Could a simple dietary change be the key to preventing prostate cancer?
Prostate cancer is a serious concern for many men, with over 200,000 new cases diagnosed annually in the United States.
A new study suggests that there may be a dietary solution to this problem - the Mediterranean diet. With its emphasis on fruits, vegetables, whole grains, and healthy fats, the Mediterranean diet has long been praised for its health benefits.
Researchers have found that following this diet may also help prevent prostate cancer. This article will examine the study's findings and what they could mean for men's health.
Your genes hold precious clues about your nutritional needs and dietary requirements. They influence how you respond to various diets, including the Mediterranean diet. Learn more:
The Mediterranean diet (MedDiet) is based on traditional food that people in countries like Greece, Italy, France, and Spain (along the Mediterranean coast) ate during the 1960s.
An American physiologist named Ancel Keys was the first to introduce the Mediterranean diet.
His most famous work was the Seven Countries Study, which highlighted how saturated fats and cholesterol levels increase Coronary Heart Disease (CHD) risk.
Until his lifetime, he championed the Mediterranean diet, promoting it for its health benefits.
In generic terms, this diet includes abundant fresh fruits and vegetables, whole grains, olive oil, and seafood and avoids processed food, sugar, saturated fat, and refined grains.
People living along the MedDiet are reported to enjoy a healthier and more active lifestyle. Nutritional experts attribute these benefits to their everyday diet style.
The Mediterranean diet is high in fiber, complex carbohydrates, and monounsaturated fats.
A typical MedDiet may contain the following elements.
| Foods | Serving frequencies |
| Olive oil | With every meal |
| Vegetables | 2+ servings with every meal |
| Fruits | 1-2 servings with every meal |
| Cereals and whole grains | 1-2 servings with every meal |
| Nuts | 1-2 servings with every meal |
| Seafood | 2+ servings/week |
| Legumes | 2+ servings/week |
| Red meat | Less than two servings/week |
| Poultry | Two servings/week |
| Sweets/desserts | Less than two servings/week |
When the MedDiet components are added to a food pyramid, vegetables, olive oil, whole grains, and seafood will top the charts.
Red meat, refined sugar, and processed foods would be at the bottom.
Heart Health
The MedDiet may support heart health and reduce cardiovascular disease risk.
A 2021 randomized controlled trial reports that long-term consumption of the MedDiet may help slow down plaque buildup in the arteries, bringing down the risk of heart attacks and strokes.
A 2022 review study reports that a MedDiet helps bring down the risk factors associated with cardiovascular diseases and also supports glycemic control.
Brain Health
A 2021 study reports that adhering to a MedDiet for an extended period increases gray matter volume in the brain, improves memory, and reduces the risk of cognitive decline.
A 2014 study analyzed the relationship between MedDiet adherence and the risk of developing Alzheimer’s Disease (AD).
Cortical thinning in the brain is associated with cognitive impairment and an increased risk of memory loss.
According to this study, individuals who adhered to a MedDiet regularly had a lower risk of cortical thinning, which may have a protective effect against AD.
Mental Health
The presence of high levels of omega-3 and omega-6 fatty acids and flavonoids in the MedDiet may help support mental health.
A 2019 Australian randomized controlled trial analyzed the effects of a MedDiet on people struggling with depression.
The participants were assessed for mental health improvement and quality of life after three months of following a MedDiet.
At the end of three months, the study reported reduced depression and improved quality of life scores in those who adhered to the diet plan.
A meta-analysis study reported that adhering long-term to a MedDiet may bring down the risk of depression by 30%.
Protection Against Cancers
The Mediterranean diet has been associated with a decreased risk of many types of cancers.
A 2021 meta-analysis analyzed the results of 117 studies involving 3,202,496 participants. The study reported that higher adherence to a MedDiet lowered cancer mortality risk.
This included liver, bladder, gastric, head and neck, colorectal, and respiratory cancers.
Weight Loss
MedDiet is a success among people wanting to lose weight because it isn’t as restrictive as other diets and has healthy and tasty food options.
A 2020 study reports that people who adhered to a MedDiet for a more extended period had a two-time increased likelihood of maintaining weight loss.
A similar 2022 study analyzed the ability of 470 adults to maintain their lost weight in 12 months while on MedDiet.
This study reports that higher adherence to the MedDiet was associated with a better likelihood of maintaining weight loss.
Blood Sugar Regulation
A systematic review analyzed the relationship between MedDiet and type II diabetes.
The review reports that MedDiet may help reduce fasting blood sugar levels and the three-month blood sugar average (HbA1c), thereby improving blood sugar regulation.
Prostate cancer is the second most common type of cancer in men (after skin cancer). The prostate is a small gland in men that produces semen fluid.
According to the National Cancer Institute, about 268,490 new prostate cancer cases were diagnosed in 2022.
The same source reports that about 12.6% of men in the United States will be diagnosed with prostate cancer at some point in their lifetimes.
Men may genetically inherit the risk of developing prostate cancer.
Apart from that, dietary and lifestyle habits may also influence the condition.
Consuming the following foods may increase people’s risk of developing prostate cancer.
A 2023 Australian study analyzed the effect of a MedDiet on prostate cancer and reported that people who adhere to the diet regularly have a lower chance of being diagnosed with prostate cancer.
CSIRO Human Nutrition and the Royal Adelaide Hospital conducted this case-controlled study.
It analyzed the lab reports of adult men diagnosed with prostate cancer and compared the values to a control group.
Study Participants
The study included 116 caucasian men diagnosed with prostate cancer.
The mean age of the participants was 71.24 ± 7.18
Study Design
The study design is based on the idea that the plasma concentrations of micronutrients and trace minerals would differ for healthy individuals and those with prostate cancer.
Plasma concentrations of the following values were measured in the control and the study groups.
The study reports that people with prostate cancer have lower levels of selenium (<120 mcg/mL), lycopene (<0.25 mcg/mL), and α-carotene compared to the control group.
People with prostate cancer also had higher plasma calcium, sulfur, and iron levels than the control group.
The study concludes that people with lower levels of selenium, lycopene, and α-carotene have a higher risk of prostate cancer.
Deficiencies of selenium, lycopene, and α-carotene may occur from a western diet lacking enough vegetables and fruits.
A MedDiet encourages the consumption of colorful veggies and fruits rich in lycopene and α-carotene and seafood, eggs, and nuts rich in selenium.
As a result, a MedDiet may be protective against prostate cancer.
If moving to a MedDiet seems overwhelming right away, here are some tips to get the diet started.
Apart from changing your diet, here are other ways to reduce the risk of developing prostate cancer.
In recent years, advancements in gene therapy have sparked hope for treating various genetic disorders, including cystic fibrosis, a life-threatening disease affecting thousands of people worldwide.
With the potential to provide a cure, gene therapy for cystic fibrosis has become an increasingly promising field of research, raising the question: could cystic fibrosis gene therapy finally offer a way to conquer this debilitating disease?
You may carry genes associated with inherited conditions and not develop the condition but may pass it to your children. Learn more:
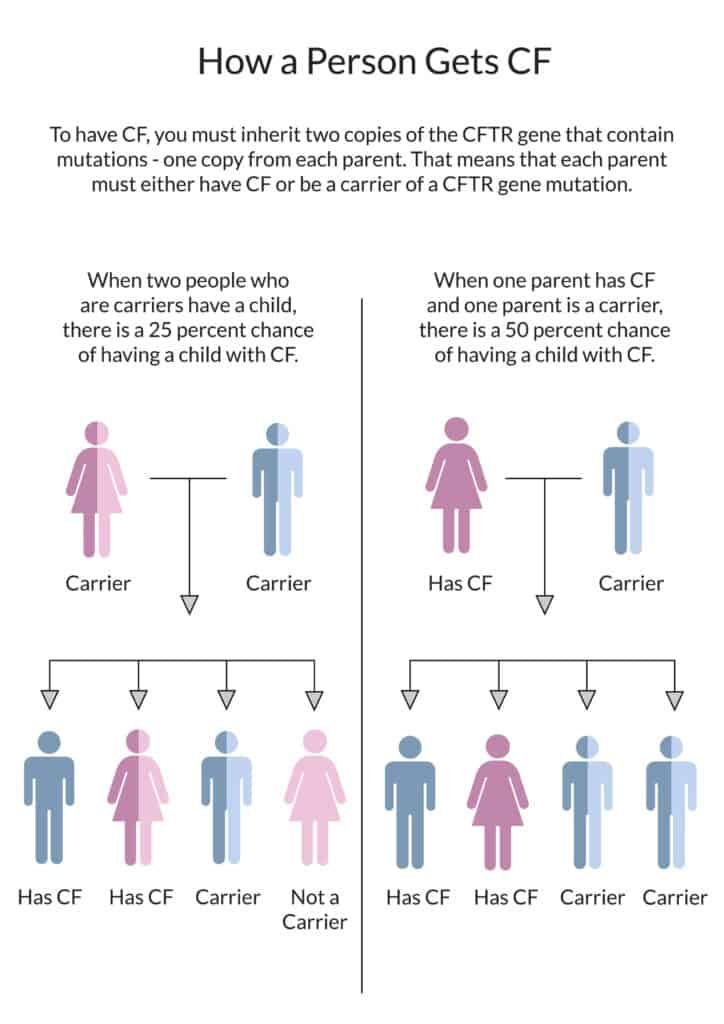
Cystic fibrosis is a genetic disorder caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene.
The CFTR gene contains the instructions for making the CFTR protein expressed in the airway epithelial cells.
When there is a mutation/change in the genetic instructions, the production or function of the CFTR protein may be affected.
The mutations in the CFTR gene can result in no protein, not enough protein, or the protein being made incorrectly.
Whilst the CFTR protein is expressed in many internal organs, the significant effect of such mutations is on the respiratory, gastrointestinal, and reproductive tracts.
The critical function of CFTR protein is ion transport (the movement of salt and water in and out of your cells).
Abnormal ion transport leads to thick viscous secretions in the airways, infection, inflammation, and eventually irreversible lung damage.
The lungs and digestive system become clogged with mucus, making breathing and digesting food hard.
There is currently no treatment that halts the natural progression of the disease.
All available successful therapies merely slow the rate of decline in clinical conditions.
Gene therapy offers great hope for the treatment of genetic diseases/disorders.
Gene therapy or gene transfer, or gene replacement, is a technique that modifies a person's genes to treat or cure disease.
Gene therapy can do the following:
Cystic fibrosis gene therapy works by placing a new, correct version of the CFTR gene into the cells in a person's body.
Two types of gene therapy have shown the potential to treat this condition.
In integrating gene therapy, a piece of DNA containing a functional CFTR gene would be delivered to an individual’s cells.
The new copy of the CFTR gene would then become a permanent part of their genome, which is the entire set of genetic instructions in every cell.
An advantage of integrating gene therapy is that it is permanent for the cell's life.
This means that a person with cystic fibrosis might have to receive gene therapy only once or a few times in their life.
A disadvantage is that there may be limited control over where the new copy of the CFTR gene integrates into the genome.
This means integrating gene therapy could have undesirable side effects, such as increasing cancer risk.
In non-integrating gene therapy, a piece of DNA with a correct copy of the CFTR gene is provided to an individual's cells.
Here the DNA remains separate from the genome and is not permanent.
Even though the newly introduced gene does not become part of the genome, the cell can still use the new copy of the CFTR gene to make normal CFTR proteins.
A major advantage of the non-integrating gene therapy approach is that it does not disrupt the entire genome.
That means the risk of side effects, including cancer, is low.
A disadvantage of non-integrating gene therapy is that it is not permanent.
The effect of the gene therapy might last only for several weeks or months and need to be treated repeatedly for it to be effective.
Over 360 variants or changes in the CFTR gene can cause the condition.
Recently, these variants have been categorized into seven classes based on CFTR protein dysfunction and/or gene expression.
Gene therapy for cystic fibrosis is done by replacing the genetic mutation with a “correct version” of the CFTR gene.
Although the mutant copies of the CFTR gene would still be there, the correct copies would allow cells to make normal CFTR proteins.
An integrating gene therapy known as CAR-T therapy has already been approved to treat patients with a few types of leukemia and lymphoma.
Several gene delivery methods exist to introduce a therapeutic gene or gene targeting.
CF gene therapy research has tested both non-viral and viral delivery vectors.
Scientific breakthroughs in the past ten years have accelerated advances in gene therapy.
Integrating gene therapies to treat CF is being tested in the lab, and a clinical trial to test the safety of this approach in people with CF could happen in the next several years.
Despite these advances, currently available drugs do not treat around 10% of CF patients.
It has also been found that existing CTF modulators are not well tolerated by eligible patients, causing many of them to stop treatment midway.
Gene therapy comes with a set of challenges that need to be overcome for the process to be effective.
Some of them include the following:
Happy World Sleep Day!
Sleep is considered a luxury these days. Most of us are lucky if we get at most 5-6 hours of sleep. We rarely pay attention to this. Understandably, working to pay our bills looks more important than a good night's sleep.
Sleep is one of the three pillars of health. Unknown to us, our body depends on the time we sleep to get a lot of background metabolic processes, like detoxification, out of the way.
Furthermore, recent studies suggest that poor sleep can significantly affect your ability to make healthy food choices and stay on track with your fitness goals, making it all the more important to prioritize a good night's rest.
Getting 7-9 hours of sleep every 24 hours is essential.
Poor sleep, which includes short sleep duration, difficulty falling asleep, sleep apnea, continuously waking up at night, etc., can impact your health negatively.
Insufficient or poor quality sleep can increase the risk of several chronic health conditions like heart disease, diabetes, obesity, depression, hypertension, kidney disease, and stroke.
It can also impact your cognitive ability by interfering with memory, attention, brain function, and alertness.
Sleep deficiency is also linked to injury risk in adults, teens, and children.
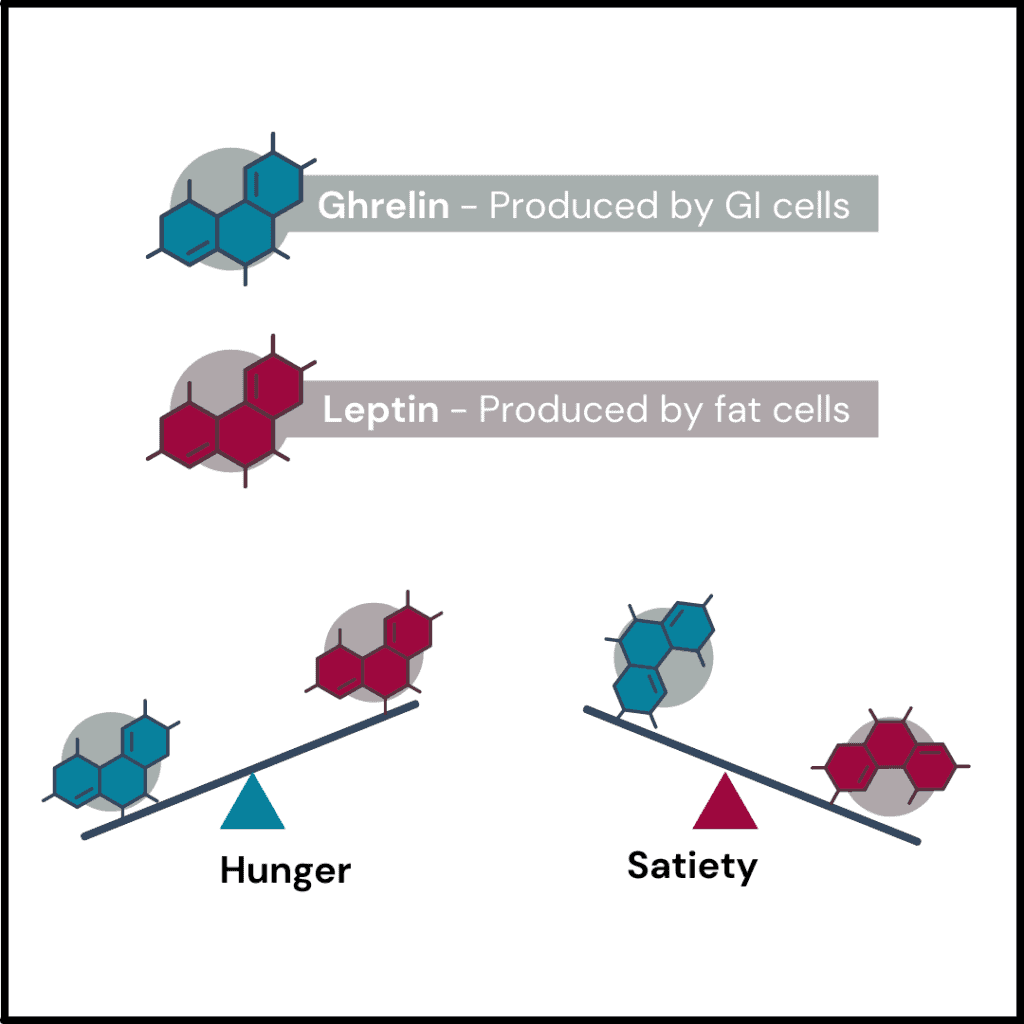
Sleep plays a critical role in regulating our appetite and eating behaviors.
Several studies have shown poor sleep can interfere with hormones controlling hunger and satiety.
This can lead to overeating and increase the risk of obesity.
For example, ghrelin is an appetite-regulating hormone that signals to the brain that you are hungry and your body needs food.
Lack of sleep can increase the ghrelin hormone levels, making us more hungry than usual.
Furthermore, it can decrease the levels of another hormone called leptin, which signals the feeling of fullness to the brain, thereby suppressing appetite.
Increased levels of ghrelin and decreased levels of leptin can lead to overeating.
Poor sleep also affects what food we pick to eat.
Studies have shown that sleep-deprived people tend to go for unhealthy foods that are high in calories over nutritious foods.
Overall, poor sleep can lead to overeating and poor nutritional choices, leading to weight gain and several other chronic diseases.
A lack of sleep or poor quality sleep can lead to fatigue and lethargy, making it harder to feel motivated to exercise.
According to a study, adequate sleep helps motivate people to stick to the exercise routine.
In this study, the more sleep participants got, the more likely they were to complete the exercise regimen.
Sleep deprivation can result in earlier onset of exhaustion, leading to a lower tolerance for physical activity.
Since sleep is crucial for the body’s repair and recovery processes, sleep deprivation can lead to decreased physical performance and increased injury risk.
Sleeping well supports our body’s recovery process, helping us feel more energized.
This can help us stay motivated and achieve our fitness goals.
A preliminary research study presented at the American Heart Association's Epidemiology, Prevention, Lifestyle & Cardiometabolic Health Scientific Sessions 2023 examined how sleep quality and behavior affect a person’s diet and exercise patterns.
The researchers designed a 12-month weight loss program to examine whether good sleep health made people adhere to weight loss-related lifestyle modifications better than bad sleep health.
| No. of participants | 125 adults |
| Average age | 50 years |
| Sex | 91% female |
| Race | 81% male |
| BMI | 27-44 (overweight/obese) |
| Pre-existing health conditions | None |
Participants sleep habits were measured three times during the study period:
Tools like questionnaires, sleep dairy, and reading from wrist-worn devices were used to measure sleep habits.
Upon measuring the score, the researchers scored each participant from 0-6, with higher scores falling under the “good” criterion and lower scores under the “poor” criterion, based on six criteria:
Adherence to the weight loss program was measured by:
The average sleep health score of the participants in the study period was 4.5 out of 6.
At the end of the study, the researchers observed that the participants who scored higher in sleep health were more likely to attend group sessions and stick to their caloric intake goals.
First six months
Last six months
The decrease in the metrics observed in the last six months was expected, says one of the authors, Kline.
The adherence to weight loss behaviors tends to taper as one continuous in a long-term intervention.
Further, there was an association between better sleep health scores and increased physical activity. But the results were statistically insignificant.
The study results suggest that optimizing sleep can lead to better adherence to weight loss-related lifestyle modifications.
While there are many ways to improve your sleep and fix your sleep cycle, three of the most effective ones are:
Your sleep habits affect what you eat and your exercise behavior via several physiological modifications.
Poor sleep can increase the hunger hormone and decrease the satiety hormone levels, making you overeat and gain weight.
If you don’t get enough rest, it can result in persistent fatigue and inadequate repair, leading to injuries and a lack of motivation to exercise.
According to a recent study, people who slept better were more likely to adhere to weight loss interventions and their caloric intake goals.
Genetically inherited diseases are always challenging to diagnose, treat, and cure. One such rare yet, complex condition of the eye is Retinitis Pigmentosa (RP). People with RP have minimal treatment options and lose vision entirely over time.
Thanks to advances in gene therapy, such individuals may have hopes on the horizon. RP clinical trials aimed at finding a standard treatment option for the condition, thereby improving the quality of life for the patients.
This article helps identify such promising Retinitis Pigmentosa treatment trials of 2022 and discusses their potential results.
You may carry genes associated with inherited conditions and not develop the condition but may pass it to your children. Learn more:
RP is a genetic condition affecting the retina, causing loss of night vision and vision over time. The signs usually start from childhood, and this condition can affect the quality of life.
The fact that no standard treatment processes are in place makes this a topic of interest for researchers globally.
This article will take you through the existing and proposed Retinitis Pigmentosa treatment in 2022 and shed light on current research advances.
RP is a group of conditions that affect the retina of the eyes and is passed genetically.
Approximately 1 in 4000 Americans develop RP in their lifetimes. RP is primarily bilateral (affecting both eyes). However, in rare cases, the condition can be unilateral (involving a single eye).
There are two types of RP identified.
RP is characterized by damage to the light-sensitive cells in the eyes called photoreceptors.
The first sign of RP is night vision loss, and this begins by the age of 10-20. Eventually, tunnel vision develops; by age 40, the person can lose eyesight completely.
About 50 different genes may lead to Retinitis Pigmentosa.
Multiple clinical trials explored Retinitis Pigmentosa treatment options in 2022. Many of these trials are still in progress, trying to find a standard treatment for the condition.
The following are some of the popular research advances to be aware of.
Prodygy Phase 1/2 Clinical Trial
SparingVision is a genomics company based out of Paris, France.
At the end of 2022, the brand announced that the Food and Drug Administration (FDA) had approved its application for a new therapy using SPVN06 to help treat RP.
Since the approval is in place, the company can initiate the Promising Rod-Cone Dystrophy Gene Therapy (PRODYGY), a first-in-human clinical trial (phase I/II) for RP.
What is the PRODYGY trial?
The Prodygy study was one of the significant RP news in 2022.
This trial will analyze the safety, efficacy, and treatment progress of the SPVN06 injection in RP patients with a mutation of the RHO, PDE6A, or PDE6B genes.
The trial plans to recruit 33 patients with RP for the study. After 12 months, the patients will go through a follow-up study, analyzing the safety and tolerability of the injection.
The study also plans to perform a long-term follow-up after five years to check the drug's quality of life and safety.
Optogenetics involves adding light-sensing molecules called opsins to the retina to the retina's photoreceptor cells to improve vision.
Optogenetic therapy was one of the most explored treatment options for RP in 2022.
In 2021, Nanoscope Therapeutics Inc., a biotechnology company based out of Dallas, Texas, conducted a Phase 1/2a optogenetic clinical study to analyze the effects of Multi-Characteristic Opsin (MCO-010) on visual restoration in 11 patients with RP.
After eight weeks of treatment, all patients experienced improved vision restoration and better quality of life.
Following this success, the company announced a Phase 2b trial in 2022 that recruited 27 individuals with advanced RP and severe vision loss to analyze the effects of MCO-010 injections on their vision.
The trial results are yet to be released, and you may be able to check the RP treatment updates sometime in 2023.
NAC Attack is a clinical trial exploring oral N-acetylcysteine (NAC), an antioxidant, in restoring vision and treating RP.
This Phase III clinical trial is sponsored by John Hopkins University. About 438 participants will participate in the study, and the trial will be conducted in approximately 30 centers across the USA and Europe.
Phase I of this trial found a small but significant improvement in vision and light sensitivity with oral NAC for six months.
The Phase III of this trial is set to be completed in March 2028.
Up until 2022, the only accepted treatment for RP one is Luxturna.
This is a gene therapy solution for people with the RPE65 gene mutation.
There are no accepted treatment options for other RPs with different gene mutations.
Since multiple genes are associated with RP, finding gene therapies for each one of these mutations is going to be an expensive and time-consuming affair, which, however, must be done.
Some of the other clinical trials currently in progress for RP include the following.
How Much Does Retinitis Pigmentosa Gene Therapy Cost?
Right now, the only approved gene therapy treatment for RP is Luxturna. This is developed and marketed by Spark Therapeutics.
This one-time treatment will cost $425,000 for one eye or $850,000 for both eyes.
How soon will there be a cure for RP? This is a question in everyone’s mind.
Multiple clinical trials have been conducted to help understand the condition better and explore standard and safe treatment solutions.
So, there is definitely hope on the horizon for people with RP. As these clinical trials progress further, researchers may be able to find a standard treatment option for RPs caused by different gene mutations.
Certain genetic tests may help confirm the presence of Inherited Retinal Diseases (IRDs).
These tests can help you know if you are a carrier of specific gene mutations that may cause RP and other IRDs and take proactive steps.
Recent studies have shown that almost all women diagnosed with breast cancer are also vitamin D deficient. In this article, we explore the science behind this link, the impact of vitamin D on breast cancer risk, and what women can do to boost their vitamin D levels and potentially reduce their risk of developing this disease.
The Recommended Dietary Allowance (RDA) of vitamin D
| Age | Female | Male |
| 0-18 years | 15 mcg (600 IU) | 15 mcg (600 IU) |
| 19-70 years | 15 mcg (600 IU) | 15 mcg (600 IU) |
| >70 years | 20 mcg (800 IU) | 20 mc (800 IU) |
| Pregnancy | 15 mcg (600 IU) | |
| Lactation | 15 mcg (600 IU) |
The body can make vitamin D from direct sunlight when outdoors.
It is also obtained through food sources like oily fish, egg yolks, red meat, mushrooms, and fortified cereals.
The link between vitamin D and breast cancer risk revolves around the VDR gene.
This gene produces a protein called the vitamin D receptor, to which the active vitamin D binds.
Mutations or changes in this gene affect vitamin D levels in the body.
According to a research review, the same changes in the VDR gene were found to increase breast cancer risk.
Many studies supporting this link have reported that many people were vitamin D deficient when diagnosed with breast cancer.
A review published in The Breast reported that up to 96% of breast cancer patients are deficient in vitamin D.
Further, some studies also suggest that low vitamin D levels are associated with a higher risk for breast cancer recurrence and metastasis.
According to a year-long study, those with the highest levels of vitamin D had the most drop in estrogen levels.
Vitamin D deficiency can lead to estrogen dominance.
This study suggests that vitamin D can be an alternative to estrogen-lowering drugs.
Low vitamin D levels are associated with a higher risk for breast cancer.
This sunshine vitamin helps regulate breast cell growth.
There’s also a direct association between vitamin D and a gene involved in tumor growth and spread called ID1.
According to a study, circulating vitamin D levels are inversely associated with ID1 protein levels.
Thus a vitamin D deficiency may favor breast cancer cell growth.
There’s no one foolproof way that guarantees breast cancer prevention.
However, by meeting your vitamin D requirements, it is possible to lower your risk for breast cancer.
According to a 2015 study, women or people assigned female at birth who are deficient in vitamin D had a 27% higher risk for breast cancer than those with adequate vitamin D levels.
Another pooled analysis reported that a serum 25(OH)D level of 47 ng/ml was associated with a 50% lower risk of breast cancer.
Thus, meeting your vitamin D needs can help significantly reduce breast cancer risk.
10-30 minutes of midday sunlight several times a week, along with a dietary intake of more than 400 IU of vitamin D/day, can help reduce breast cancer risk and recurrence.
Though sun exposure and diet are excellent sources of vitamin D, most people can’t get enough of this vitamin.
Due to various reasons like latitude, skin tone, and lifestyle, adequate sun exposure for our bodies to synthesize vitamin D doesn’t happen.
Further, not all countries have dairy products fortified with vitamin D.
In these situations, a high-quality vitamin D supplement can help you be vitamin D sufficient.
Disclaimer: Vitamin D supplements are not advised to be taken without a doctor’s advice. Consult a qualified practitioner for dosage recommendations.
Vitamin D plays a role in regulating breast cell growth.
Changes in the VDR gene that increase vitamin D deficiency risk also seem to increase breast cancer risk.
Further, lower vitamin D levels are associated with higher protein levels that play a role in cancer cell growth and spread.
Adequate sun exposure, fortified foods, and a quality D3 supplement are effective ways to meet your vitamin D needs.
Disclaimer: This blog post is for information purposes only and must not be taken as medical advice. Please consult a qualified medical practitioner for appropriate treatment.
As if menstrual cramps and bloating weren't enough, for many women, migraines can also strike during their period. But why exactly does this happen? A new study has shed light on the matter, revealing some fascinating insights into the link between hormones and headaches.
Hormonal headache is linked to hormonal fluctuations in the body.
They are most commonly associated with changes in estrogen levels, which occurs during the menstrual cycle, pregnancy, and menopause.
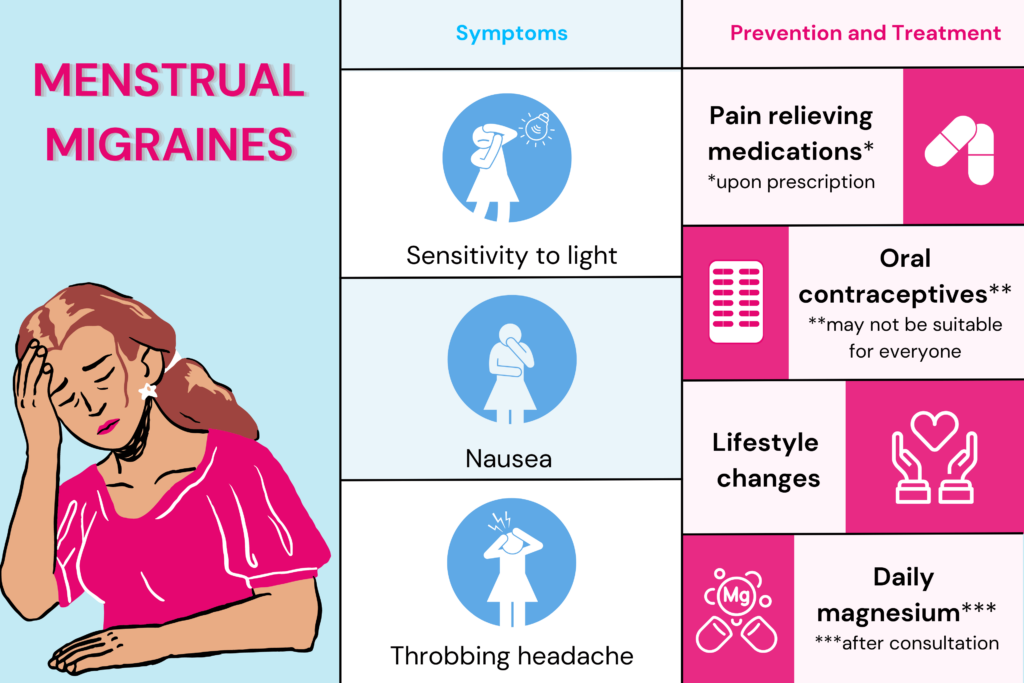
Hormonal headaches range from mild to severe and can often be accompanied by other symptoms such as nausea, sensitivity to light or sound, and fatigue.
Women are more likely than men to experience hormonal headaches and often find their headaches more frequent or severe during certain times of the month.
Menstrual migraine is a specific type of hormonal headache that occur in women in the days leading up to or during their period.
These migraines are often more severe and longer-lasting than a typical migraine.
Symptoms include nausea, vomiting, and sensitivity to light and sound.
The exact cause of menstrual migraines is not fully understood, but it is believed to be related to changes in estrogen levels.
As estrogen levels drop before and during menstruation, it can trigger the release of certain chemicals in the brain that can cause migraine.
Women who experience menstrual migraines may benefit from tracking their menstrual cycle.
A study published on February 22, 2023, in the online issue of Neurology explored the cause behind attacks experienced by cisgender women during periods.
Study Participants
Three groups of 30 (total of 90) cis-gendered women with episodic migraine was considered for this study.
They all experienced migraines for at least three days in the month before the study.
The group included those with regular menstrual cycles, those on oral contraceptive pills (OCPs), and those who had gone through menopause.
Three groups of 30 cis-gendered women, each without migraines, were considered for reference.
Study Design
The researchers measured the levels of a protein called CGRP (calcitonin gene-related peptide).
When CGRP is released, it results in the inflammation of the protective layer of the brain called the meninges.
This can result in a migraine attack in some.
To measure CGRP levels, the researchers collected blood and tear fluid samples.
The samples were collected around ovulation time (CGRP levels highest) in those with regular menstrual cycles.
For those on OCPs, sample collection was done during hormone-free and hormone-intake time.
Sample collection was at random times for those who attained menopause.
For those with migraines and regular menstrual cycles, CGRP levels were higher during menstruation than those with migraine - 5.95 pg/ml in the former group and 4.61 pg/ml in the latter group.
For those on OCPs and those who attained menopause, the CGRP levels weres similar between the migraine and non-migraine groups.
The increase in CGRP levels following estrogen fluctuations can help explain why migraines are more likely to occur during periods and why the attacks decline post-menopause.
Accurate blood measurement of CGRP levels is challenging due to its short half-life.
CGRP measures through tear fluid are non-invasive but still exploratory.
The hormone levels were considered around ovulation time; however, they may not have been taken on the exact day of ovulation.
So the full extent of estrogen level fluctuation may not have been captured.
There are several strategies that women can use to help prevent and manage period migraines.
Triptans are a type of specific painkiller for migraine. They work by calming down overactive pain nerves.
Nonsteroidal anti-inflammatory drugs, or NSAIDs, like naproxen, can also be used to get relief from pain.
NSAIDs are also used as prophylactic drugs - to prevent pain by taking the tablets at a prescribed dose for up to 5-6 days before periods.
Some research suggests that oral contraceptives may reduce the frequency of menstrual migraines.
However, this doesn’t apply to all OCPs, and not everyone may experience the benefit.
It is also essential to discuss with your doctor any personal risk factors you may have for taking OCPs, as they can affect different women with migraine differently.
Much research suggests that regular exercise, especially aerobic exercise, can help prevent migraine headaches. HIIT and yoga can help too.
However, over-exertion could also be a trigger for migraines.
A regular sleep schedule, which includes clocking in 7-9 hours of daily sleep, can have magical effects on migraine in terms of reduced frequency, intensity, and duration.
Daily oral magnesium supplement has been proven effective in preventing menstrual migraines, especially for those who experience migraine before their periods.
The mechanism behind how magnesium plays a role in preventing migraines is still hazy. Some scientists theorize that magnesium may help decrease neuronal firing.
The healthcare practitioner can decide the type and dosage of magnesium.
Please do not start any nutritional supplements without a consultation.
Techniques like guided meditation, breathing exercises, and yoga flow to relax muscles can help reduce stress, which is a common trigger for menstrual migraines.
Working with a healthcare provider to develop a personalized treatment plan for menstrual migraines is essential, as the best approach may vary depending on the individual.
Additionally, tracking menstrual cycles and migraine symptoms can help identify patterns and potential triggers, making it easier to prevent migraines before they occur.
A new study sheds light on the cause of menstrual migraines.
The study reports that levels of a protein called CGRP that plays a role in inflammation in the brain are higher in those experiencing menstrual migraines.
Women can make lifestyle changes, avoid triggers, use medications, consider hormonal therapy, and try alternative therapies such as acupuncture or relaxation techniques to prevent and manage menstrual migraines.
Work with a healthcare provider to develop a personalized treatment plan and track menstrual cycles and migraine symptoms to identify patterns and potential triggers.