Researchers have identified a number of genes associated with gallstone disease.
In the sample report below, we've attempted to analyze some important genes that increase the risk for gallstone disease.
You can identify your genetic risk of Gallstones by using your 23andMe DNA data and placing an order for the Gene Health Report.
Gallstones are common, with around 20% of the population affected. Many people wonder if gallstones are hereditary. The answer is not clear-cut, as many factors contribute to the formation of gallstones. However, some studies suggest a genetic predisposition. While more research is needed in this area, it is possible that gallstones may be passed down from generation to generation.
The gallbladder is a small, pear-shaped organ in the upper right abdomen, just below the liver.
The gallbladder's primary function is to store and concentrate bile, a yellowish-brown digestive fluid produced by the liver.
Bile salts help break down fats in the small intestine during digestion.
Gallstones are hardened deposits of digestive fluid that can form in your gallbladder.
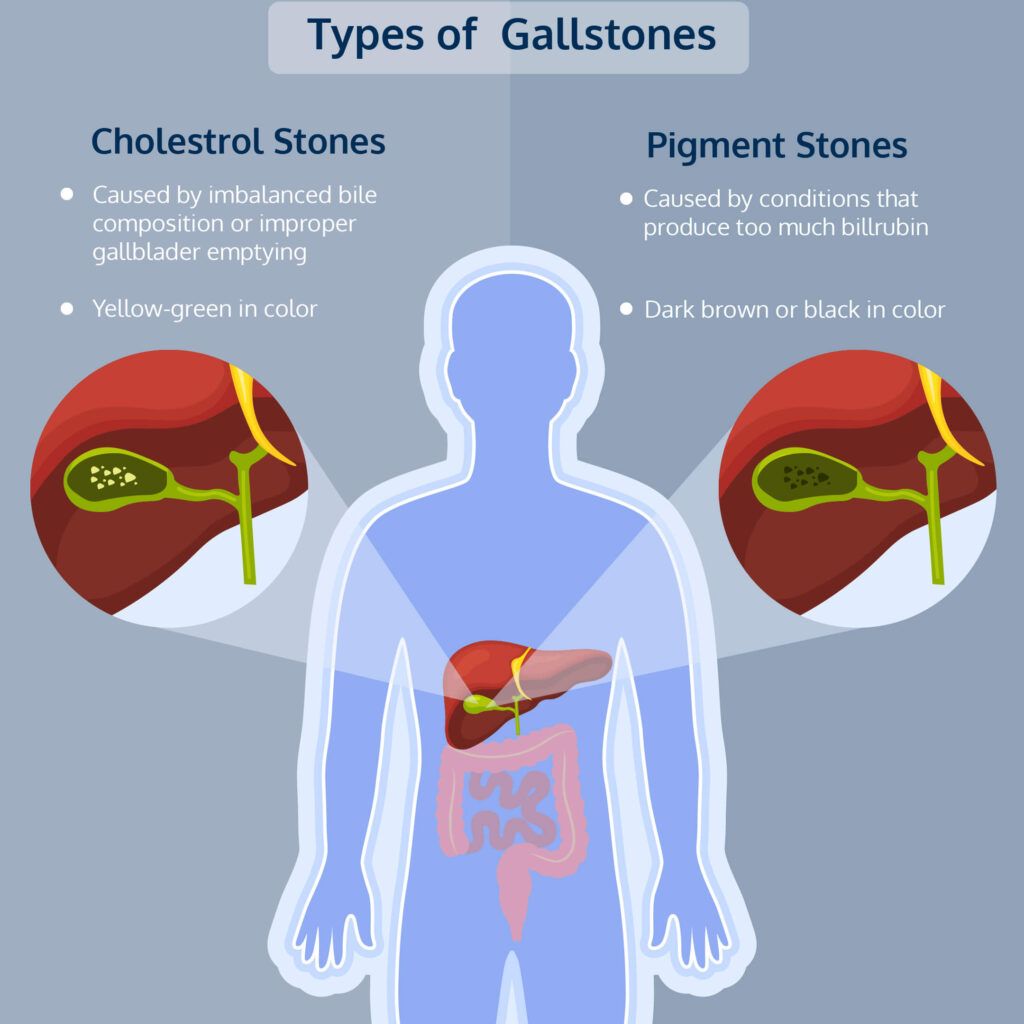
Too much cholesterol, bile salts, or bilirubin (bile pigment) can cause gallstones.
Gallstones range in size from as small as a grain of sand to as large as a golf ball.
Some people develop just one large stone, while others develop many smaller stones.
What causes gallstones is still in the grey, but experts suggest 3 contributing factors.
Too much cholesterol in the bile: Cholesterol, when present in normal amounts, is digested by the chemicals in the bile. But if the lives secrets excess cholesterol, it may crystallize, resulting in gallstones.
Too much bilirubin in the bile: Bilirubin is a yellowish pigment produced during red blood cell breakdown. Certain conditions like liver cirrhosis result in excess production of bilirubin, which can cause gallstones.
Incomplete emptying of the gallbladder: If the gallbladder doesn’t empty correctly, the bile can become concentrated, resulting in gallstones.
Most people with gallstones have no symptoms.
However, if a stone gets stuck in the bile duct causing, it can cause pain in the upper abdomen or back between the shoulder blades.
The pain may be severe and come on suddenly.
Other symptoms may include:
If you have these symptoms, you should see your doctor.
They can do tests to find out if you have gallstones.
Treatment may help if you have pain or other problems from the stones.
According to published research, the risk for developing gallbladder diseases, including gallstones, run in families.
This underlines a genetic link.
Studies have identified a mutation in the gene that regulates cholesterol transport from the liver to the bile duct that can increase gallstone risk.
Mutations in other families of genes can cause defective proteins leading to higher levels of cholesterol or bilirubin.
It is not necessary that having a relative with gallstones means you or any other family member will develop it.
Having said that, it can serve well to be on the lookout for symptoms and follow a healthy diet.
Conditions like obesity, Crohn’s disease, or irritable bowel syndrome running in families can increase the risk for gallstones.
Women or people assigned female at birth (AFAB) are twice as likely as men to develop gallstones.
This risk increases further in those who are pregnant or are under hormone replacement therapy.
Too much estrogen can increase cholesterol in the bile and lessen gallbladder movement.
Gallstones occur up to 10 times more frequently in the older population, especially those over 60.
The highest risk for gallstones is in the Native American population (30-70%), and the lower risk is in Asian and African populations (less than 5%).
People who are overweight or obese are at increased risk for gallstones.
This is because excess weight can cause the overproduction of cholesterol.
Low-fiber, high-fat diet can increase gallstones risk.
Overconsumption of heme-rich food can also cause gallstones.
Messenger RNA (mRNA) is a molecule that helps "read" the genetic instructions of a gene and convert them into a protein. Proteins are the building blocks of all living things, so mRNA plays a vital role in synthesizing proteins. Without mRNA, proteins could not be made, and life as we know it would not exist.
mRNA are molecules that exist in all the cells of our bodies.
Unlike double-stranded DNA, RNAs are single-stranded.
Using DNA as a template, mRNA is made through the process of transcription.
mRNAs are the only type of RNA from which proteins can be made, thus making them as essential as DNA.
Transcription is the process of making an RNA copy using a DNA strand as a template.
Transcription is like translating a book from one language to another - a universal biological language that the cellular machinery can use to assemble amino acids and form proteins.
The synthesized mRNA is chemically similar to DNA except for a base change.
Instead of T (Thymine) in DNA, we have U (Uracil) in RNA.
mRNA is much smaller than DNA and is far less stable.
It has a very short half-life (from seconds to minutes or hours) compared to that of nuclear DNA (years)
Without mRNA, the human genetic code, the DNA, is 1.8 meters of junk.
The mRNA acts as an intermediary between the genetic information in DNA and the amino acid sequence of proteins.
Each mRNA carries instructions to make a specific protein.
These instructions are like a “blueprint.”
mRNA delivers these instructions, and cells put the protein together.
Translation involves decoding the letters of the mRNA strands to form chains of amino acids, called polypeptide chains.
The polypeptide later folds into an active protein and performs its functions in the cell.
mRNA also contains multiple regulatory regions that can determine the timing and rate of translation.
Two molecules called ribosomes and tRNAs are involved in translation.
The tRNA carries along with it an amino acid that will later become a part of the protein.
The ribosome provides a surface where tRNA can bind to the mRNA
Source: Wikipedia
Image: mRNA Translation into Proteins
Any abnormal changes in the DNA can lead to the transcription of defective instructions.
This can lead to insufficient or excess levels of a particular protein. It can also result in the production of abnormally functioning proteins.
Such defects in proteins can cause serious genetic disorders.
Over 200 diseases are associated with defects in pre-mRNA processing to mRNA.
*Pre-mRNA is the first form of RNA created through transcription.
The mRNA molecule transfers a part of the DNA code to various parts of the cells to make proteins.
DNA-based therapeutics must enter the nucleus to be transcribed into the RNA for the medication to work.
In contrast, mRNA-based therapeutics don’t need to travel to the nucleus since it gets translated into protein as soon as it reaches the cytoplasm.
Further, unlike DNA-based therapeutics, mRNAs do not go and integrate with the host’s genome (entire genetic material).
This eliminates the risk of new mutations.
Therefore, mRNA-based therapeutics are good options for cancer vaccines, tumor immunotherapy, and infectious disease prevention.
To trigger an immune response, many vaccines put a weakened or inactivated germ into our bodies.
For mRNA-based vaccines, laboratories create an mRNA that can teach a cell how to make a protein or a part of the protein.
This triggers an immune response, producing antibodies.
When we are exposed to that protein again, the same antibodies protect us from getting sick.
Unlike DNA-based drugs, mRNA transcripts have a relatively high transfection efficiency and low toxicity because they do not need to enter the nucleus to be functional.
The average lifespan of humans has gone from 36 to around 80 years. Today the world’s oldest living human is nearly 120 years old (Lucille Randon was born in February 1904 in France).
The world record for the oldest human being ever is currently held by Jeanne Calment, another Frenchwoman, at 122 years old (born. in 1875 and died. in 1997).
Several factors influence the average duration of human life, including the usual suspects: genetics, environment, and lifestyle.
By the turn of the 20th century, economic and environmental changes were in full swing.
The 1900s brought improved food availability, better access to clean water, and better living conditions.
Scientific understanding of infectious diseases has taken huge leaps, and this, in turn, positively impacted healthcare.
Better healthcare meant lower risk for infant mortality, improved chances of surviving childhood, and better awareness of how to avoid communicable diseases.
Needless to say, longevity and the study of human lifespan and whether or not it is controlled by systemic factors became a study of interest to scientists.
Long-living individuals like nonagenarians, centenarians, semi-supercentenarians, and supercentenarians were studied and interviewed to find a possible connecting pattern.
While the results showed that there were no remarkable similarities in education, income or profession amongst the subjects, they did share significant similarities in lifestyle habits.
For example, many of them were non-smokers, were not obese, and had better mechanisms for coping with stress.
Interestingly, most of them were women.
Due to their healthy habits, older adults were less prone to high blood pressure, heart disease, cancer, and diabetes compared to their peers.
The positive health effects of these older adults extended to their first-degree relatives (siblings and children).
Children and siblings of long-living adults are more likely to live long lives themselves, showing that there is a genetic link in this mechanism.
People whose parents are centenarian are less likely to have an age-related diseases that is common among adults who are more than 70 years of age.
Longevity, like other bodily phenomenons, tends to run in families and this led scientists to examine which genes were likely responsible for this effect.
Although still a developing science, around 25% of the variation in human life span is found to be determined by genetics.
The genes that are associated with longevity are APOE, FOXO3, and CETP.
Variations in these genes are found in all the subjects with extraordinary longevity.
Scientists have conducted whole genome sequencing in supercentenarians to try and identify these gene variations.
Results of these studies show an increased disease risk in individuals with an average life span.
Despite these results scientist hypothesise that the first 70-80 years in the lives of supercentenarians are more likely due to healthy lifestyle habits than genetics.
Nutritious and wholesome diets, low alcohol intake, not smoking, and staying physically active seem to have a higher weightage when it comes to longevity.
A healthy lifestyle is shown to have reduced the risk of such individuals for typical age related ailments like heart disease and high blood pressure.
In fact many nonagenarians and centenarians live a high quality life with no age-related disease until the fag end of their lives.
The genes that have been shown to have the maximum impact on longevity are related to maintenance and optimal functioning of the cells.
Critical cell functions like maintenance of telomeres, DNA repair, and protection from free radicals have a high impact on longevity.
Further genes that are implicated in risk of heart disease, the main cause of mortality in older people, also influence longevity.
These genes are involved in vital organ systems like the cardiovascular and immune system and processes like inflammation and maintenance of blood lipid levels.
These genes are also implicated in the risk of stroke and insulin resistance.
Regions like Okinawa (Japan), Ikaria (Greece), and Sardinia (Italy) are places where many people live to see their nineties or older.
Naturally, these are places of interest to scientists studying longevity.
Common themes in these countries are that still follow a very traditional way of life without major influences from the Western world.
Further studies are needed to understand the genetic and environmental factors influencing these populations.
Several factors influence the average duration of human life, including genetics, environment, and lifestyle. Commonly implicated genes associated with longevity are APOE, FOXO3, and CETP. Nutrition, low alcohol intake, not smoking, and staying physically active seem to have a higher weightage when it comes to longevity. Further studies are needed to understand the genetic and environmental factors influencing these populations.
Addison's disease is an adrenal insufficiency disorder in which the adrenal glands do not make a sufficient amount of a few hormones, including cortisol.
This disorder can occur in people of all ages and genders.
Since levels of essential hormones like cortisol are lower, Addison's disease can be life-threatening.
Addison's disease is considered an autoimmune disorder as it occurs due to the improper functioning of the immune system that results in attacking the adrenal glands.
This affects the hormone production by the adrenals.
A few common symptoms of Addison's disease are:
Other symptoms of this disorder include:
Some people with Addison's disease may have darkened skin that is more visible on scars and folds of the skin.
Since Addison's disease develops slowly over a long period, minor changes and symptoms are often overlooked.
If you feel any of the symptoms of Addison's disease mentioned above, visit your doctor for an evaluation and prompt treatment to avoid an adrenal crisis.
Image: Is Addison’s Disease Genetic? Common Symptoms
Addison's disease occurs when immune system cells attack and damage the outer part of the adrenal gland (called the cortex).
When over 90% of the adrenal cortex is damaged, the gland cannot produce sufficient hormones, resulting in Addison's disease.
It is still unclear why people develop this autoimmune disorder, but researchers speculate this disease may run in families.
Other causes of Addison's disease are:
Besides familial history, researchers also indicate that a few genes may increase an individual's risk for Addison's disease.
Studies show that the most common genes associated with Addison's disease belong to the human leukocyte antigen or HLA complex.
The HLA complex genes help the body's immune system differentiate between the body's proteins from those made by viruses and bacteria.
The most well-known risk factor for Addison's disease is a variant of the HLA-DRB1 gene, also called the HLA-DRB1 *04:04.
This variation of the HLA-DRB1 gene results in an abnormal immune response, damaging the adrenal cortex and causing Addison's disease.
The exact mechanism of how this gene damages the adrenal cortex is still unknown.
Based on symptoms, if the doctor suspects Addison's disease, they may take a detailed medical and familial history.
They may also screen for skin discoloration in areas such as:
The doctor will also check your blood pressure for hypotension, especially when you change position.
Diagnostic tests for Addison's disease include:
Medications are common treatment options for Addison's disease.
The most common and effective treatment for Addison's disease is hormone replacement therapy.
This treatment corrects or restores the steroid hormone the body is not producing adequately.
Other tips for managing Addison's disease include:
Did you know the lifetime risk for developing alopecia areata is >2%, even with no family history? Alopecia areata is an autoimmune disorder characterized by hair loss on the scalp or other body parts. In people with alopecia areata, the immune system attacks the hair follicles, causing them to shrink and preventing new hair from growing. Studies have shown that people with certain HLA genes are more likely to develop alopecia areata. This suggests that there may be a genetic predisposition for the condition.
Alopecia areata is a health condition that results in massive amounts of hair fall.
Most people with alopecia witness hair fall in small and round patches resulting in a coin-like appearance of bare skin.
While alopecia mostly affects the scalp, it can result in hair fall in other body parts like eyebrows.
It affects as many as 6.8 million people in the United States and 147 million worldwide.
Alopecia is the second most common hair loss condition after androgenetic alopecia and affects men and women equally.
Alopecia isn’t a painful or disabling condition; however, it can change a person's physical appearance, affecting their quality of life and self-esteem.
Most of the research shows that people with alopecia have higher levels of anxiety and depression.
There are two types of alopecia areata:
Research also reports a few rarer forms of alopecia, each with unique hair loss patterns.
The role of our immune system is to fight off unwanted invaders that enter our body, like viruses and harmful bacteria.
In some people, the immune system goes into overdrive and starts attacking the healthy cells in the body, resulting in a group of conditions called autoimmune disorders.
Alopecia, one such autoimmune condition, occurs when the immune system starts attacking the hair follicles.
However, it doesn't destroy the hair follicles, so hair regrowth is a possibility.
The reason why the immune system goes into overdrive is complex and not well understood.
It could be a combination of many factors like hormonal imbalances and genetic changes.
Evidence also supports that environmental factors like stress, physical injury, and illness can result in abnormal immune reactions.
The immune system involvement in alopecia suggests the role of HLA genes in alopecia.
HLA genes to a gene family called the human leukocyte antigen (HLA) complex.
The HLA complex plays a key role in guiding the immune system by helping it differentiate between the body's own proteins and proteins made by foreign invaders.
There are many types of HLA genes, each of which allows the immune system to react to different types of invaders.
Certain changes in these HLA genes can make the immune system confused and result in misidentifying the body's own cells as foreign.
In alopecia, specific HLA gene changes make the hair follicles appear foreign to our immune system.
Other genes involved in inflammatory processes also appear to play a role in alopecia.
Alopecia shares similar genetic roots to other autoimmune conditions.
Therefore, people with alopecia may be at increased risk for conditions like:
People with any of these conditions have an increased risk for alopecia as well.
Several genetic, environmental, and lifestyle factors contribute to alopecia.
As a result, the inheritance pattern is unclear.
However, it is evident that the risk for alopecia is heightened in siblings and children of affected individuals than in the general population.
A family history of other autoimmune conditions also increases the risk of alopecia.
The risk for alopecia increases with:
The primary step in diagnosing alopecia areata is a physical exam to see the pattern of hair loss.
Blood tests can also reveal autoimmune disorders.
The doctor may also perform additional tests to reveal any underlying disorder.
The type of test your doctor may order depends on what they may suspect is causing the problem, which may be based on other symptoms.
Some common medications used to treat children 10 years or younger are corticosteroids and minoxidil.
They are also used in adults with patchy alopecia areata
Complete loss of hair is treated with contact immunotherapy, where the goal is to change your immune system so that it stops attacking your hair follicles.
Is insomnia genetic? According to the Sleep Foundation, the heritability of insomnia is 31-58%, indicating a strong genetic component to insomnia.
In the sample report below, we've attempted to analyze some important genes that increase the risk for insomnia.
You can identify your genetic risk of insomnia by using your 23andMe DNA data and placing an order for the Gene Sleep Report.
Insomnia (also known as sleeplessness) is a common sleep disorder that is characterized by the inability to fall asleep or stay asleep at night, resulting in tired or unrefreshing sleep.
According to the American Psychiatric Association (APA), insomnia is the most common sleeping disorder.
Approximately 30% to 40% of adults in the United States report symptoms of insomnia.
A diagnosis of insomnia needs to meet the following two categories:
This can be caused by variations in biological, psychological, and social factors, which most often result in a reduced amount of sleep.
People with parents or siblings with insomnia have an increased risk of experiencing the condition themselves. This indicates a genetic link to insomnia.
This was further confirmed by a 2018 study that reported that insomnia has a partially heritable basis. In fact, heritability accounts for 31% to 58% of your insomnia risk.
Insomnia also appears to share genetic links with other health conditions.
The researchers also found a strong genetic link between insomnia and type 2 diabetes.
Tissue-specific gene-set analyses showed that insomnia might have higher genetic signals among genes that are usually expressed in the brain.
The functions of these regions of the brain are of relevance to insomnia.
The genetic correlations between insomnia and psychiatric traits were stronger than the genetic correlations between insomnia and other sleep-based characteristics.
The study suggests that, genetically, insomnia resembles neuropsychiatric traits more closely than other sleep-related characteristics.
The MEIS1 gene is a transcription factor that plays a key role in hematopoiesis, endothelial cell development, and vascular patterning.
It also plays a role in neurodevelopment.
Research studies have shown that the reduced MEIS1 levels and function of the gene may contribute to the pathogenesis of sleep-related disorders.
The rs113851554 is a G>T polymorphism located in the MEIS1 gene, which is found to be correlated with multiple sleep disorders.
A study found that the T allele of rs113851554 is associated with an increased risk of developing insomnia symptoms.
Functional study analysis suggested that the rs113851554 in the MEIS1 locus is most strongly associated with insomnia disorder.
A July 2022 study published in Nature Genetics attempted to discover new genetic loci (specific regions in the gene) associated with insomnia.
This was a robust study since it included nearly 600,000 cases and 1.8 million controls.
The study identified 554 risk loci, out of which 364 loci were novel, associated with insomnia.
It also prioritized 289 genes that could help understand the underlying mechanisms of insomnia.
Insomnia is more common in women than in men.
More than one in four women in the United States experience insomnia, compared with fewer than one in five men.
Insomnia is more common in older people than in younger ones.
As many as 50% of older adults complain about difficulty initiating or maintaining sleep.
Medical and psychiatric conditions can increase insomnia risk.
Insomnia is more commonly seen in those with heart disease, asthma, depression, and anxiety than their healthier counterparts.
https://pubmed.ncbi.nlm.nih.gov/30804565/
https://pubmed.ncbi.nlm.nih.gov/26132482/