are listed below:
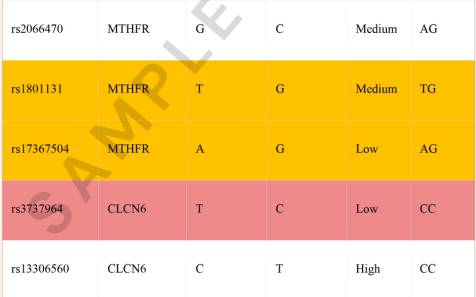
The first section of your report will include the 2 main mutations of the MTHFR gene.
This section, "PROMINENT MTHFR SNPS," includes the 2 SNPs:
The bar graph below will indicate the combined result for these SNPs, which is "MODERATELY REDCUED MTHFR ENZYME ACTIVITY," in this case. This indicates a genetic likelihood of moderately functioning MTHFR enzyme.
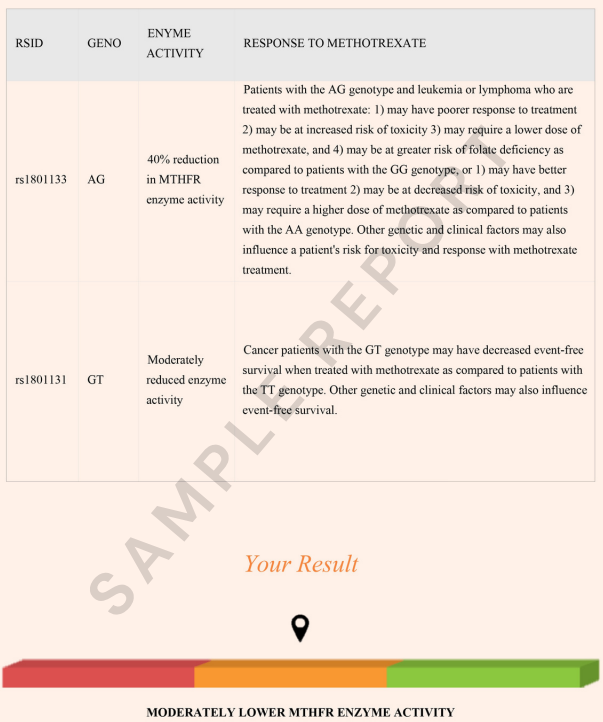
Under the "OTHER MTHFR SNPS," we profile other variants that have a mild effect on the MTHFR enzyme activity but are not considered significant individually.
In the example below, for some, the individual carries one or two copies of the risk and all, and for others, they have two copies of the normal allele. This may have a mild effect on the MTHFR enzyme functioning.
With simple dietary modifications or folic acid supplements, you will be able to mitigate the enzyme deficiency.

If you already have your DNA raw data from an ancestry test you may have done, you can easily find out your 23andMe MTHFR status from your DNA raw data with the Methylation report. Otherwise, you may consider an ancestry test for $99 or less, so that you can get your genetic raw data for further analysis. Once you have your raw data, you can upload it to xcode.life for your 23andMe MTHFR Methylation status report.
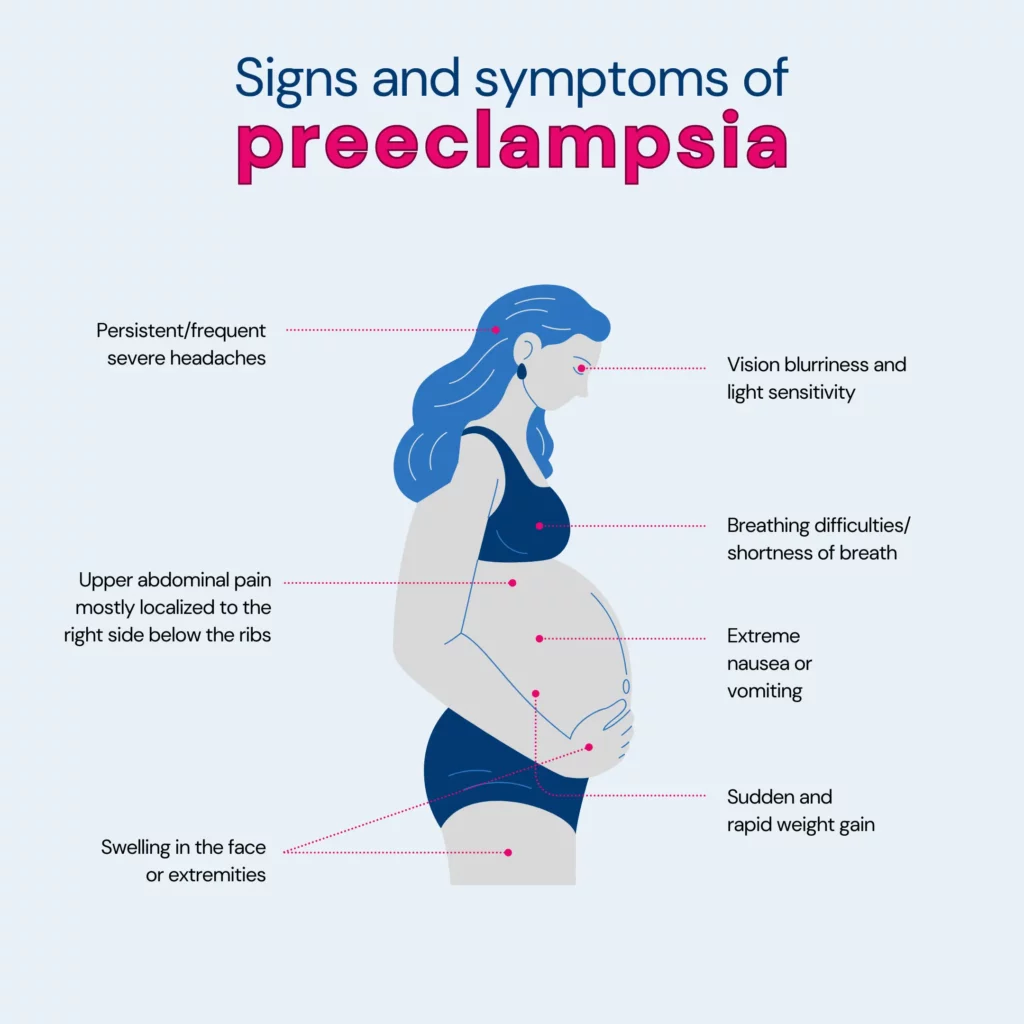
Preeclampsia is a pregnancy complication that affects two hundred thousand pregnant people in the U.S. per year. This worrying number has only been on during and post the COVID pandemic. While certain factors can increase the risk of this condition, research also suggests that family history plays a role here. This article discusses in-depth about preeclampsia, touching upon its risk factors and whether it has any genetic roots.
Preeclampsia is a serious condition that may arise during pregnancy, usually occurring after the 20th week.
It results in high blood pressure (hypertension) and is often linked with the presence of protein in the urine (proteinuria), suggesting potential kidney issues.
Preeclampsia can extend its impact to other organs, such as the liver, leading to additional symptoms.
Although it commonly resolves post-childbirth, neglecting treatment can pose significant health risks for both the baby and the mother.
Preeclampsia is usually seen in first pregnancies, but if there is a history of it in the previous pregnancy/ies, then the risk of preeclampsia in future pregnancies is seven times higher!
While it can affect anyone who is pregnant, certain factors increase the risk. Let's take a closer look at them:
Remember, individual risk varies depending on the combination of factors present in each person.
Regular checkups with your healthcare provider throughout the pregnancy are vital steps, ensuring your and your baby's well-being.
Yes, there is substantial evidence suggesting a genetic component in the development of preeclampsia.
Scientists did an extensive study, checking 775 tiny genetic variations in 120 genes of over 350 moms with preeclampsia and 602 without it.
They identified six genes (IGF1, IL4R, IGF2R, GNB3, CSF1, and THBS4) that contribute to preeclampsia development through a combination of maternal and fetal genetic changes.
Yes, there is a familial link to preeclampsia, indicating a genetic influence on the condition, such as:
Yes, if your mom had preeclampsia during her pregnancy, there is an increased risk that you may also develop preeclampsia during your pregnancy.
A cohort study involving 22,768 elder daughters and 2,959 younger daughters revealed a link between a mother's preeclampsia and her daughters' vulnerability to it.
Mothers having preeclampsia during the first pregnancy with an elder daughter increase the elder daughter's risk of developing it in her own first pregnancy by 1.7 times. This risk continues into the second pregnancy.
The study found similarly elevated risks for daughters if the mother had preeclampsia in any other pregnancy or if only mothers with firstborn children were considered.
However, it's important to note that genetic predisposition explained only a minor part of preeclampsia occurrence in the population studied.
Preventing genetic preeclampsia isn't guaranteed because it depends on factors beyond your control. However, there are steps you can take to reduce the risk or manage it:
The best-known method is low-dose aspirin, typically an 81-milligram tablet daily after 12 weeks of pregnancy.
Your primary care provider may recommend this if you have one high-risk factor for preeclampsia or more than one moderate-risk factor.
Being as healthy as possible before pregnancy is advised, especially if you've had preeclampsia before.
Manage any conditions that increase the risk of preeclampsia by discussing them with your healthcare provider.
Note: Before taking any medications, vitamins, or supplements, it's crucial to consult your provider to ensure safety.
Preeclampsia can bring about various health challenges, including:
Understanding these potential impacts is crucial, and early detection and management are essential for the well-being of both the mother and the baby.
Additional factors that might slightly raise the likelihood of developing preeclampsia include:
Preeclampsia is a serious condition during pregnancy with high blood pressure and protein in urine.
It's more likely in first pregnancies, especially if there's a family history or if it happened before.
Genetics is a factor, but it doesn't explain everything. If your mother had it, you're at a higher risk.
Taking low-dose aspirin as prescribed by your doctor and adopting a healthy lifestyle can help lower your risk.
Preeclampsia can cause problems for both mom and baby, so early detection and care are essential.
Age, obesity, and certain conditions can also affect the risk. Regular checkups and healthy choices make a big difference in having a safer pregnancy.
https://www.nhs.uk/conditions/pre-eclampsia/
https://www.news-medical.net/health/The-Genetics-of-Pre-Eclampsia.aspx
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4060423/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3145161/
https://pubmed.ncbi.nlm.nih.gov/10468424/
https://www.mayoclinic.org/diseases-conditions/preeclampsia/symptoms-causes/syc-20355745
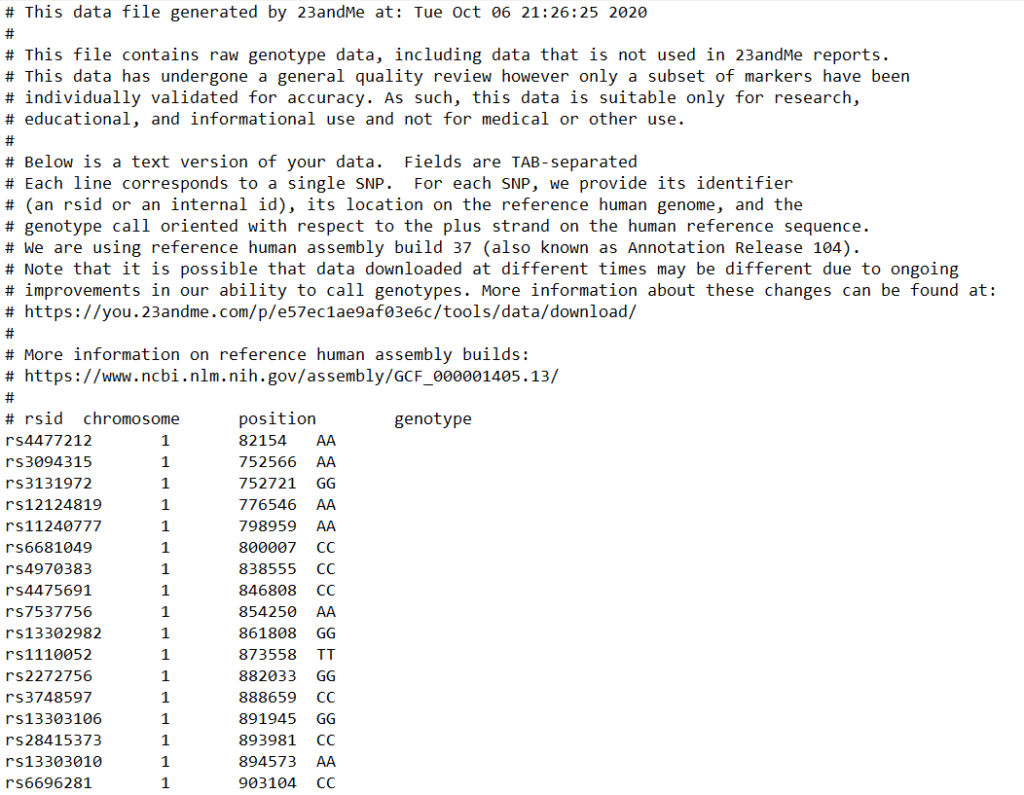
One of the most important parts of your 23andMe results is the DNA raw data, which contains information on more than 700,000 genetic markers. While only a fraction of these markers are utilized to trace your lineage, the remaining data holds invaluable insights into your health and wellness, including potential risks for certain diseases. Unlocking this wealth of information is straightforward. By following seven simple steps, you can swiftly download your DNA raw data file in under a minute. Xcode Life can then analyze this data to provide ten comprehensive reports, offering you a deeper understanding of your health.
Video explainer: How to download 23andMe DNA raw data.
Sign in to your 23andMe account from the 23andMe website
Click on the down arrow near your name from the top navigation bar
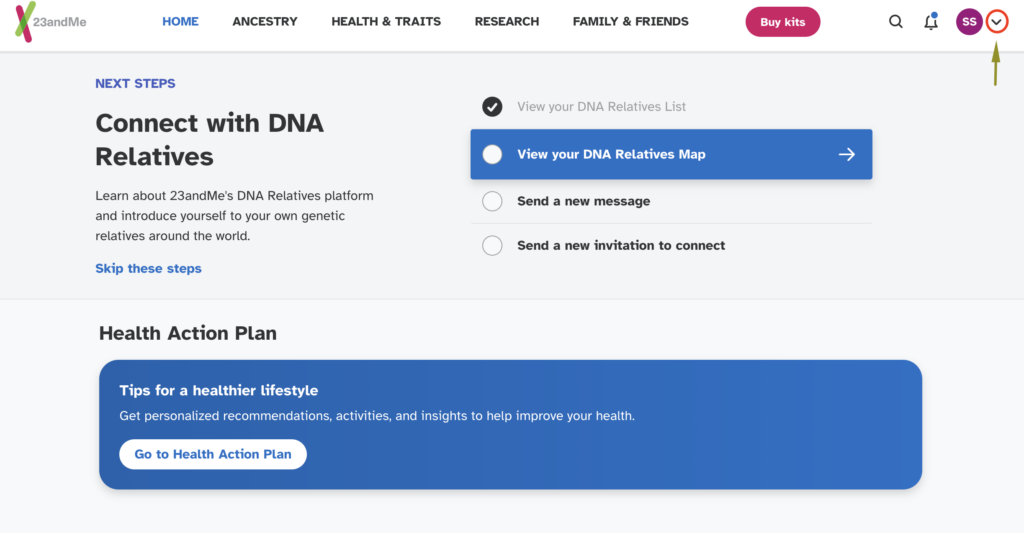
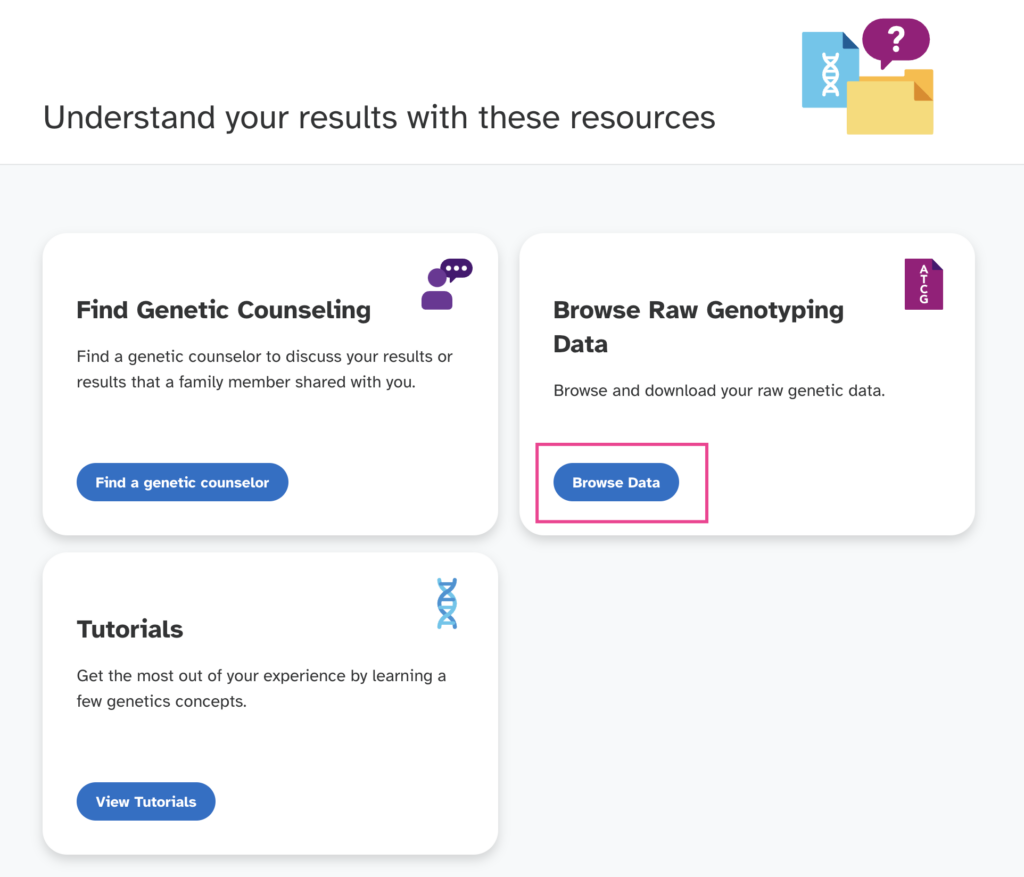
Select "Resources" as shown below
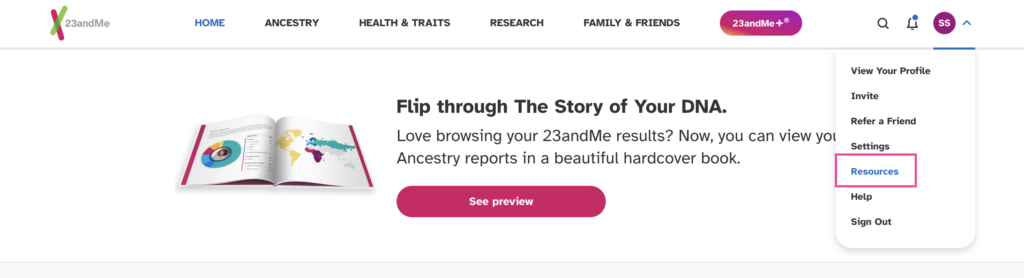
Click on the 'Browse Data' button
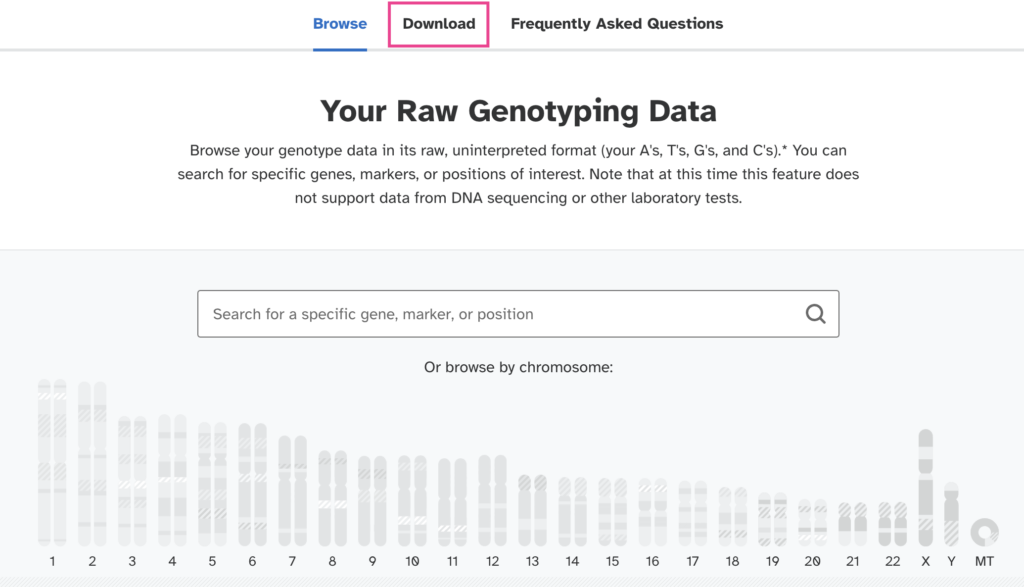
Select the "Download" option from the next page.
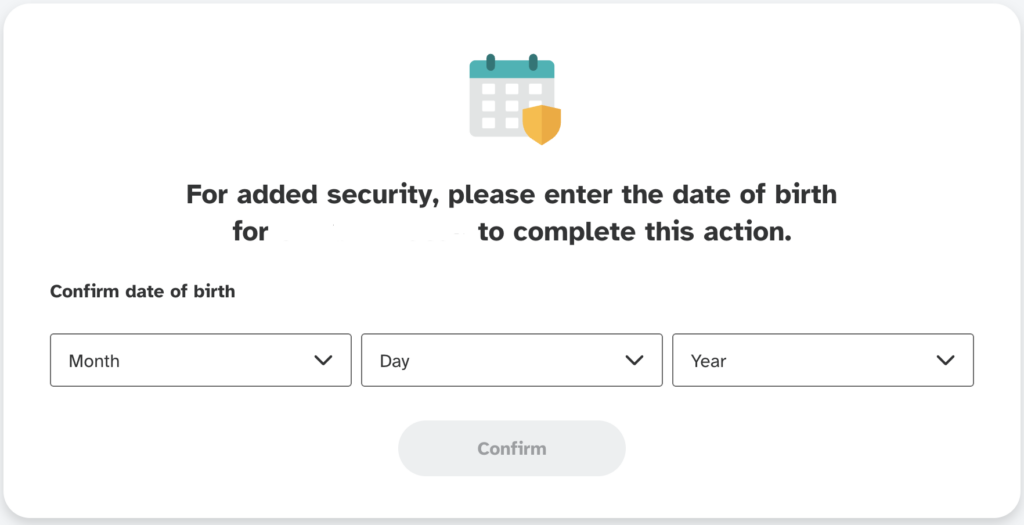
Enter the same date of birth you had given when registering your account.
On the next page scroll down to the bottom of the download page until you see the "Submit request" button.
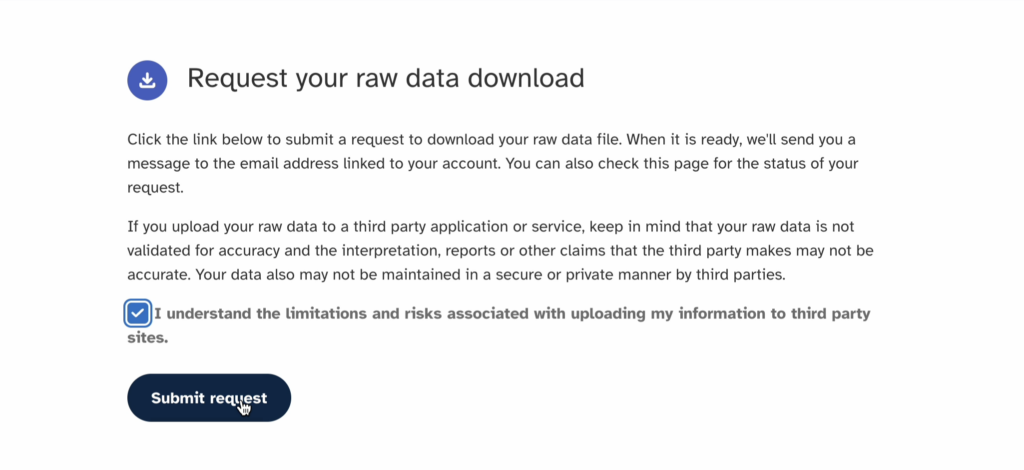
23andMe will send you an email notification once your raw data is ready, or you can just refresh your download page. This may take 2-4 days.
OR, you can directly access the download page here
Also see, Free tools for 23andMe, AncestryDNA, FTDNA raw data analysis
Final notes:
Your DNA raw data is a file of size 5-7 MB in the .zip format or 16-21 MB in the .txt format.