Seeking a solution for hair loss? Look no further! This article explores oral minoxidil – a revolutionary remedy that has captured the attention of those battling hair loss.
Discover how this medication can potentially restore hair growth and prevent hair loss. The article dives into the science of oral minoxidil, debunking the common misconceptions and providing you with the knowledge you need to make informed choices.
Read on to know more.
Genes can influence drug responses. Carrying certain gene changes can affect drug efficacy and put you at increased risk for side effects. Learn more:
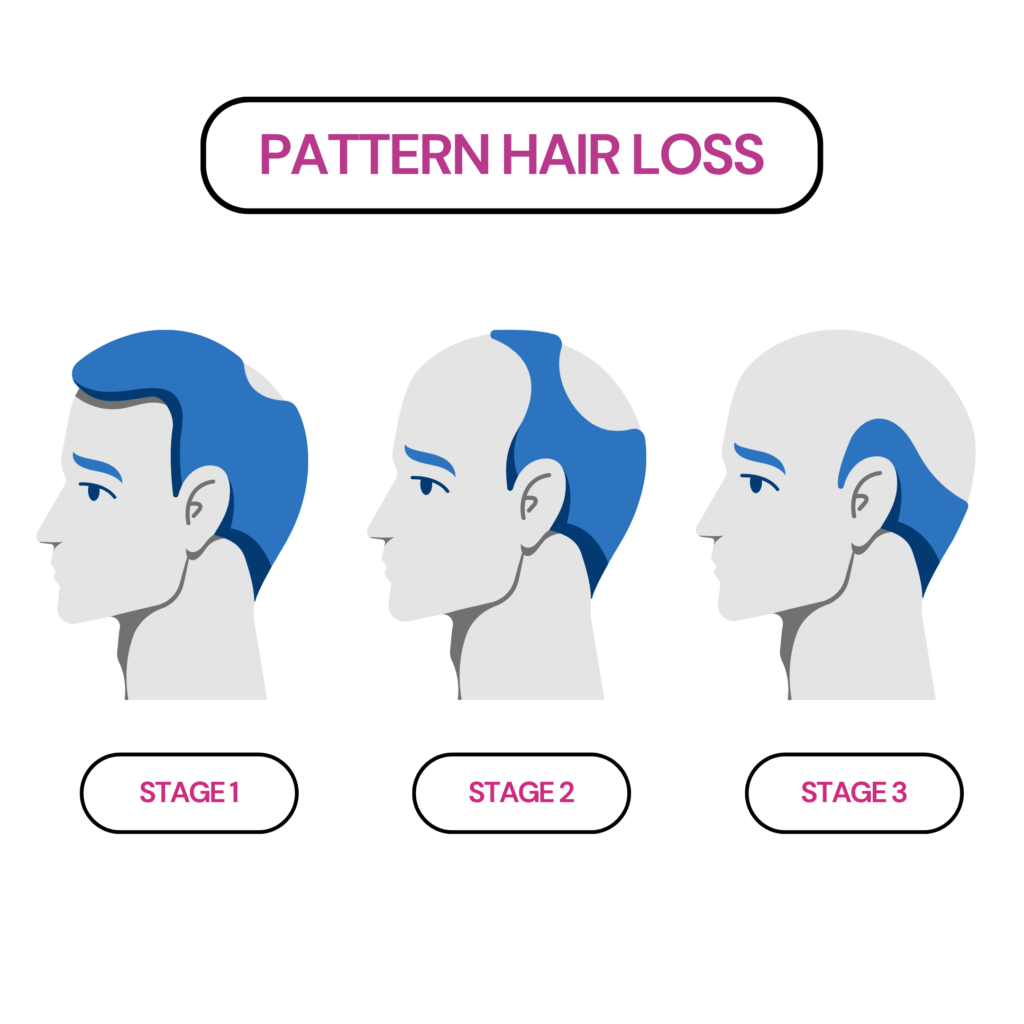
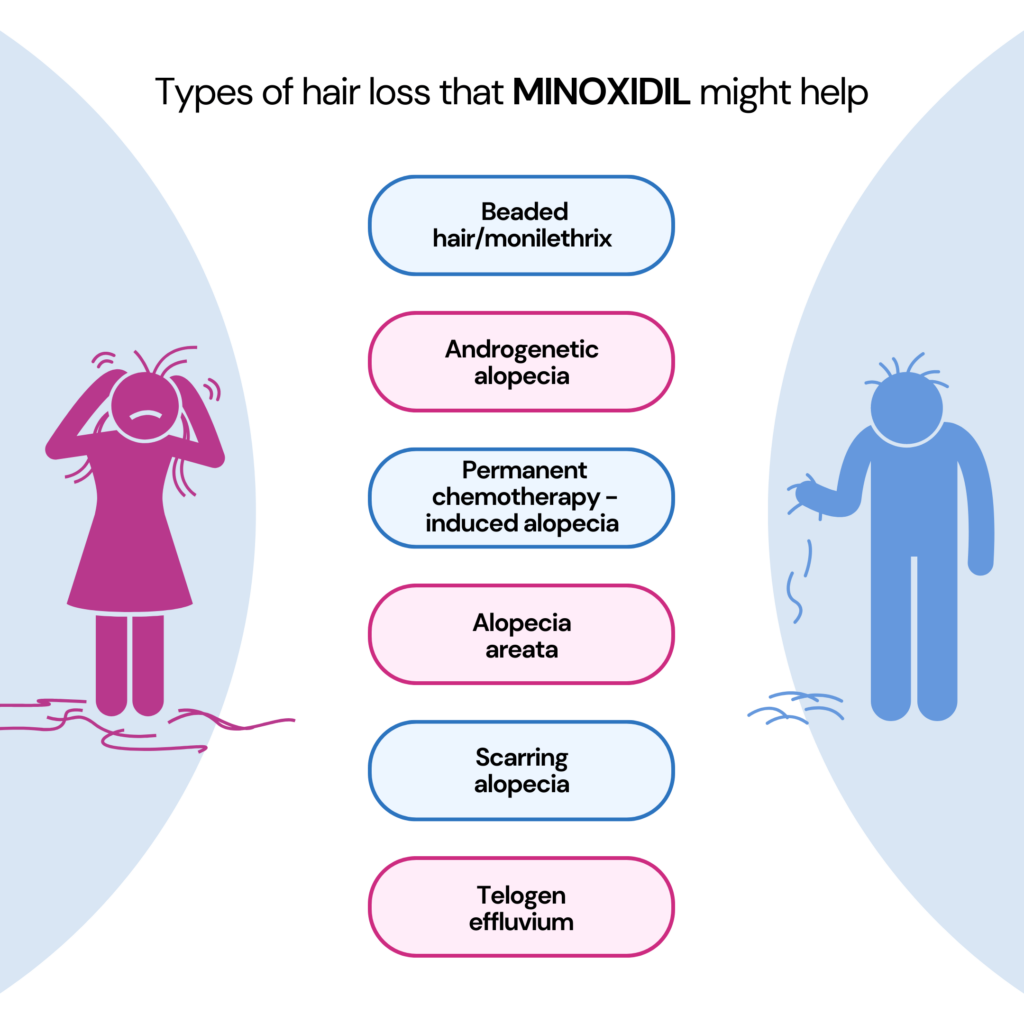
Minoxidil is a powerful medication designed to combat the challenges of a specific form of hair loss known as pattern hair loss.
But apart from their hair loss treatment, minoxidil was originally developed to treat high blood pressure.
You can acquire minoxidil in two ways: by obtaining a prescription for the generic oral tablet or by purchasing the over-the-counter topical solution or foam (MF).
Minoxidil solution (MS) comprises water, ethanol, and propylene glycol (PG), with PG playing a crucial role in delivering the drug to the hair follicles.
Nevertheless, the presence of PG in MS may result in irritation. This prompted the researchers to develop PG-free MF as an alternative.
So, which is better? MF is advantageous compared to MS as it delivers the active ingredient with a specific region and dries faster than solutions.*
Certain versions have minoxidil in the inactive form. It is converted into the active form only upon entry into the body.
This is facilitated by an enzyme called sulfotransferase.
It converts inactive minoxidil into its active form, called minoxidil sulfate. Accordingly, patients with higher enzyme activity had greater hair growth than those with lower ones.
*Not all people respond to minoxidil the same way. Therefore, please consult your healthcare practitioner for advice on which form is better suited for your needs.
The exact mechanism behind minoxidil's effect on hair growth is unknown.
But research has indicated a potential way minoxidil fights hair loss and restores hair growth.
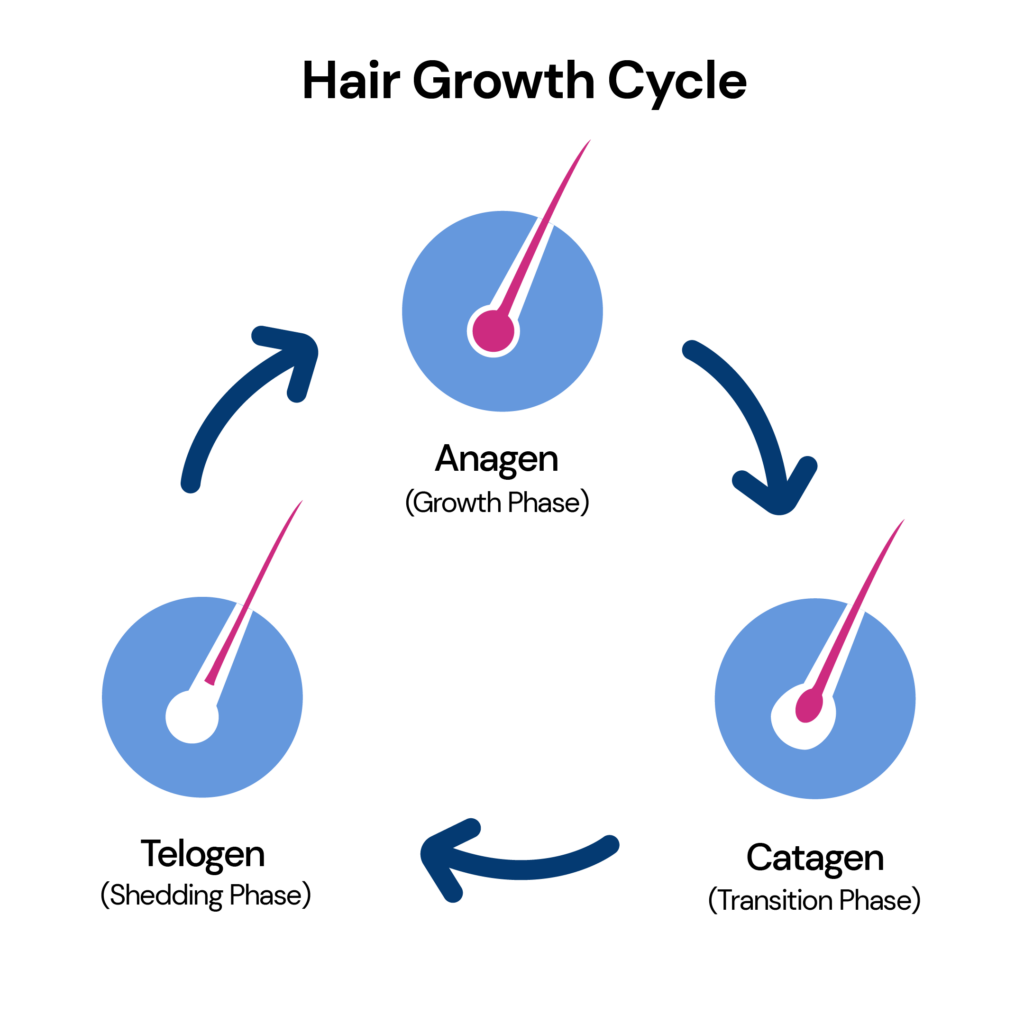
The hair growth cycle encompasses three distinct stages: a phase of active growth called anagen, a transition phase known as catagen that typically lasts around 10 days, and, finally, a resting phase called telogen.
Minoxidil increases the anagen phase, the growth phase of hair follicles, and the hair follicle size while reducing the resting phase.
Drugs like salicylates such as acetaminophen, ibuprofen, and aspirin could lower sulfotransferase enzyme activity.
Topical minoxidil is generally safe, but some patients may experience side effects.
Performing a patch test can help identify the causative agents of the allergic reaction.
Minoxidil exerts its effects on the hair follicles, promoting hair growth and reducing hair loss. However, if you discontinue treatment, the progression of hair growth also ceases.
An initial side effect of oral minoxidil is temporary hair shedding, which typically occurs within the initial six weeks of treatment and lasts around four weeks.
It is important to persist with the medication in order to witness the potential benefits of minoxidil.
The FDA has approved topical minoxidil as an effective female pattern hair loss.
Disclaimer: Using topical minoxidil during pregnancy and breastfeeding may carry potential risks due to its association with fetal malformations. Further, usage during breastfeeding also needs to be approved by a qualified healthcare professional.
A prevalent misconception suggests that minoxidil may diminish male libido, but this claim lacks validity.
Studies report improvements in hair color, length, and coarseness with the consumption of 0.5 mg of oral minoxidil on a daily basis.
Once a person discontinues minoxidil usage, their hair growth ceases, and there is a chance of encountering hair loss comparable to the initial baldness that existed prior to using minoxidil.
Other than minoxidil, several treatment options for pattern hair loss are available. Some of them include:
As we go about our daily lives, it's not uncommon to catch ourselves engaging in a silent conversation with ourselves.
Talking to oneself is a common phenomenon, whether muttering thoughts while getting ready in the morning or reflecting on the day's events.
However, it's often misunderstood and stigmatized as a sign of mental instability.
In reality, decades of psychological research have shown that self-talk is not only normal but also plays a crucial role in our cognitive development and overall well-being.
In fact, the majority of individuals engage in self-talk in some form on a daily basis.
This article explores the reasons behind talking to oneself and the potential impact of this internal dialogue.
Genes influence many aspects of our behavior, including empathy potential, anger temperament, and self-esteem. Learn more:
Self-talk refers to the internal narration within our minds, often called the "inner voice. "
Psychologists define self-talk as verbalized thoughts directed toward oneself or some aspect of one's life.
It includes personal conversations, such as setting goals or affirmations, and reflections on daily experiences.
In the realm of human development, self-talk plays a pivotal role.
Russian psychologist Lev Vygotsky proposed in the 1930s that vocal self-talk was crucial for children's cognitive growth and emotional regulation.
Children often engage in vocal self-talk as they imitate conversations they've had with adults.
Through this process, they learn to manage their behaviors and emotions independently.
As children mature, their outward self-talk gradually transitions into internal dialogue.
This shift from vocal to internal self-talk becomes integral to their cognitive processes, allowing them to plan, problem-solve, and navigate complex situations.
Children acquire the tools to manage their behavior and emotions autonomously by rehearsing conversations and imitating adult interactions.
Inner dialogue becomes a private companion, guiding their thoughts and decision-making.
Studying self-talk poses challenges.
Since most of these talks are often spontaneous, it is difficult to rely on individuals consciously tracking them.
Thus, scientists are trying to get the basics out of the way first by answering some fundamental questions regarding self-talk:
But even with these challenges, one thing is clear: the content of our self-talk can have significant impacts on our attitude and performance.
Engaging in instructional or motivational self-talk has been shown to increase focus, boost self-esteem, and enhance task performance.
For example, athletes who incorporate instructional self-talk during practice tend to improve their concentration and accuracy.
Additionally, self-talk can help regulate emotions, reducing stress and anxiety.
Distanced self-talk, where individuals address themselves in the third person, is especially useful in dealing with emotions.

While self-talk can be a valuable tool, negative and self-critical self-talk can adversely affect our mental well-being.
People who are too tough on themselves may tend to engage in negative self-talk too often to a point where it may get toxic!
The tendency to constantly blame themselves for the problems surrounding them can result in intense feelings of depression.
Further, constant negative self-talk can indicate anxiety in both children and adults!
However, certain psychological tools can help navigate self-talk in the right direction.
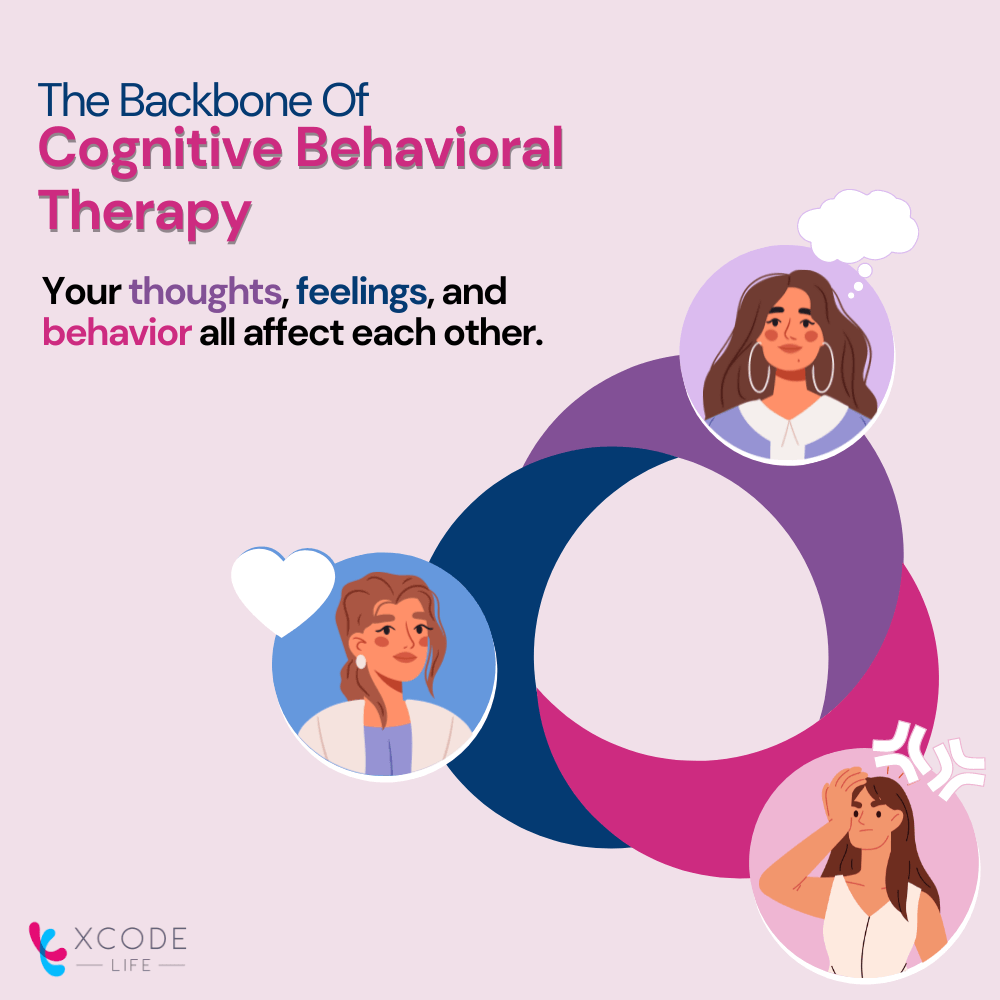
Cognitive Behavioral Therapy (CBT) is an effective therapeutic approach that addresses negative self-talk and its impact on mental health.
Through CBT, individuals can gain self-awareness and recognize how their thoughts influence their emotions and behaviors.
CBT focuses on identifying and challenging negative self-talk patterns.
By examining the underlying cognitive distortions contributing to negative thinking, individuals can reframe their thoughts and replace self-criticism with self-compassion.
Therapists work with individuals to develop realistic and compassionate self-talk, fostering a positive mindset.
CBT also incorporates behavioral changes to reinforce positive self-talk.
Individuals can break free from negative cycles and build confidence by engaging in new behaviors aligned with positive thoughts.
The integration of thoughts and actions creates positive momentum in life.
It is important to note that CBT is a personalized therapy process.
Each individual's experience of self-talk and the underlying causes of negative thinking may vary.
Collaborative efforts between the individual and therapist ensure that interventions are tailored to meet specific needs.
Self-talk is completely normal and common behavior.
It serves various functions throughout our lives, from childhood development to daily self-reflection and problem-solving.
The content of our self-talk significantly impacts our attitudes, performance, and emotional well-being.
Positive and instructional self-talk can increase focus, boost self-esteem, and improve task performance. However, negative self-talk, characterized by self-criticism and constant blame, can harm our mental health, leading to depression and anxiety.
Fortunately, cognitive behavioral therapy (CBT) offers effective techniques for addressing negative self-talk and promoting a positive mindset.
Individuals can reshape their self-talk patterns and enhance their overall well-being by challenging negative thoughts, fostering self-compassion, and aligning thoughts with positive actions.
So, the next time you find yourself engaged in a silent conversation with yourself, remember that it is a natural and valuable process.
Embrace the opportunity to cultivate positive self-talk, practice self-compassion, and use your inner dialogue as a supportive partner on your journey toward personal growth and well-being.
Imagine yourself on the field, giving your all in a grueling workout or an intense sports competition.
You push your body to its limits, struggling for peak performance and faster recovery.
In your pursuit of excellence, you may have heard whispers about the mystical powers of ice baths.
But what exactly are ice baths, and why do athletes swear by their benefits?
Join us on a chilling journey into the world of ice baths, uncovering their purpose, the science behind them, and how to create the ultimate ice bath experience.
Cold water immersion, commonly known as an ice bath, requires you to submerge your body in water with a temperature ranging from 12°C to 15°C for a specific duration.
Ice baths are a widely used recovery method among athletes due to their numerous benefits in muscle healing and overall wellness.
Ice bath session within 10 to 15 minutes is advisable.
But paying attention to your body's needs and changing the time to suit your comfort level is important.
Athletes may opt for shorter or longer durations based on their preferences and desired effects.
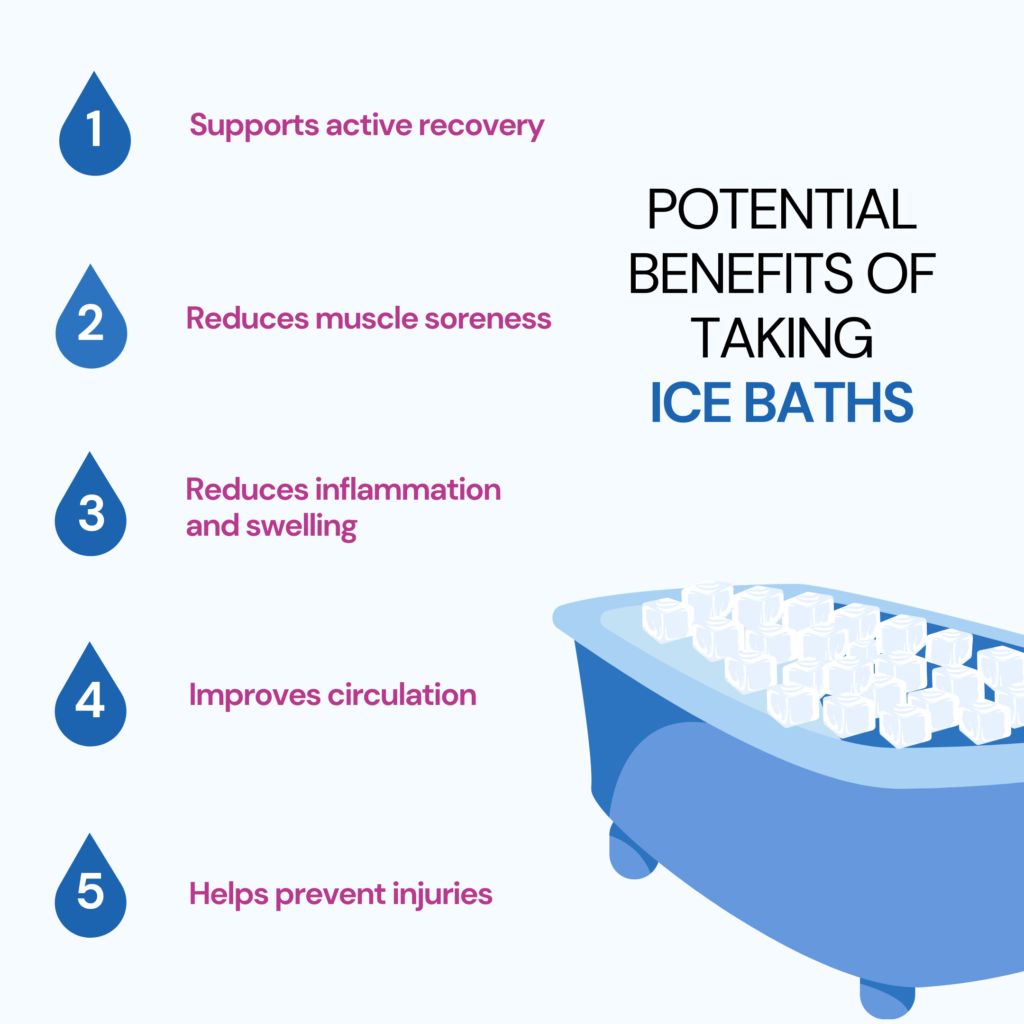
Ice baths provide several benefits and can significantly improve an athlete's performance.
We will now go through some of the benefits:
Over the past decade, significant research has focused on optimizing the recovery of elite athletes.
One recovery strategy that has received considerable attention is cold-water immersion (CWI).
Proposed mechanisms suggest that CWI may enhance recovery by reducing pain perception, altering blood flow, and decreasing muscle temperature.
However, the impact of CWI on inflammation and cellular stress in human skeletal muscle has been a topic of debate.
In a study conducted in 2015, researchers found prolonged CWI for a long time might reduce the body's ability to adjust to muscular training by decreasing signals that control inflammation.
Another study in 2016 showed that post-exercise CWI could benefit mitochondrial biogenesis and angiogenesis genes following high-intensity workouts.
However, these studies had different results, so more research is needed to understand the effects and best use of CWI as a recovery method.
More recently, a well-designed study by Peake and colleagues in 2017 compared CWI to active recovery after athletic training. Surprisingly, the study found no significant difference in the body's response to inflammation and stress between CWI and active recovery, challenging the traditional belief that CWI reduces post-exercise inflammation.
While CWI may have other benefits, such as reducing delayed onset muscle soreness, its impact on the inflammatory response requires careful consideration when implementing recovery strategies.
Athletes are increasingly using ice baths as a recovery method to improve their performance and speed up their recovery time.
In addition, ice baths have therapeutic and stimulating properties that offer a variety of advantages to athletes.
Some of them are:
While ice baths offer numerous benefits, it's essential to be aware of potential risks and exercise caution.
Here are a few risks associated with ice baths:
Ice baths are not just for athletes. Anyone can confidently include ice baths into their routine, whether an athlete, fitness enthusiast or seeking to enhance their recovery.
However, consulting with a medical professional before starting any new healing technique is advised, especially if you have pre-existing medical issues.
Creating the ideal ice bath experience involves a few key considerations:
A temperature range of 12°C to 15°C is appropriate for an ice bath to provide a safe and pleasurable cooling effect while minimizing the risk of hypothermia or frostbite.
However, monitoring water temperatures and keeping them within permissible levels ensures safety throughout sessions.
Scientific research has shown that ice baths can effectively reduce muscle soreness, inflammation, and swelling while improving circulation.
Athletes have found ice baths beneficial in enhancing their recovery and overall performance.
Ice baths provide athletes with a competitive advantage, helping them recover faster and minimize the risk of injuries.
While there are potential risks, such as frostbite and hypothermia, exercising caution and seeking professional guidance can mitigate these concerns.
Ice baths are not limited to athletes alone.
Non-athletes and fitness enthusiasts can also add them into their recovery routines, provided they consult healthcare professionals.
Have you ever experienced a day when it's difficult to remember something? Or concentrate on a task? As we get older, some cognitive slip-ups are normal.
But for others, these may hint at something more concerning.
In this piece, we'll delve into Alzheimer's, its causes, and symptoms and explore how breathing exercises might provide some defense against this condition.
Alzheimer's disease is a complex neurological condition.
It gradually (and irrevocably) alters the human brain. As a result, it is characterized by a progressive cognitive decline.
This decline manifests as memory loss and severe language difficulties, disorientation, and challenges with abstract thinking.
Alzheimer's often commences subtly, with minor lapses in memory or temporary confusion.
The early symptoms are easy to dismiss as normal aging.
However, as the disease advances, it becomes increasingly disruptive, affecting all facets of cognitive function.
The ability to perform routine tasks, recognize loved ones, and communicate effectively may gradually disappear.
The progression of Alzheimer's ultimately reaches a point where individuals require full-time care, which often leads to significant emotional and physical strain for caregivers.
For those who've witnessed a loved one grappling with Alzheimer's, the journey is deeply moving, sometimes distressing, and profoundly transformative.
It involves a gradual loss of the person they once knew, as the disease slowly erodes their unique personality traits, cherished memories, and eventually, their sense of self.
Alzheimer's stems from the build-up of beta-amyloid protein in the brain.
Amyloid-beta protein is a large membrane protein that plays a big role in neural growth and repair. The body produces it from a larger protein called amyloid precursor protein (APP).
The protein called APP is located on nerve cells. When enzymes break it down, it creates several fragments, including amyloid-beta.
This creates plaques that interfere with nerve cell communication.
As these plaques increase, they trigger inflammation and brain cell damage, leading to cognitive decline.
However, while this protein is often credited as a cause of Alzheimer's, many studies are still ongoing to identify the actual or other more prominent causes.
It's important to remember that the symptoms and signals mentioned are general and may not be applicable to everyone with Alzheimer's.
If you are worried that you or a loved one may have Alzheimer's, you should consult a doctor for a diagnosis.
Age, genetics, and lifestyle choices (like poor diet and sedentary life) are common risk factors for Alzheimer's.
However, the most significant factor in developing Alzheimer's and other cognitive problems is age.
As a person gets older, their chances of developing these conditions increase.
Similarly, our genes also play a crucial part in determining this risk.
Lifestyle factors, however, add a dynamic element to this equation.
While we can't turn back time or rewrite our genetic code, we hold the reins regarding these lifestyle choices.
By embracing a healthy diet, staying physically active, and avoiding smoking, we can wield substantial influence over our Alzheimer's risk, potentially steering ourselves towards a healthier cognitive future.
Harnessing our breath through specific exercises can profoundly impact our mental faculties.
Research points to lessened anxiety, improved focus, and overall cognitive enhancement.
It's akin to a gym session for your mind, ensuring mental agility.
So, what's the science behind this?
Breathwork activates the parasympathetic nervous system.
This system acts like an internal chill-out switch, reducing heart rate and blood pressure.
It makes us deeply relaxed, lowering brain inflammation and enhancing cognitive function.
A study in Scientific Reports, led by the University of Southern California researchers, delved into breathwork's potential impact on Alzheimer's.
They assembled 108 participants and divided them into two groups.
One group practiced slow-paced breathing for 20 minutes twice daily for a month.
The control group followed their usual routine.
Post-study results were intriguing.
The breathwork group showed a significant drop in blood levels of amyloid-beta peptides, a protein implicated in Alzheimer's development.
This group also demonstrated better memory test scores.
Please keep in mind that this study was relatively small.
More research is needed to validate findings across a larger set of populations. Yet, the initial results show promise.
They hint that something as uncomplicated as breathwork might help decrease Alzheimer's risk.
So, if you're concerned about Alzheimer's, consider integrating breath exercises into your routine. It's a straightforward, safe approach to better health, potentially offering a cognitive edge.
Breathing exercises can easily blend into your daily routine. You can practice many straightforward exercises anywhere, anytime.
To maintain a healthy brain, try these breathing exercises:
Put one hand on your chest and the other on your stomach. Slowly inhale through your nose; feel your belly expand. Then slowly exhale through your mouth; feel your stomach contract.
To perform this breathing exercise, sit comfortably with a straight spine and place your left hand on your left knee. Next, cover your right nostril with your right thumb while breathing through your left one. After that, close your left nostril with your ring finger and exhale from your right. Then again, inhale through your right nostril, use your right thumb to close it, and exhale from your left nostril. Repeat this cycle for several rounds.
Sit comfortably with a straight back and your feet flat on the ground. Breathe in deeply through your nose, counting up to four. Then hold your breath for four counts. Exhale through your nose for four counts. Hold your breath for four counts. Repeat this pattern for several rounds[^6^].
Breathing exercises have cognitive benefits and might reduce Alzheimer's risk. In addition, several studies have presented promising results showing that deep breathing exercises (like alternate nostril breathing and breath retention) can significantly cut amyloid-beta peptide levels. For example, one study involved 100+ participants assigned to a breathing exercise group or a control group.
While the study had limitations, it did offer quantified evidence that integrating simple breathing exercises into your daily routine might help lower the risk of Alzheimer's.
In all, breathing exercises are the easiest and most accessible way to support brain health that could benefit individuals of all ages, preventing the onset of diseases that are common with aging.
Did you know that within just 0.01% of your genome lies a wealth of information about your health, including your disease risk, optimal diet and exercise routine, skincare tips, behavior and personality, allergies, and drug sensitivities?
If you have done an ancestry genetic test with companies like 23andMe, AncestryDNA, MyHeritage, etc., you can unlock this information in just 3 steps.
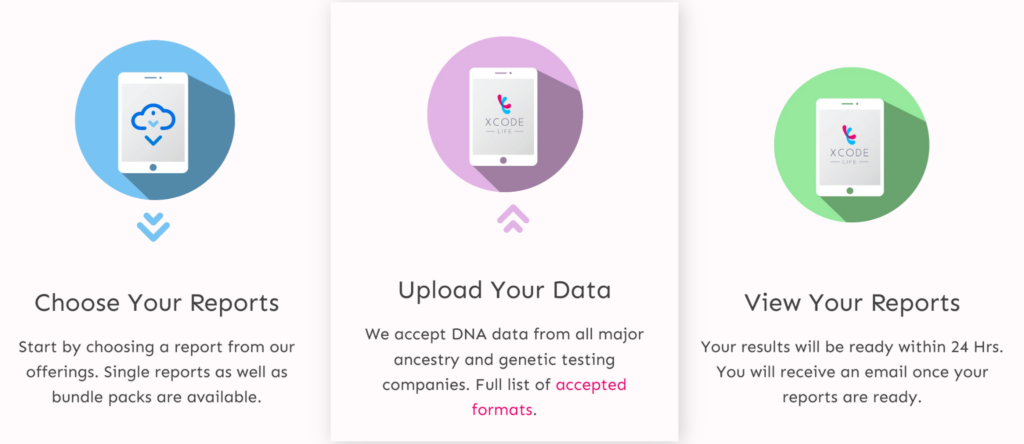
Even if you haven't received your ancestry test results, you can now purchase our reports at an unbeatable sale price.
Once you've made your purchase, the order remains safe with us, and you can upload your DNA data whenever you receive it.
Not yet tested?
If you're new to the world of genetic testing, we've got you covered!
You can now get your ancestry DNA kits at an additional discount!
By following the link provided in this article, you can purchase a DNA kit at 10% OFF (the discount will be reflected when you add the product).
This will ensure that you have everything you need to embark on your genetic journey.
Once you receive your kits, you can follow the instructions given by the respective service providers to collect your sample and ship it.
After you receive your DNA test results from the kit, follow the instructions provided here to upload your DNA data to our secure platform.
If you have not purchased the Xcode Life reports, you can check out our money-saving bundles here.
Ready to discover the key to lifelong good health? This insightful article delves into Life's Essential 8, a powerful checklist curated by the experts at the American Heart Association.
These essential pillars encompass all aspects of health and wellness, empowering you to make positive changes and live your best life.
From nutrition and physical activity to sleep and habits, we explore the key components contributing to your overall well-being.
Read on to gain valuable insights, practical tips, and actionable steps to start living healthier and happier lives.
The World Health Organization's definition emphasizes that good health is a total package - it involves not only freedom from illness or weakness but also a balanced combination of physical fitness and psychological/social well-being (WHO, 1948).
There is a direct connection between one's state of being healthy and their capacity for leading a productive life.
The lifespan refers to the complete duration of an individual's life.
At the same time, the health span relates to how long an individual stays healthy and free from illnesses.
Instead of believing that aging is beyond our control, we should focus on our daily lifestyle, which may lengthen our lives and make us more vibrant, healthy, and useful.
Scientific research indicates that genetic factors account for a whooping 20% of an individual's lifespan. Many environmental and lifestyle factors influence the rest. Some of them are:
The American Heart Association has identified Life's Essential 8 as the fundamental measure for enhancing and sustaining cardiovascular health.
By taking care of these key principles, individuals can significantly reduce their risk of heart disease, stroke, and other critical health issues.
Prioritizing cardiovascular health by implementing Life's Essential 8 is crucial to maintaining overall well-being and achieving a healthier lifestyle.
Here's how you can be healthy
It has been found that eating a healthy breakfast improves focus and attention, which helps achieve targets.
Including various fruits and vegetables in your diet, including apples, berries, oranges, and veggies like broccoli, sweet potatoes, beetroot, and okra, is recommended.
Limit the use of:
Including physical activity into daily routines, such as choosing to walk as a means of exercise or cycling as a mode of transportation, is an easy way for individuals to begin with.
Moreover, to enhance and sustain good heart health, it is advised to participate in moderate physical activity for at least 30 minutes daily or 150 minutes per week.
Below are some exercise suggestions that may help in improving your emotional state:
Tobacco contains chemicals such as nicotine that attract smokers. It can be quite difficult for individuals to detach themselves once they have become dependent. Therefore, quitting such behaviors may be very challenging. Fortunately, a few therapies have been used effectively to help smokers quit smoking.
Quitting smoking has been proven to bring many health benefits to an individual, including:
Recent research has shown the importance of getting enough sleep for a healthy immune system, metabolism, memory, learning, and other essential physiological functions to work properly.
Maintaining proper sleeping habits plays a key role in enjoying restful sleep. The term "sleep hygiene" refers to a group of regular activities that can either help or hurt an individual's ability to get a pleasant and refreshing night's sleep.
Just as good dental cleanliness is linked to excellent oral health, good body hygiene is related to overall physical health.
Similarly to this, practicing good sleep hygiene is associated with higher-quality sleep.
The consequences of insufficient sleep:
It is challenging to lose weight, and maintaining a healthy weight can be even more difficult. An individual's shape and how their clothes fit them are chosen by the distribution of fat and muscle across their body.
The current discussion focuses on practical methods for successfully controlling weight in a way that improves overall wellness and health.
Cholesterol is an oil compound with a wax-like consistency. Producing hormones, bile, and vitamin D are the metabolic processes dependent on it.
In the absence of any other risk factors, then it is recommended that individuals maintain a total cholesterol level below 5.5 mmol/L.
Individuals with cardiovascular risk factors, including hypertension, pre-existing cardiovascular issues, diabetes, or tobacco use, should strive to maintain LDL cholesterol levels below 2 mmol/L.
Irrespective of family history or previous cardiac problems, following a nutritious dietary plan, consistent engagement in physical exercise, and quitting smoking can prevent the development of increased cholesterol levels. In addition, sticking to a healthy body weight and restricting alcohol consumption may also have advantages.
Blood glucose level refers to the glucose levels in the bloodstream at a specific moment. Monitoring one's blood glucose level is crucial to managing one's health.
Typically, individuals measure their blood glucose levels before meals and during the night hours.
It is advisable to monitor your blood glucose levels during these scenarios:
Individuals who have been diagnosed with Type 1 diabetes must include daily insulin administration as a crucial part of their treatment plan.
Individuals with Type 2 diabetes can effectively control and lower their blood sugar levels by adopting a healthy diet and regularly engaging in physical activity. Lifestyle interventions, such as these actions, provide a practical approach to managing the condition.
To achieve maximum control over their blood glucose levels, individuals may need to undergo medical treatment and make certain lifestyle changes. This could involve taking hypoglycemic agents along with modifying their daily routine and habits.
Bodily events influence fluctuations in blood pressure during the daytime. While a rise in blood pressure is a normal response to physical and emotional stress, a decrease indicates relaxation. However, prolonged elevation in blood pressure may indicate a more severe problem. But making some lifestyle changes can help manage and reduce blood pressure. These changes include keeping a healthy weight, managing stress, eating well, and exercising regularly.
It's important to adopt these lifestyle changes and consult with healthcare professionals to address blood pressure concerns effectively.
A cardiac risk calculator helps predict an individual's possibility of experiencing a cardiac event within ten years.
The device evaluates cardiovascular health to estimate the possibility of developing atherosclerotic cardiovascular disease (ASCVD).
This can help in finding out the chance of:
Who doesn't need the use of a cardiac risk calculator?
Cardiac risk calculators can only be useful if you have yet to experience a heart event. For example, the information isn't helpful if you've had a heart attack, stroke, or heart failure.
What are the required inputs for a cardiac risk calculator?
The required inputs for a cardiac risk calculator are:
ASCVD risk calculator
The ASCVD risk calculator is a tool utilized to assess an individual's risk of developing atherosclerotic cardiovascular disease.
Healthcare providers utilize the American College of Cardiology (ACC) Atherosclerotic Cardiovascular Disease (ASCVD) Risk Calculator. The instrument evaluates the chances of an individual between the ages of 40 years and 79 years acquiring cardiovascular disease within the following decade.
The ACC and the AHA collaborated to create a dependable calculator for assessing the risk of heart disease. The AHA Cardiovascular (CV) Risk Calculator, available online, is a modified version of the ASCVD Risk Calculator designed to make fewer inquiries. Nevertheless, the results obtained are similar.
What is the approach for calculating the risk of cardiac events?
Cardiovascular risk assessment tools provide a numerical estimate of the chance of developing heart disease, expressed as a percentage. A decrease in percentage is associated with reducing the possibility of developing cardiovascular disease within a decade.
Various heart risk calculators categorize an individual's chance of developing cardiovascular disease as follows:
Low: Less than a 5% risk.
Borderline: A 5% to 7.4% risk.
Intermediate: A 7.5% to 19.9% risk.
High: More than a 20% risk.
Parameters Analyzed
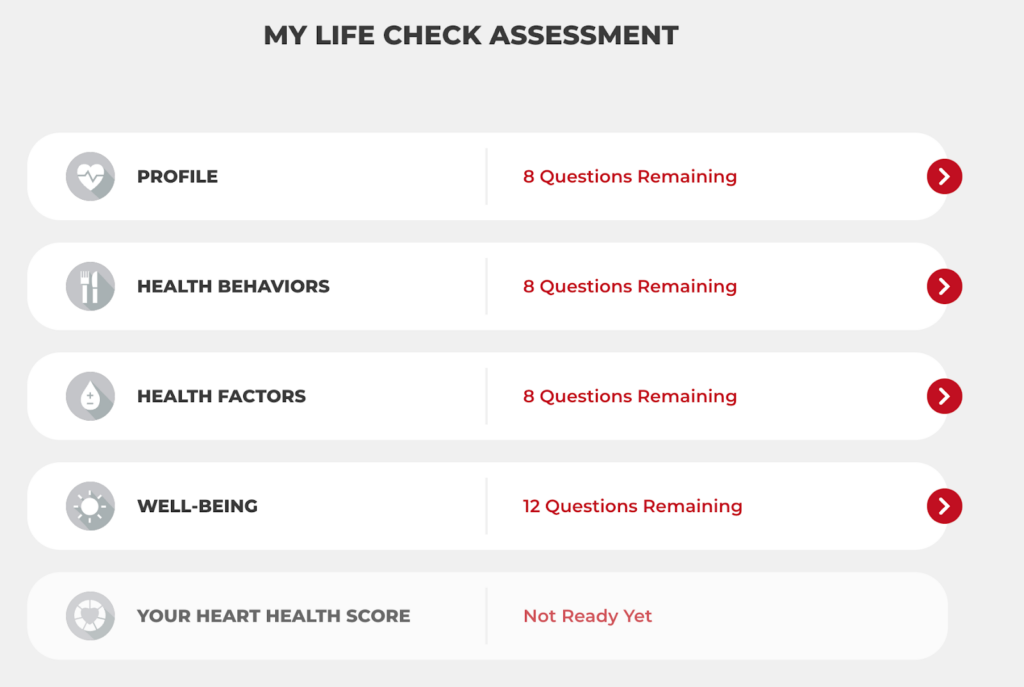
Image source: AHA website
Sample score
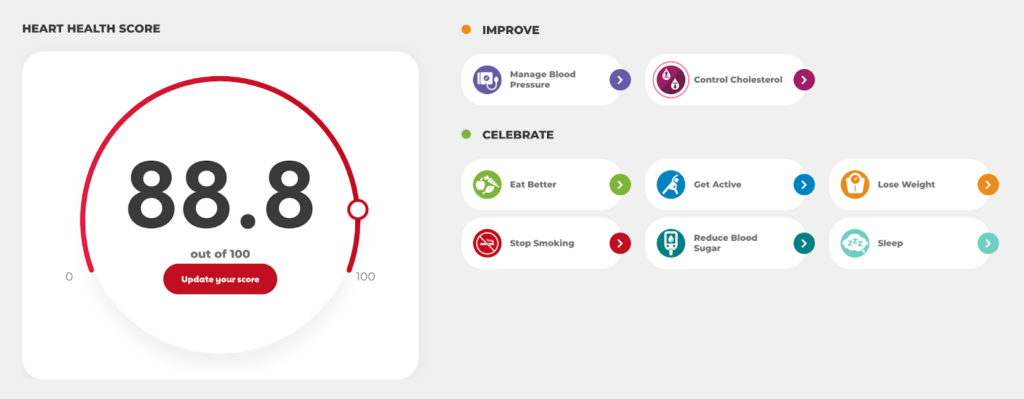
Image source: AHA website
Lifestyle changes are necessary to control several health factors, including body weight, cholesterol, blood pressure, and blood sugar levels.
A few key behaviors are needed to maintain a healthy lifestyle, including eating well, exercising, giving up smoking, getting enough sleep, and routinely checking your health.
The Life's Essential 8 checklist, curated by the American Heart Association, is a valuable guide for making positive changes and living healthier, happier lives.
Remember, small steps towards a healthier lifestyle can significantly impact long-term well-being.