Companies like 23andMe, Ancestry DNA, and Family Tree DNA (FTDNA) enjoy popularity in the ancestry DNA testing arena.
You can learn interesting insights about different aspects of your health and wellness.
DNA raw data provided by them is used to obtain additional health reports from third-party DNA raw data analysis tools.
Xcode's DNA raw data analysis tool is compatible with the raw data information from many more service providers.
Here is a comprehensive list.
*For companies not on the list, you can email us at hello@xcode.life to check compatibility.
**We have temporarily discontinued the processing of whole genome files from Nebula, Self Decode, Helix, and other formats. Please check back with us in 6 months for updates.
At Xcode Life your data privacy is our top priority. Which is why we are one of the few companies that let our users have complete control over their data. Find out the different ways by which Xcode Life protects user data:
Also read:
What Else Can I do With my 23andme, Ancestry DNA, FTDNA raw data?
10 Amazing Tools For 23andme Raw Data Analysis
Loneliness is a complex and often painful emotion felt by people around the world.
Most people have experienced it at one point or another. But for some, it's a constant battle.
Though its causes are varied, new research suggests that loneliness may be partially attributable to genetics.
Genetically-informative studies have estimated that genetic factors account for approximately 40–50 % of the variance in loneliness.
Loneliness has been linked to an increased risk of premature death, heart disease, anxiety, and depression.
It's also been shown to contribute to cognitive decline and Alzheimer's disease.
So, it's clear that loneliness is not something to be taken lightly.
There's a lot of stigma surrounding loneliness, due to which it's been trivialized and ignored for many decades.
But loneliness is emerging as a public health problem.
According to a report on social isolation and loneliness in the UK, 200,000 older people hadn’t had an interaction with a friend or relative for more than 30 days.
Further, the report states that the impact of social isolation and loneliness is “twice as harmful as obesity and is comparable to smoking 15 cigarettes a day or being an alcoholic.”
According to Cigna’s 2020 Loneliness Index measuring loneliness and social isolation, 61% of Americans reported that they sometimes or always feel lonely.
The numbers were even higher in younger people – 79% of Generation Z and 71% of millennials reported loneliness.
According to the CDC, many adults older than 50 experience social isolation and loneliness to the extent that it impacts their health.
Recent studies found that:
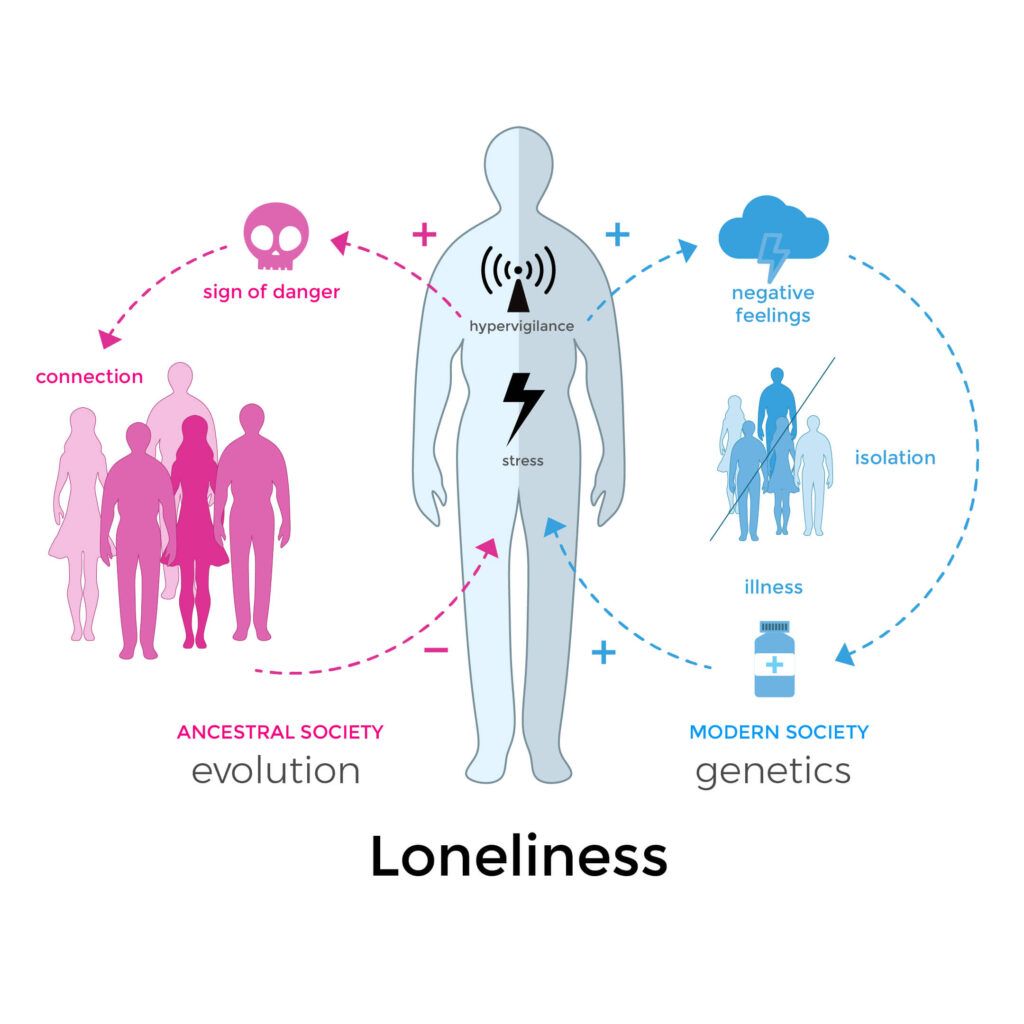
Loneliness is a hereditary trait that served to improve our chances of survival as a species.
To the archaic human, loneliness sent a paradoxical signal to the brain.
It was a motivating force to connect with others to increase the chances of passing one’s genes to the next generation.
On the other hand, loneliness also triggers the body’s fight-or-flight response.
When hunting alone, loneliness brings about anxiety and hyper-vigilance, which can be handy under dangerous encounters.
Researchers at the University of California San Diego School of Medicine conducted the first GWAS for loneliness.
Previous studies have examined the heritability of loneliness in twins, children, and adults.
After analyzing the results of these studies, the researchers estimated that 37 to 55 percent of loneliness is influenced by genetics.
Older research also pinpoints genes that regulate the levels of brain chemicals like dopamine and serotonin contributing to loneliness.
But these studies have relied on only small sample sizes.
The GWAS considered genetic and health information of 10,760 people aged 50 and older.
The participants were made to answer questions like:
The research team found that loneliness as a tendency to feel lonely over a lifetime (and not occasional loneliness due to circumstances) has a modest heritability of 14-27%.
The lowered genetic contribution arrived at in this study could be because the team considered genetic changes that were common in the general population instead of the rare ones.
Drawing on survey responses from 487,647 participants of the UK Biobank scheme, a study identified 15 gene regions linked to loneliness.
The researchers also underlined a possible link between obesity and loneliness, suggesting that one might be driving the other.
The same genes that can drive the tendency for weight gain can also increase the risk for loneliness.
The team also identified genetic overlaps of loneliness with other traits like depression, obesity, and heart health, indicating that these traits combine to increase the risk of loneliness.
Two people in very similar situations may feel differently about whether or not they feel lonely, which boils down to the genetic code they’re born with.
This, however, doesn’t mean that there’s a “loneliness genes” or that how we feel is entirely dependent on our genes.
A host of genetic and non-genetic factors are likely to influence loneliness.
Loneliness is a growing problem, with an increasing number of not just older adults but also millennials and Gen-Zs experiencing it. The first GWAS on loneliness reported its heritability of 14-27%. Loneliness also shares genetic links with other conditions like obesity, depression, and heart disease. In fact, researchers report that obesity and loneliness can drive each other. However, there’s no loneliness gene reported so far. Loneliness has both genetic and non-genetic influencers.
Cinnamon is a spice obtained from the bark of the Cinnamonum family.
A popular spice native to the Caribbean, South America, and Southeast America, cinnamon is known to have strong antioxidant, anti-inflammatory, antidiabetic and antimicrobial properties.
Gluten is a family of proteins found in grains like wheat, rye, and barley and gives dough elasticity.
Cinnamon, being a spice, is gluten-free.
While most people can safely consume gluten, an increasing number of them are becoming intolerant.
People with conditions like celiac disease, irritable bowel syndrome, and gluten sensitivity must avoid gluten consumption to prevent adverse reactions.
To avoid side effects or allergic reactions due to gluten, many people choose to go gluten-free.
A gluten-free diet is important to manage the signs and symptoms of gluten-related health conditions.
A gluten-free diet is also important for people who haven’t been diagnosed with a gluten-related medical condition but wish to experience other benefits such as weight loss, improved energy, and better overall health.
Gluten intolerance is a condition in which you may get sick after eating gluten.
Common symptoms that you may experience in the case of gluten intolerance are nausea, bloating, and feeling tired.
Gluten intolerance is also called non-celiac gluten sensitivity.
Since people with celiac disease are gluten intolerant, many confuse the two conditions.
Gluten intolerance and celiac disease are different.
People with celiac disease have an autoimmune response to gluten, which means their body presumes gluten as an infectious agent and launches an immune reaction toward it.
This inflammatory reaction damages the digestive tract and results in symptoms characteristic of the disease.
Celiac disease occurs due to the presence of an abnormal gene change.
Gluten intolerance affects nearly 6% of the US population.
Anyone can develop gluten intolerance, though it is more common in women.
While some people are born with gluten intolerance, others develop the condition later in life.
The Human Leukocyte Antigen (HLA) system of genes is associated with the production of cell-surface proteins and helps regulate the immune system.
Six single nucleotide polymorphisms (SNPs) in the HLA gene complex, namely HLA DQ, HLA DQ 2.5, HLA DQ 2.2(3 SNPs), and HLA DQ7, are associated with gluten intolerance.
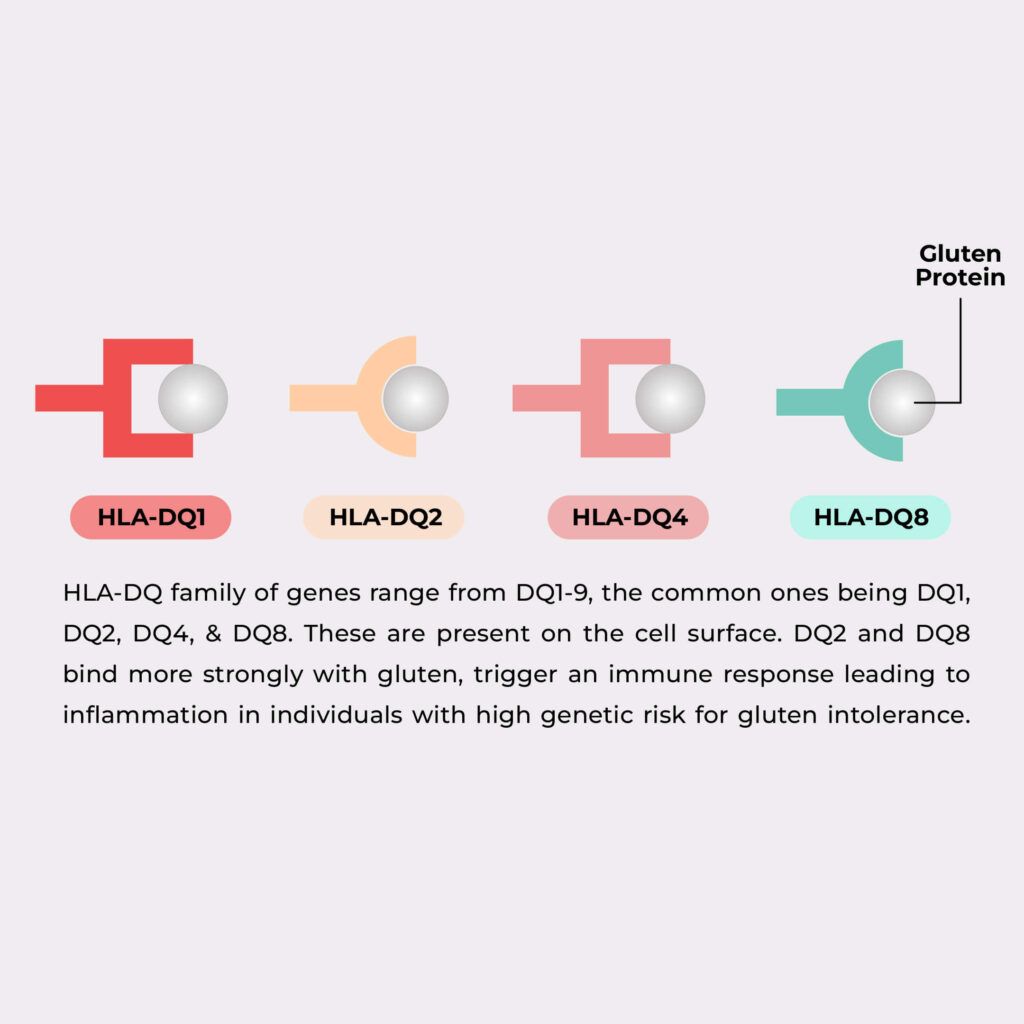
Image: HLA Genes and Gluten Intolerance
The HLA DQ genes are strong predictors of celiac diseases.
A study conducted to understand individuals' susceptibility to gluten intolerance found that people with celiac disease had the risk alleles in the HLA DQ2 and HLA DQ8 genes.
In another study, people with the following genes and respective variants were found to have a reaction to gluten in the diet:
| Gene | Risk Variant |
| HLA DQ | G variant |
| HLA DQ 2.5 | T variant |
| HLA DQ 2.2 | G variant |
| HLA DQ7 | A variant |
Cinnamon is a spice, and so it is naturally gluten-free.
Though cinnamon is gluten-free, manufacturers may add some flour to help with caking.
In this case, ground cinnamon may contain some gluten.
Additionally, there may be contamination in the manufacturing facility, wherein ground cinnamon may contain gluten.
If you buy fresh, unground cinnamon, you can be sure it does not contain gluten.
If you are purchasing cinnamon powder, you should check out the product's label to confirm the presence or absence of gluten.
If the manufacturer says the cinnamon is gluten-free, it may not contain any gluten-containing ingredients.
In some cases, the manufacturer can say the product is ‘certified gluten-free; this means it may contain less than 20ppm of gluten.
Whole exome sequencing (WES) is a powerful tool that can provide insights into the genetic causes of disease. WES can identify mutations in genes associated with inherited conditions, diagnose rare diseases, and guide treatment decisions. Here we provide an overview of WES, how it is performed, and its potential applications.
Genetic testing has been employed in healthcare areas like cancer and prenatal diagnostics for some time now.
Whole exome sequencing is a popular genetic test choice, and that’s increasingly being used to understand what is causing a condition or a set of symptoms.
Exome sequencing is done at certified laboratories by specialists who extract the DNA from saliva or blood.
The geneticists and bioinformaticians then sequence the exome from the DNA extracted to look for mutations and variation.
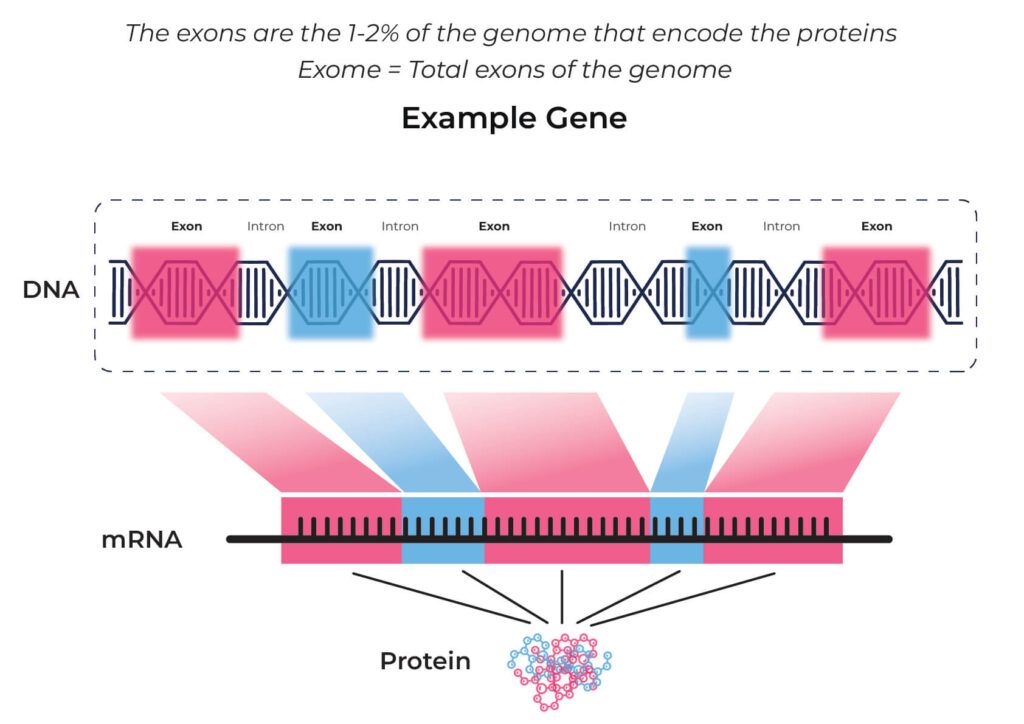
The entire DNA content of a human, called the genome, is made up of more than 3 billion base pairs (meaning: the letters A, T, G, and C).
Not all of these 3 billion letters can provide instructions for forming proteins.
Only 1-2% of the entire DNA can form protein. This portion of the DNA, also called the coding region, is known as the exome.
85% of all genetic changes associated with diseases can be found in the exome.
So, in clinical settings, whole-exome sequencing is more commonly done than whole-genome sequencing.
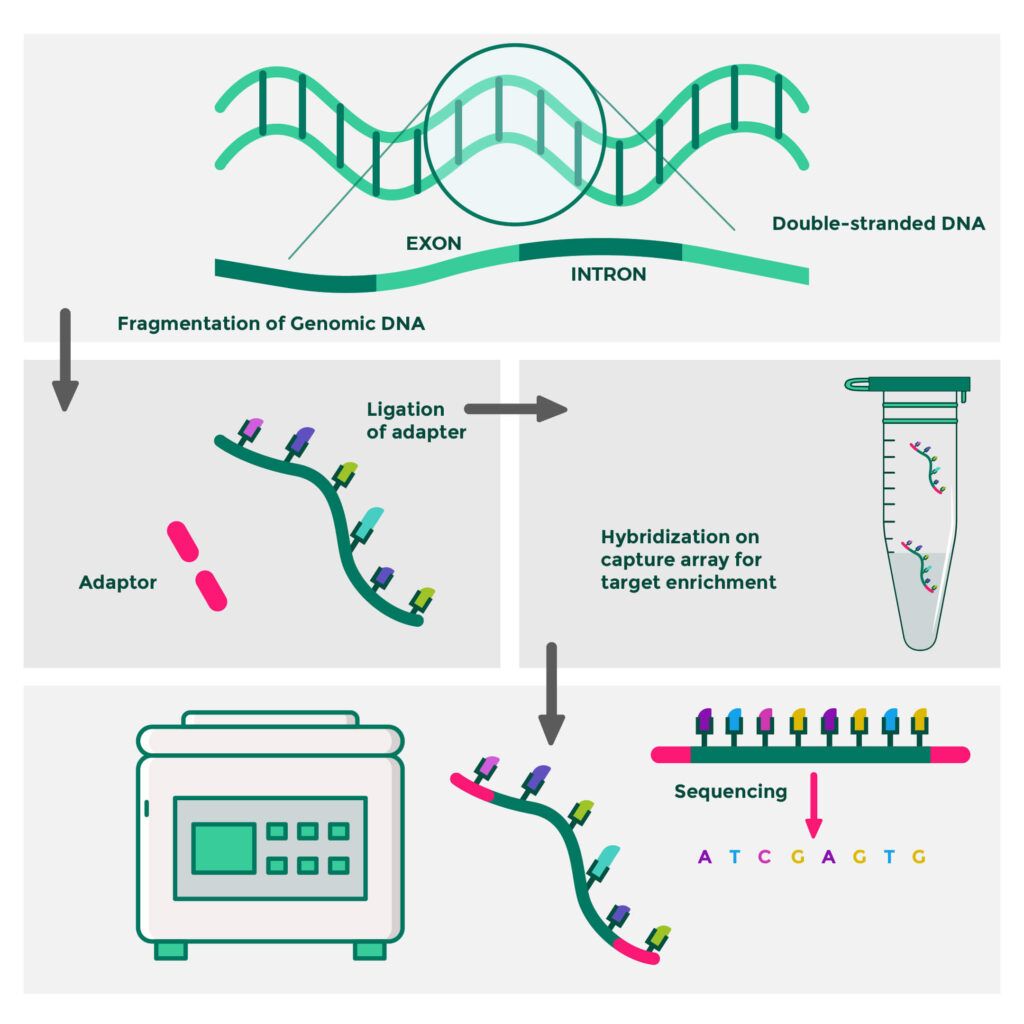
The whole exome sequencing is done in three steps.
There are many techniques to isolate the DNA from the sample, and the method employed depends on the application.
Commonly arrays are used, where probes are designed to capture the portions of interest.
DNA sequencing determines the order of the four letters (A, T, G, and C) that make up the DNA molecule.
Sanger sequencing technology is the original one that was a breakthrough in helping scientists determine the human genetic code.
But it was a time-consuming and expensive technology.
Fast forward to a few years later, next-generation sequencing (NGS) took the genetic world by storm with a faster turnaround time and less heavy on the pocket.
With NGS, it is possible to sequence large amounts of DNA, like all the portions that contain the code to produce proteins (exome).
Analysis of the human genome is a data-heavy process.
Decoding as little as 1% of human DNA produces data of around 8 GB.
There are several programs to decode these reads.
Variants (or genetic changes) are present in several file formats like FASTQ, BAM/CRAM, and VCF.
A rare variant is a genetic change that alters gene function and occurs at a low frequency in a population.
Rare variants may play a significant role in complex diseases.
Since most disease-causing variants are found in the exome, exome sequencing remains a very active and ongoing area of research in discovering rare variants.
Mendelian disorders are a type of genetic disorder that occurs when an alteration in single genes is inherited from the parents, resulting in disease.
Mendelian disorders are typically very severe.
So the genetic mutation causing the disorder is presumed to be very rare in the population.
Exome sequencing uses advanced technologies that can help discover these variants.
Exome sequencing can help identify the underlying genetic mutation causing a disease.
Having this information can influence the diagnostic approach and treatment options.
Further, it can predict the inheritance pattern of the condition, making it possible to test at-risk family members.
There are many potential benefits of exome sequencing.
There are many psychological repercussions to getting your genome sequenced.
Since exome sequencing can reveal most disease-causing variants, you may uncover that you are at risk for a condition you weren’t originally planning to investigate.
Since you share your DNA with other family members, this type of finding can have an impact on them as well.
Talking to your healthcare provider about all the risks involved before electing for whole exome sequencing is important.
Alzheimer's disease is a complex disorder with multiple causes. One important factor in the development of Alzheimer's disease is genetics. In this article, we will explore the role of genetics in Alzheimer's disease. In particular, we will discuss how the ApoE gene can increase or decrease a person's risk for Alzheimer's disease.
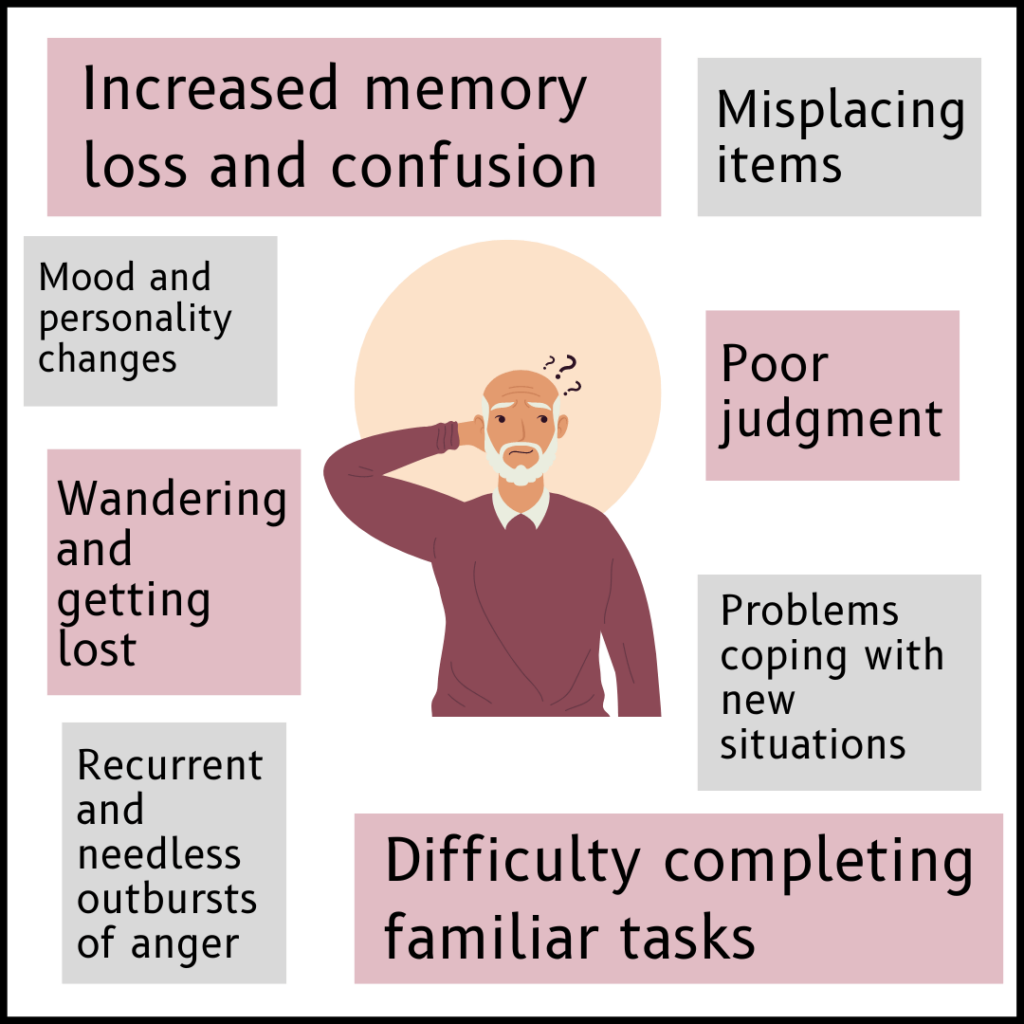
Alzheimer's disease (AD) is the most common cause of dementia in the elderly.
People with Alzheimer's exhibit a progressive decline in memory, function, language, and other areas of cognition.
This condition is characterized by the formation of amyloid plaques and tau tangles in the brain, which we will explore in detail in the later sections.
While many genes have been studied in association with Alzheimer's, the only strongly confirmed genetic risk factor across many studies for early, and late-onset AD is apolipoprotein E (ApoE) genotype, with the E4 allele being an AD risk factor and the E2 allele being protective.
The ApoE gene is responsible for producing a protein called Apolipoprotein E.
The APOE protein combines with fats (lipids) and cholesterol in the body to form lipoproteins.
It is responsible for metabolizing and clearing out fats and cholesterol from the body.
Besides its role in fat metabolism, it’s also been found to regulate the immune system and cognitive (thought) processes within the brain.
Most of the ApoE is produced in the liver.
The rest of it is produced in the brain.
We all have the ApoE gene but carry different versions of it, just as we have different blood types.
The three versions of the ApoE gene are E2, E3, and E4.
They are also called the isoforms of the ApoE gene.
Each of these results in small differences in the ApoE protein.
These differences alter the activity of the protein and the lipoproteins it is associated with.
The ApoE3 type is believed to be the most common version present in humans.
Since we carry two copies of every gene, one each from the mother and father, there are six possible combinations:
The E3/E3 is the most common type found in about 60% of the general population.
E4/E4 has the strongest genetic link for Alzheimer’s and is associated with a higher than normal risk.
E2/E4 and E3/E4 also increase the risk of Alzheimer’s, though not as much as E4/E4.
There are two types of Alzheimer's, early-onset and late-onset.
Both have a genetic association.
This is the more common type of the two.
The symptoms start to appear roughly in the mid-60s.
There's no direct genetic cause for late-onset Alzheimer's.
However, certain isoforms of the ApoE gene are associated with the risk of Alzheimer's.
We'll see more about this in the upcoming section.
This is a rare type of Alzheimer’s.
In fact, it represents less than 10% of all Alzheimer’s cases.
The symptoms can start to appear anywhere between the mid-30s to the mid-60s.
Three genes have been implicated in the risk of Early-onset Alzheimer’s. They are
The genetic association centers around the build-up of amyloid plaques, a hallmark of Alzheimer’s disease.
Many molecular and cellular changes occur in the brains of people with Alzheimer’s.
Two protein clusters are involved in the development of Alzheimer’s.
Amyloid plaques are aggregates of a protein called beta-amyloid.
This protein is a part of a larger protein called amyloid precursor protein, or APP in short.
Beta-amyloid is made up of 42 amino acids (beta-amyloid 42) and has a sticky nature.
So they easily bind to one another to form amyloid plaques.
Some genetic variants that change the function of gamma-secretase are associated with early-stage Alzheimer’s disease.
Gamma secretase is involved in the cleaving of APP to form beta-amyloid 42.
The mechanism of how beta-amyloid 42 build-up becomes toxic to the brain is unclear.
According to some studies, the plaques release free radicals (unstable molecules that damage cells) that end up attacking the neurons.
Research also suggests that the plaques result in an imbalance in calcium levels, ultimately leading to neuronal death.
ApoE and Amyloid Plaques
ApoE has been associated with plaque formation.
It has multiple functions in regulating beta-amyloid clearance, aggregation, and deposition, all of which can affect Alzheimer’s pathogenesis.
Research shows that ApoE competes with the amyloid proteins for binding with the receptors.
ApoE4 exacerbates the brain accumulation and subsequent deposition of beta-amyloid proteins.
Neurons are cells that are the fundamental units of the brain.
Healthy neurons are supported by structures called microtubules.
Tau proteins are molecules that bind and add stability to the microtubules.
With Alzheimer’s, the tau proteins start to detach from the microtubules and instead bind to one another, forming plaques (known as tau tangles).
The tangles block the communication pathway between neurons, causing their dysfunction.
Some studies have suggested that tau protein accumulation often occurs in the regions of the brain associated with memory.
ApoE and Tau Proteins
The research on how different isoforms of ApoE contribute to tau plaque formation is a bit hazy.
Some studies suggest that ApoE contributes to beta-amyloid Alzheimer’s pathology but not tau Alzheimer’s pathology.
However, a 2019 study that explored the relationship between ApoE4 and Tau in Alzheimer’s found that ApoE4 carriers did have more tau tangles in the brain than noncarriers.
This suggests that ApoE4 may accelerate tau pathology in the key Alzheimer’s Disease region.
Yet another study found a relationship between the ApoE2 isoform and increased tau pathology.
The mice injected with the ApoE2 isoform exhibited a significant increase in tau aggregates and behavioral abnormalities.
The E4 allele frequency is estimated to be about 15% in the general population but is around 40% in Alzheimer’s patients.
ApoE4 is thus considered a risk factor for Alzheimer’s.
However, it is important to note that not all people with E4 will develop Alzheimer’s.
At the same time, not carrying E4 doesn’t mean one will not develop Alzheimer’s.
Other brain-related changes that occur as you age also may be causative factors of Alzheimer’s.
Some of them include:
The idea of using ApoE4 as a target for Alzheimer’s treatment revolves around delaying the onset and progression of dementia instead of curing the condition itself.
Such treatment would likely slow down the neurodegenerative decline in ApoE4 carriers.
A study claims that such ApoE4 targeted treatments in ApoE4 carriers without dementia could slow down the onset of the condition by 7 years!
Treatments that target ApoE4 also help prevent the development of associated conditions like coronary heart disease and atherosclerosis.
Some therapeutic approaches are:
Gene editing is a genetic engineering technique where a gene is changed to manipulate its function or silence it.
ApoE3 and ApoE4 vary only at one position.
Using a technology called CRISPR (a popular technique used for DNA modification), ApoE4 editing has been carried out.
Immunotherapy involves activating our immune system by raising antibodies against the unwanted ‘guest.’
Anti-ApoE immunotherapy can help prevent the accumulation of amyloid plaques.
A novel therapeutic approach uses small molecules called structural correctors.
These molecules correct misfolded protein variants and convert them into their wild-type (normal) form.
ApoE4 protein structure has two domains - the N domain and the C domain.
Interaction between these two domains has been implicated in the pathogenesis of Alzheimer’s. Two ApoE4 correctors disrupt the interaction between the domains.
This transforms ApoE4 into an ApoE3-like molecule.
A mimetic is a molecule that can biologically mimic other molecules like hormones, enzyme substrates, viruses, and other molecules.
These apoE mimetics have both anti-inflammatory and neuroprotective actions.
Treatment with apoE mimetics was shown to significantly improve behavior and reduce inflammation and pathology of the disease in transgenic mice.
The ApoE gene encodes the apolipoprotein, which forms lipoproteins mainly involved in cholesterol and fat metabolism in the body.
There are three types of ApoE gene, namely ApoE2, ApoE3, and ApoE4. Each type gives rise to slightly structurally different proteins. E3 is the most common isoform found in people.
The ApoE4 isoform is associated with elevated levels of circulating cholesterol. This isoform has been implicated in many diseases, especially Alzheimer’s. 40% of people with Alzheimer’s are found to have the E4 allele.
Gambling addiction is a serious mental health disorder that can devastate a person’s life. It is characterized by an intense and persistent urge to gamble, despite the negative consequences. Some people seem to be more prone to gambling addiction than others, and scientists are beginning to wonder if there is a genetic component to this addiction. If you have a family member struggling with gambling addiction, you may be at greater risk of developing the condition. If you think you may be addicted to gambling, it is important to seek professional help.
Behavioral addictions revolve around the brain’s reward system, predominantly driven by the dopamine hormone.
Dopamine, the feel-good hormone, plays a critical role in many types of addiction, including gambling, owing to its pleasure-inducing effects.
Feel-good activities like sex, shopping, drug usage, smoking, gaming, and gambling can trigger dopamine release.
The effects of dopamine make the person repeat the activity, and when this continues for a while, it becomes an addiction.
Dopamine’s reinforcement effect seems to play a bigger role in addiction than the direct effect. What does this mean?
Dopamine signaling during pleasurable activities causes some changes in how the brain cell functions.
It hampers certain pathways that enable the person to keep repeating the activity easily without giving it much thought.
This repetitiveness leads to addiction.
Studies suggest that people addicted to the thrill of gambling, in fact, have a lower activation of the reward pathways in the brain.
This is described by a term called the reward deficiency model.
This model suggests that people prone to addiction have a dormant reward system, making them more prone to reward-stimulating activities like gambling.

Most of us can manage to wager a few bets without running into too many problems.
But a few people encounter gambling addiction, which can significantly affect their lives.
This begs the question: are certain people naturally more tuned to develop gambling addiction due to their genetic makeup?
A study published in the June 2017 issue of the Archives of General Psychiatry has attempted to answer this question.
The study was conducted by scientists from the University of Missouri-Columbia and Australia's Queensland Institute of Medical Research.
It involved about 2,700 women and 2,000 men from the Australian Twin Registry.
The researchers asked a bunch of questions to this group and compared the responses between identical twins (with the same genetic makeup) and fraternal twins (50% similar genetic makeup).
The findings show that if a twin had a gambling problem, an identical twin had an increased risk for gambling than a fraternal twin.
The study further reported that while almost all study members gambled, men (3%) were more likely to be gambling addicts than women (1%).
The author says that “genes rule at least 50 percent of a person's propensity to gamble irrespective of sex.”
Exploring the science behind increased propensity to gamble
An analysis of the molecular genetics of gambling addiction revealed specific forms of genes (called alleles) that link to brain chemicals (called neurotransmitters) playing a role in pathological gambling.
This link suggests that certain people may be more prone to gambling addiction due to certain genes influencing how their brains interact with the happy hormones.
People with these genetic changes associated with gambling addiction can pass them down to their children, resulting in a hereditary component of gambling.
The same study identified genes that play a role in the transport of dopamine and serotonin, which were common in people with gambling addiction.
The Monoamine-Oxidase A or the MAO-A gene, in particular, showed a significant link to gambling addiction.
The MAO-A gene is a key contributor to serotonin and dopamine distribution
Certain changes in this gene make people more dependent on pleasurable feelings due to dopamine elicited by gambling events.
For example, a study found that some men carry a change in the serotonin gene, resulting in increased serotonin production when gambling.
This increased production may make gambling more addictive to those with this genetic change.
This change was not identified in females, explaining why men may be more prone to gambling addiction.
Compulsive gambling is found in higher numbers among those younger than 65.
The risk-taking behavior tends to decline as people get older.
Those with mental health disorders like depression, anxiety, bipolar disorder, and attention deficit hyperactivity disorder (ADHD) are at a greater risk of developing a gambling problem.
Stress is frequently identified as a trigger of gambling behavior.
According to a study, almost 50% of individuals with gambling disorders undergoing cognitive behavioral therapy identified negative emotional states, such as stress.
The people around you influence your behaviors and choices.
Surrounding yourself with people who constantly gamble can increase your tendency to gamble due to peer pressure.
Living in an environment where gambling is widely accepted and regularly practiced can significantly increase the chances of becoming a compulsive gambler.
Post-traumatic stress disorder (PTSD) and gambling disorder can go hand in hand.
Studies show up to 34% of people with gambling problems also have PTSD.
In conclusion, gambling addiction may have a genetic component. However, it is also influenced by environmental factors.
If you think you may have a gambling problem, talk to your doctor or mental health professional.
They can help determine if you have a gambling problem and provide insights into the available treatment options.