Persistent fatigue, abdominal discomfort, or unexplained changes in appetite are just some symptoms that can signal underlying liver health issues.
When it comes to liver diseases, understanding the genetic factors involved is crucial.
In this blog post, we shed light on the top three genetic liver diseases of 2023, unraveling the connections between genetics and common symptoms that impact daily life. Read on to learn more!
Certain genes don’t directly cause diseases but contribute to increased risk. Triggered by certain environmental or lifestyle events, this risk can translate into disease development. Learning about these genes can help modify lifestyle factors to reduce your risk or even prevent the conditions. Learn more:
Genetic liver diseases are a group of genetic and metabolic defects that can result in chronic liver disease.
While some people inherit these conditions from their parents or close relatives, others are born with abnormal changes (or mutations) in their genes.
The prevalence of genetic liver diseases is variable, and they are considered rare diseases.
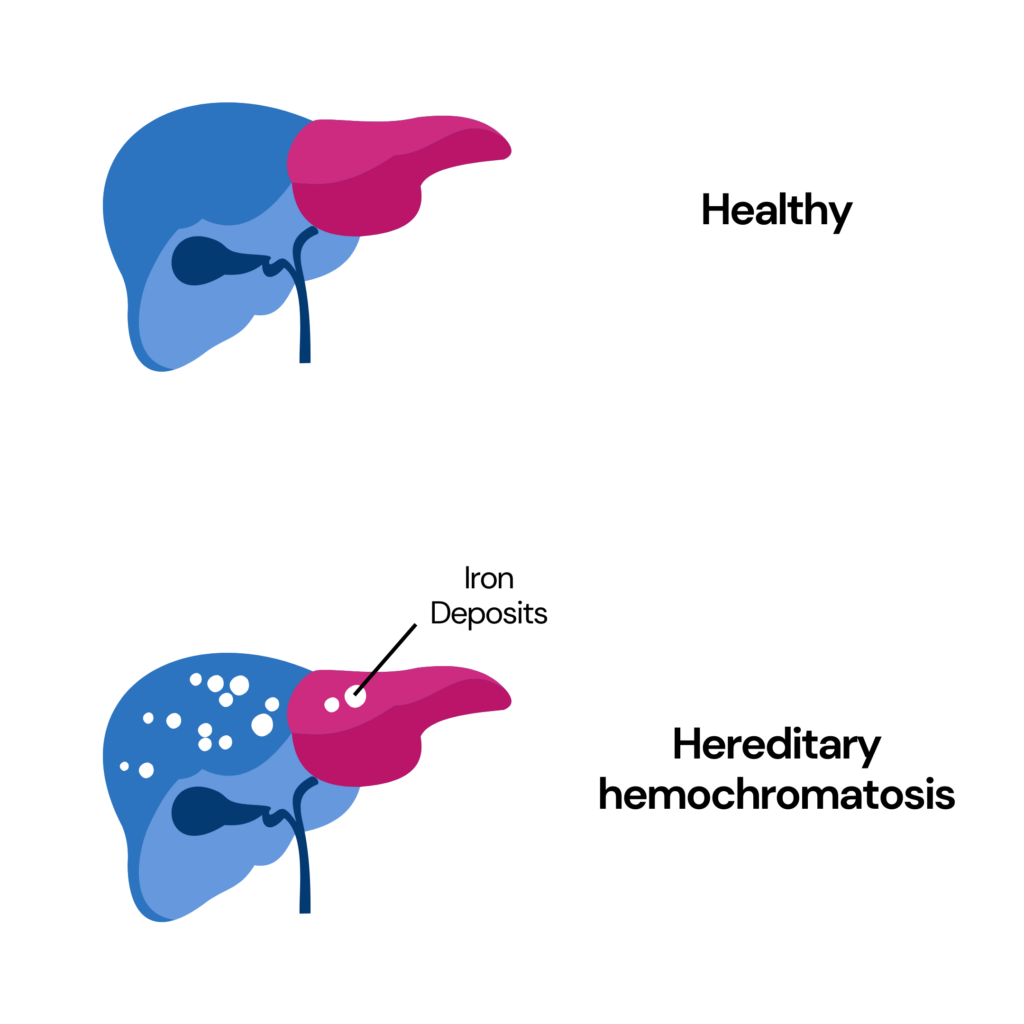
Hemochromatosis is a genetic liver disease in which iron begins to collect in the liver and other organs.
Primary hemochromatosis is one of the most common inherited diseases in the US.
When one family member has this disorder, their siblings, parents, and children may be at risk.
Secondary hemochromatosis is not genetic and is caused by other diseases like thalassemia.
Iron overload associated with hemochromatosis affects men more commonly than women.
Due to menstruation, women are not likely to show signs of iron overload until menopause.
Symptoms and Treatment
A few common symptoms of hemochromatosis include:
People with hemochromatosis may also show signs of diabetes and heart disease.
Treatment for hemochromatosis includes one of the following:
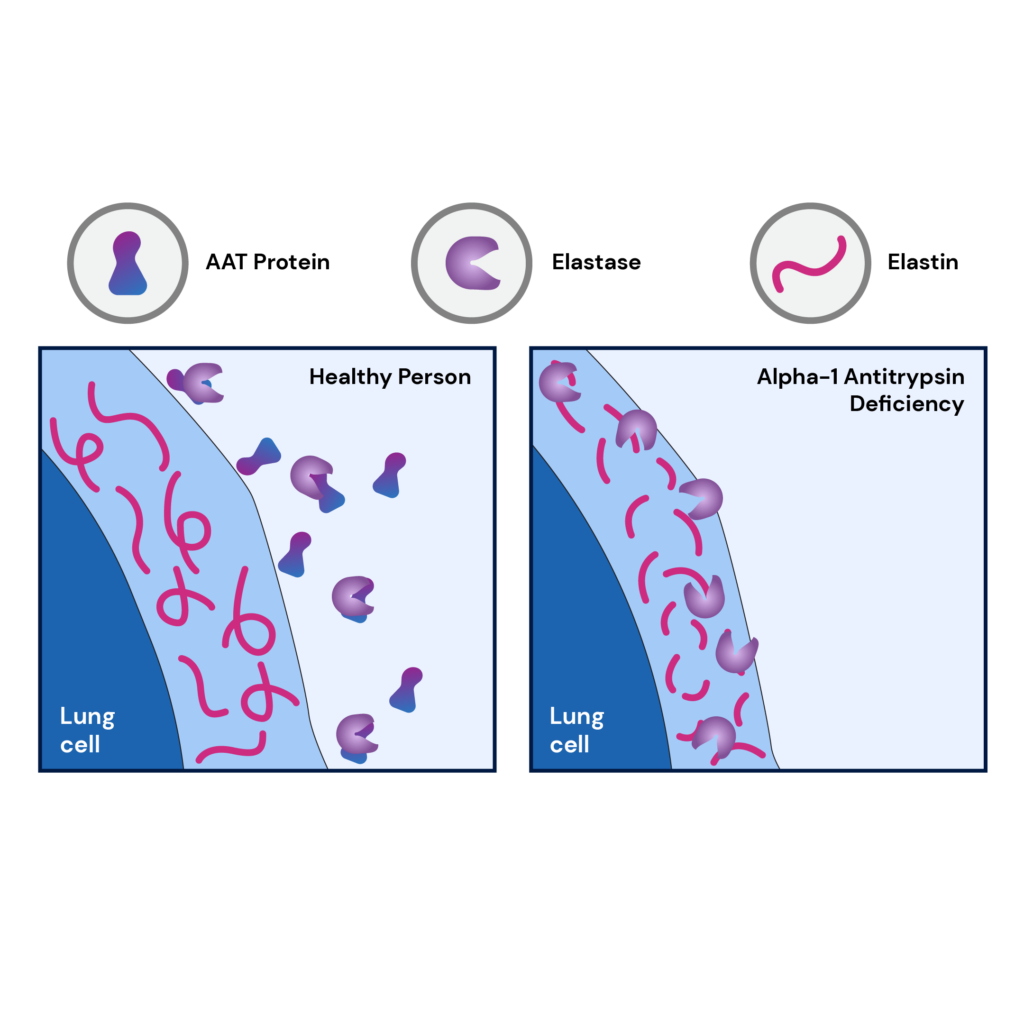
Alpha 1 antitrypsin deficiency, or AATD, is an inherited genetic condition that affects 1 in 1,500 to 3,500 individuals of European ancestry.
This condition affects the lungs and liver.
Alpha-1 antitrypsin is a protein that protects the lungs from damage due to infection-fighting components released by the immune system.
When this protein is too low or damaged, the lungs are affected, leading to breathing difficulty and conditions like emphysema.
People with this condition also risk developing cirrhosis due to the accumulation of alpha-1 antitrypsin.
In the lungs, AATD causes emphysema, whereas, in the liver, it causes the accumulation of abnormal alpha-1 antitrypsin, leading to progressive liver injury.
Symptoms and Treatment
One of the first symptoms of AATD is usually those which affect the lungs.
Common symptoms of AATD include:
Currently, there is no established treatment to cure AATD.
While replacing the defective protein in the bloodstream may be done, experts need clarification about how effective this procedure will be.
Most often, treatment of AATD includes the management of emphysema and cirrhosis.
Other treatments may include:
People with AATD can undergo a liver transplant if they don’t have lung disease.
Wilson's disease is a genetic disease caused by mutations in the ATP7B gene and results in an increased accumulation of copper in the body.
This is a rare disease and affects 1 in 30,000 individuals.
Wilson's disease does not cause any symptoms unless it is serious.
It can be diagnosed using blood and urine tests, liver biopsies, and genetic tests.
The aim of treating Wilson's disease is to remove the excess copper in the body and prevent reaccumulation.
Symptoms and Treatment
Common signs and symptoms of Wilson’s disease are:
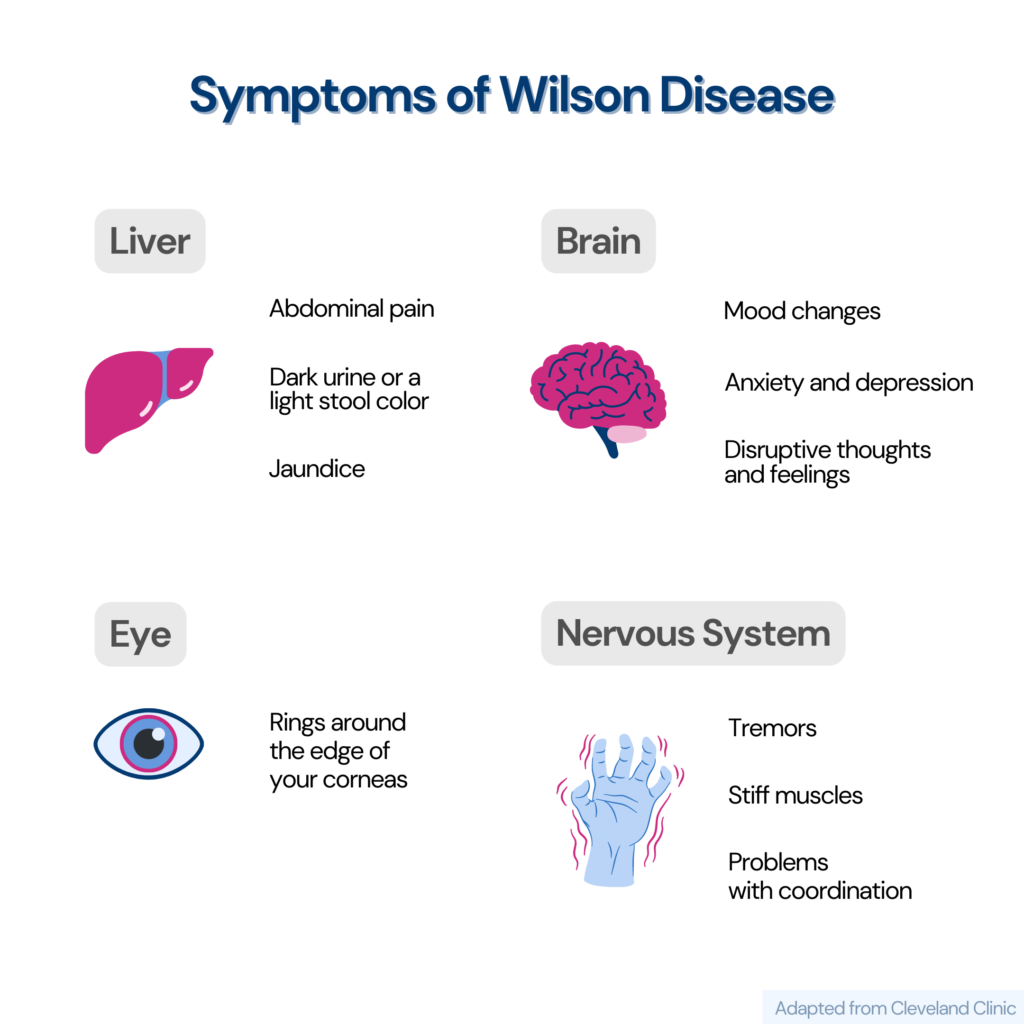
The treatment of Wilson’s disease includes one or more of the following:
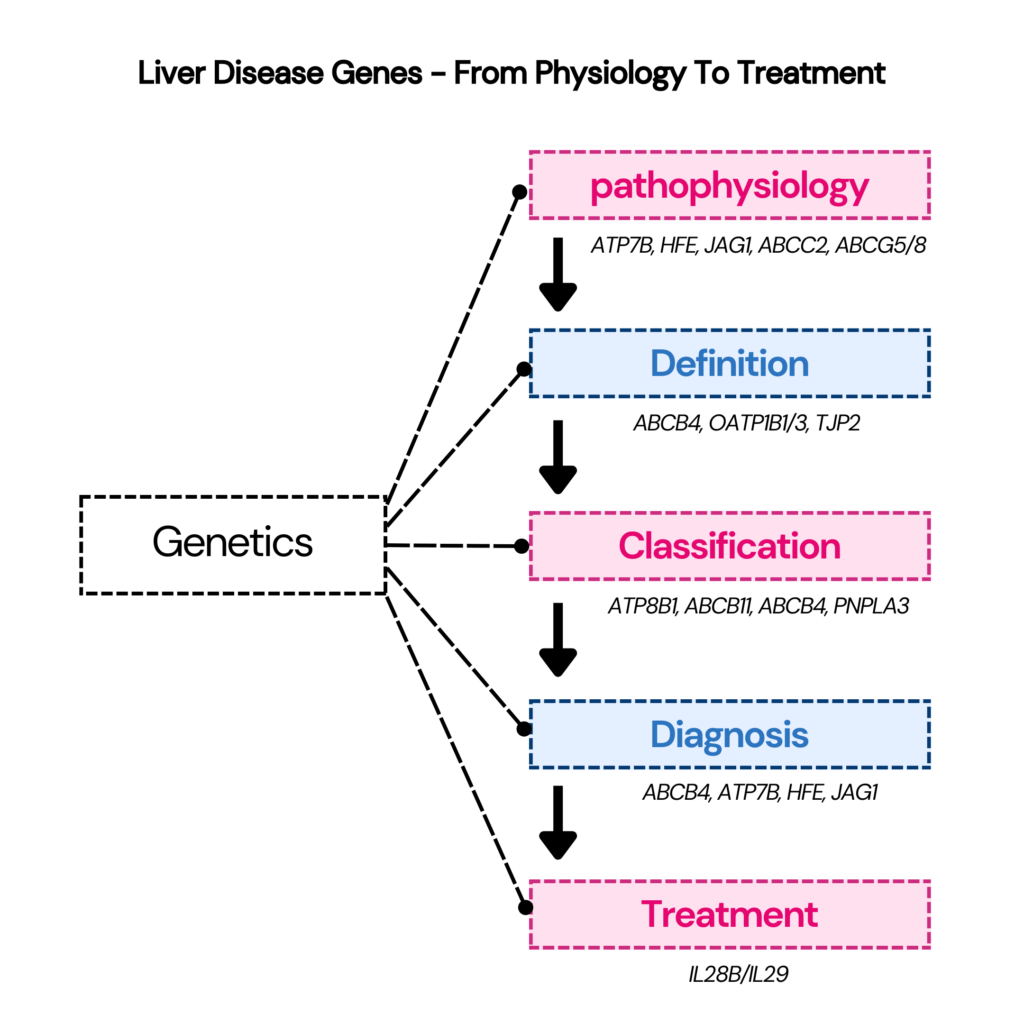
Genetic testing is recommended for individuals with liver diseases like bile acid synthesis defects, jaundice, and cholestasis with unknown causes.
A liver genetic test usually involves sequencing or deletion/duplication analysis.
Before a genetic test for liver disease is performed, your doctor may recommend the following tests:
To undergo genetic testing for liver disease,
In some cases, a blood test may be followed by a liver biopsy to interpret the test results better.
A few genes that are routinely tested for genetic liver disease are:
Some direct-to-consumer genetic testing companies provide the option to learn your risk for liver diseases.
These tests are non-invasive and don’t diagnose genetic liver diseases. However, they present you with a comprehensive risk profile for liver diseases.
This information can then be used to reduce your risk and enable early screening and detection.
Liver Disease Parameters in Xcode Life’s Health Panel
Check Out The Gene Health Panel Here
There are several tests available for diagnosing genetic liver diseases. However, these tests have their limitations.
Genetic testing is most useful for diseases like hereditary hemochromatosis due to the high frequency of C282Y mutations in people of European descent.
In the case of other genetic liver diseases, testing is less helpful as they have a higher number of possible mutations and clinical manifestations.
Appropriate use of screening tests can help in the early detection of genetic liver diseases and prevent end-organ damage.
However, genetic testing for liver diseases cannot prevent the development of the disease.
Unlock the secrets to a better night's sleep by understanding the fascinating interplay between your menstrual cycle and sleep.
As a woman (or people assigned females at birth), your monthly cycle influences more than just your physical and emotional well-being.
It can significantly impact the quality of your sleep.
Each phase of your menstrual cycle brings unique changes to your body that can affect your sleep patterns.
This article delves into the intricate relationship between your menstrual cycle and sleep, exploring how different phases can disrupt or enhance your rest.
We also provide practical tips to optimize your sleep throughout your cycle.
Did You Know? While external factors impact your sleep health, internal factors like your genes can also influence how well you sleep. Certain genetic differences can result in poor sleep quality and an increased risk for sleep disorders. Learn more:
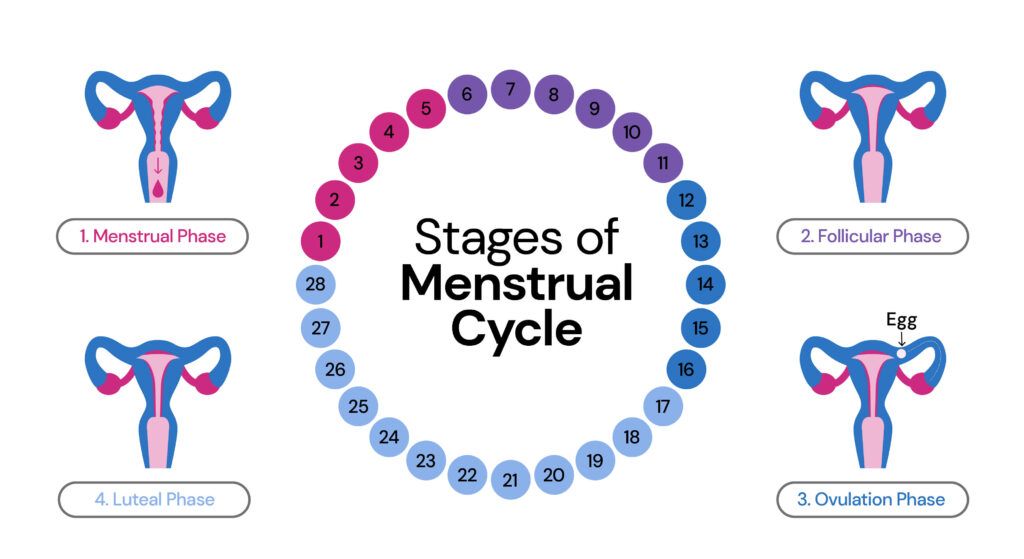
There are four stages in the menstrual cycle:
| Phase | Description | Days* | Hormone changes |
| Menstrual phase | Menstruation, the initial phase of the menstrual cycle, involves the shedding of the uterine lining. This 3 to 7-day process occurs when the egg is unfertilized, eliminating the mucous layer through the vagina, though the duration may differ among individuals. | Day 1 - Day 5 | Estrogen and progesterone level drops |
| Follicular phase | Follicles develop on the surface of the ovary, with one mature to form an egg. 6th day after menstruation until ovulation. Women with regular cycles have this phase for around 6-8 days. | Day 6 - Day 11 | Estrogen levels rise, and low progesterone levels |
| Ovulation phase | Release of an egg/ovum from one of the ovaries. Women with normal cycles have this phase for around 5-7 days. | Day 12 - Day 16 | Estrogen levels start to decrease, and progesterone levels start to increase |
| Luteal phase | The luteal phase lasts around 8-11 days in regular cycles. Hormonal changes during this phase may lead to mood swings, headaches, acne, bloating, and breast tenderness - common signs of premenstrual syndrome (PMS). If fertilization doesn't occur, the menstrual cycle repeats from the beginning. | Day 17 - Day 28 | Higher progesterone (declines as the luteal phase approaches an end) and lower estrogen levels |
Women experience sleep disturbances more frequently than men.
One of the factors contributing to this could be the menstrual cycle.
According to a study, young women who reported sleeping less than 8 and 7 hours per day experienced more premenstrual spasms than those who slept for 8 hours or more.
Sleep disturbances tend to increase during the premenstrual and menstruation phases, particularly in women with PMS and dysmenorrhea (painful menstrual cramps).
This could be attributed to hormonal changes involving progesterone and estrogen.
The effects of the changes are more notable in the premenstrual phase.
Women diagnosed with polycystic ovary syndrome might encounter sleep problems due to the following factors:
Is Obstructive Sleep Apnea Genetic?
Compared to the follicular phase, the luteal phase results in a body temperature rise of about 0.3°C to 0.7°C.
This sudden temperature change creates disturbed sleep quality.
A study also associates higher body temperature with reduced REM sleep in the luteal phase.
Therefore, hormonal fluctuations throughout the menstrual cycle alter temperature regulation, affecting sleep quality.
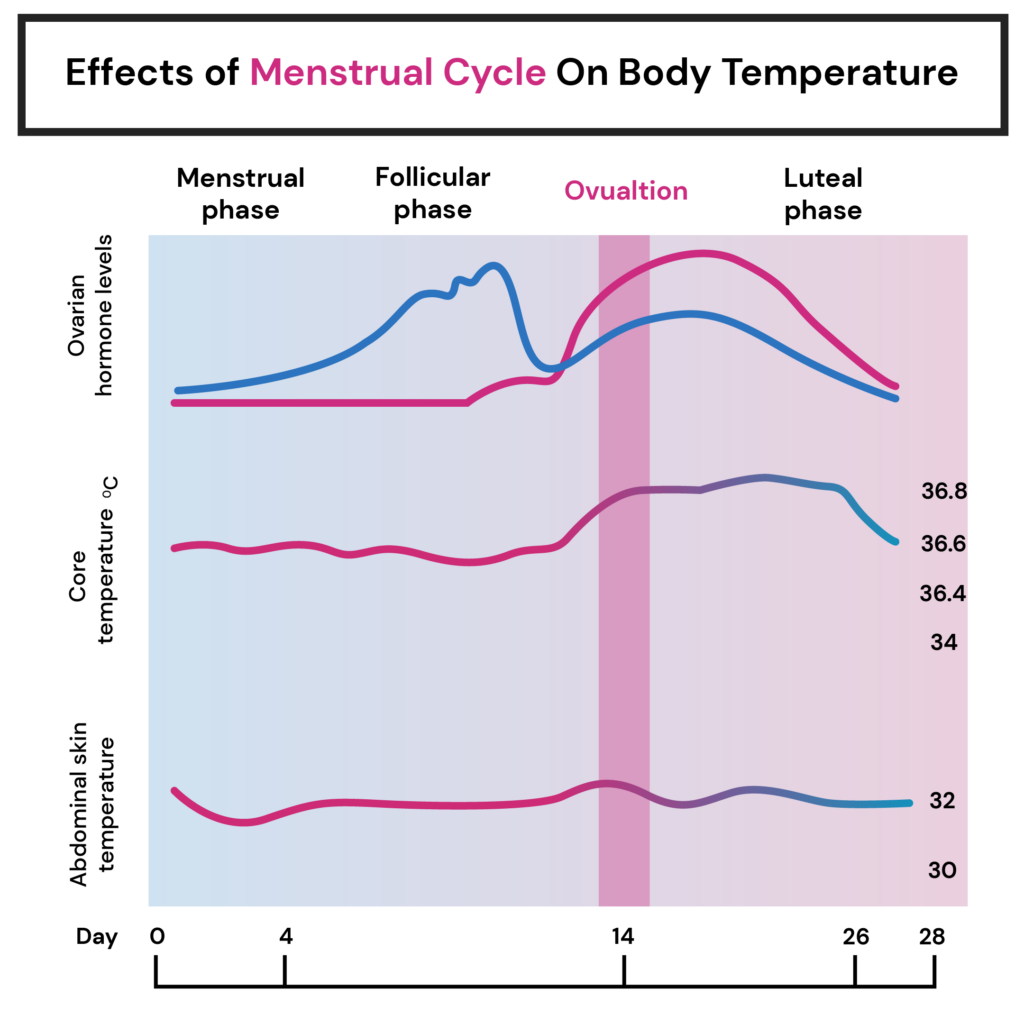
Higher progesterone (declines as the luteal phase approaches an end) and lower estrogen levels during the luteal phase prevail if the egg is not fertilized.
A 2016 study published in the Journal of Sleep Medicine and Disorders investigated the relationship between sleep and PMS.
It reported the following:
Females who experience premenstrual syndrome are more likely to have insomnia.
As a result, they experience excessive daytime sleepiness, reduced focus, and concentration, and are tired and drowsy throughout the day.

Women experience more sleep problems than men, with one of the key factors being hormonal fluctuations during their menstrual cycle.
Hormonal fluctuations alter the temperature range, which also impacts sleep quality.
Sleep problems are more evident in the luteal (premenstrual) and menstrual phases than in others due to reduced melatonin and allopregnanolone levels and menstrual cramps.
Sleep quality can be improved by incorporating natural remedies, practicing relaxation techniques, implementing pain management strategies, reducing caffeine consumption, and avoiding exposure to blue light.
Please consult a qualified healthcare practitioner if you experience severe sleep disturbances or other menstrual cycle-related problems.
Here's how you can still get your sleep report
Diabetes affects millions worldwide, and managing this chronic condition can often feel like a never-ending puzzle.
However, in our increasingly digital age, new tools and technologies are emerging to transform how we approach diabetes care.
At the forefront of this revolution is artificial intelligence (AI), a game-changing force that promises to enhance daily life for individuals with diabetes.
In this blog post, we'll unravel the potential of AI, examining its role in improving glucose control, providing personalized insights, and even predicting future health outcomes.
Did you know? Your genes hold precious clues about nearly all aspects related to your health and wellness. Harnessing this information can help prevent diseases, improve diet, age gracefully, and maintain a healthy weight. Learn how:
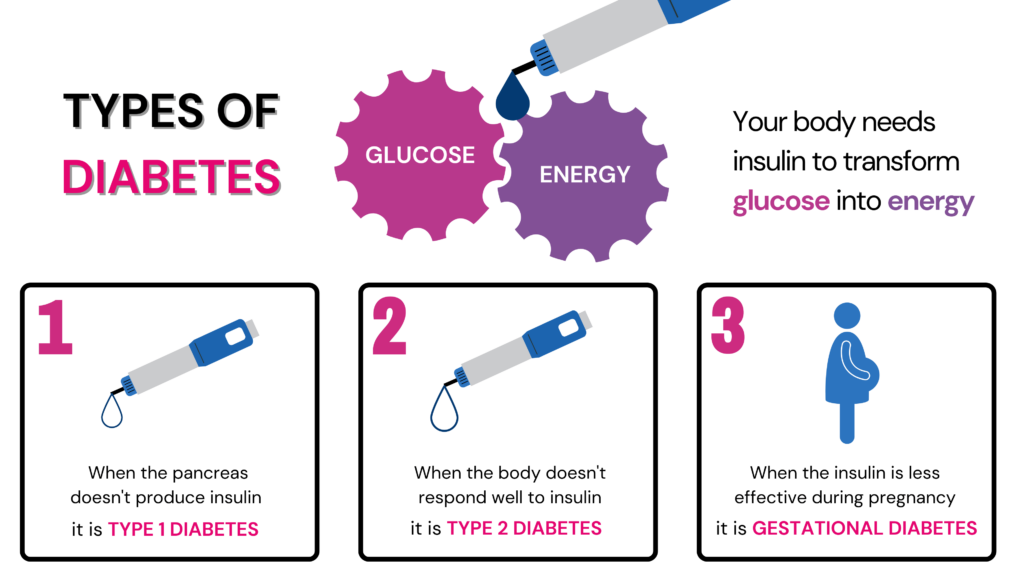
Diabetes is a chronic condition that affects millions of people globally.
It occurs when the body struggles to regulate blood sugar levels, which are critical for our cells' energy production.
The pancreas plays a vital role in this process by producing insulin, a hormone that enables the body to manage glucose levels effectively.
However, insulin production complications can lead to abnormal sugar levels and result in diabetes.
Diabetes is classified into numerous categories. The most widespread are type 1, type 2, and gestational diabetes.
Is Type 2 Diabetes Genetic?
Blood sugar monitoring, dietary adjustments, and, in some cases, insulin therapy are essential in managing gestational diabetes to ensure a healthy pregnancy and delivery.
Living with diabetes presents numerous challenges that require continuous management and care. Some of them are:
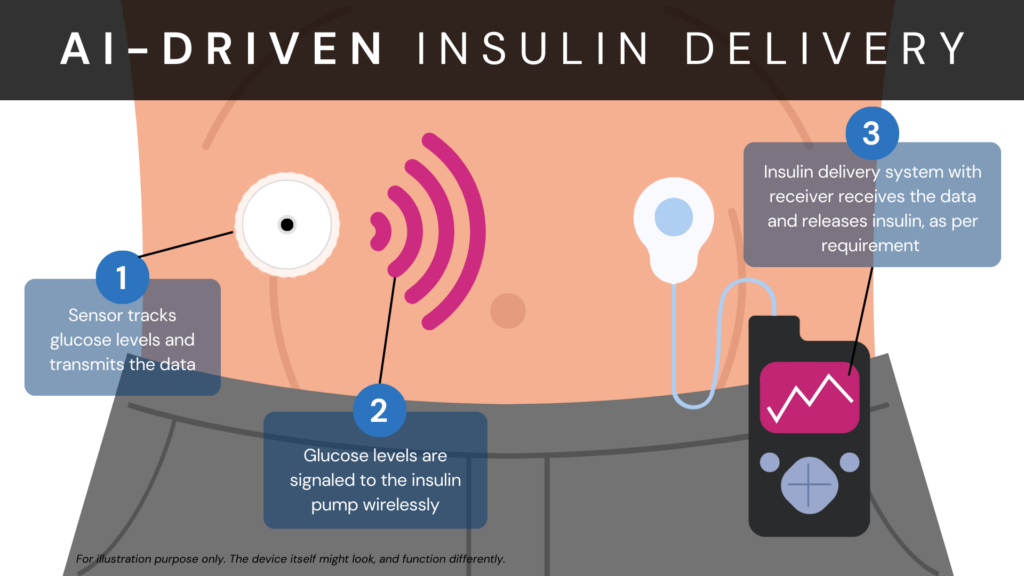
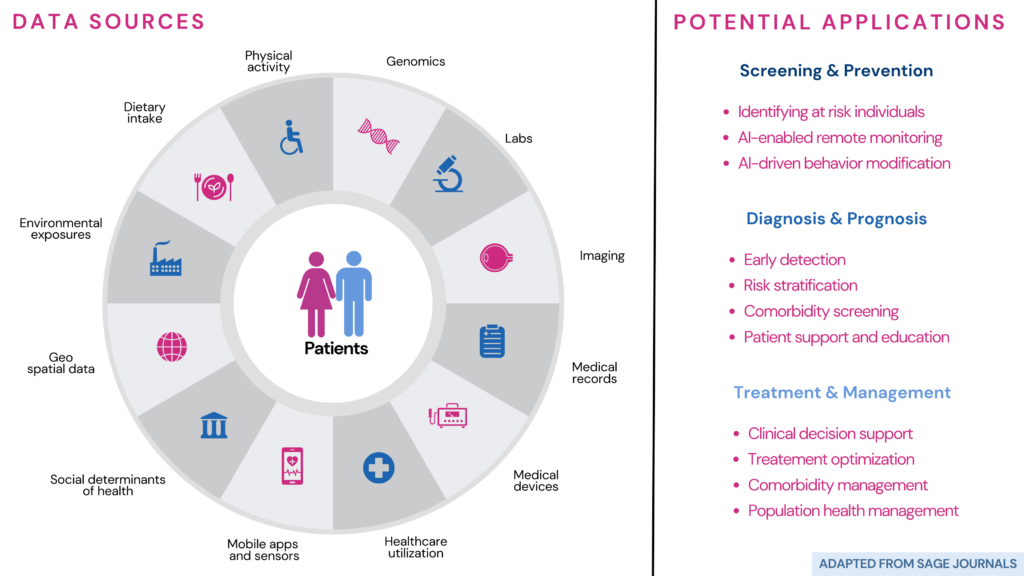
The ever-evolving progress of AI has revolutionized how diabetes is treated and monitored, introducing numerous possibilities for enhanced care.
Traditional glucose monitoring typically involves periodic finger pricks to measure blood sugar levels.
By using AI technology, monitoring glucose levels has undergone a remarkable transformation.
Continuous glucose monitoring (CGM) devices use tiny skin-implanted sensors to test glucose levels faster than slower traditional methods.
Lots of data are gathered and then examined using machine learning techniques.
The algorithms can detect abnormal events, trends, or patterns in glucose data from this process.
Benefits of AI-driven glucose monitoring
AI can continuously analyze glucose levels and consider factors like carbohydrate intake and activity levels.
It can then use this information to deliver precise and timely insulin doses without requiring manual calculations or frequent user intervention.

The advantages of AI-powered smart insulin pumps include the following:
It is important to note that AI technologies in diabetes management are meant to support and complement the expertise of healthcare professionals.
While these technologies offer valuable insights and automation, they should always be used under medical supervision and with personalized care plans.
Machine learning techniques have been used in medical health research, including predicting diabetes.
In a study, researchers used AI and machine learning (ML) technologies to predict diabetes in a dataset from a hospital in Luzhou, China.
The three tools used here include:
All these employ AI and ML but use slightly different techniques.
The scientists divided the data into training sets and a test set to test their methods.
They used the training sets to teach the computer program how to make predictions. Then they used the test set to see how accurate the predictions were.
While they used various methods to assess and simplify the data, they found that using all the information about a person's health was the best way to predict diabetes.
Further, while all the 3 tools predicted diabetes accurately, random forest was the best predictor.
This study shows that machine learning can help predict diabetes.
By using these computer programs, doctors can understand who might develop diabetes in the future and take steps to prevent it or manage it better.
Mobile apps are a simple and convenient way to manage diabetes.
Features like glucose level tracking, meal planning, medication reminder, and other insights can prove useful for those with diabetes.
These are some commonly used apps:
Note: The apps in this list are not our recommendations, and we do not vouch for any of them. This is for informational purposes only. The best app for you will depend on your needs.
The following features provided by most diabetes care apps make them useful tools for managing this condition:
Can AI help with a breast cancer diagnosis?
Using AI in diabetes care can help prevent the condition in the following ways:
By harnessing the power of AI, healthcare providers can enhance preventive efforts, enable early detection, and provide personalized care for individuals at risk of developing diabetes.
Discussing the ethical issues in AI implementation is important as it continues influencing diabetic care. Developing AI ethically and preserving human control also involves safeguarding data privacy and preventing algorithmic biases.
However, the future possibilities of AI in diabetes management are promising, offering advancements that can revolutionize daily life for individuals with diabetes.
Let's briefly discuss these considerations and their potential effects in the future:
Future Directions
Integrating AI into the lives of those with diabetes has immense potential for transformative change.
The benefits of AI are enormous, from managing diabetes more effectively to improving quality of life and overall health outcomes.
AI-based glucose monitoring technologies, such as CGM systems, offer the following benefits:
Smart insulin pumps powered by AI algorithms provide automated insulin delivery, improving glycemic control and more comfort.
Moreover, AI can predict the risk of developing diabetes by analyzing vast datasets and generating personalized risk assessments.
Diabetes care apps integrated with AI provide on-the-go monitoring, customized support, seamless data integration, reminders, notifications, and community support.
Ethical considerations, such as data privacy, algorithm bias, and human oversight, are crucial when implementing AI in diabetes care.
The advancements in AI for diabetes management have promising future implications.
These include continuous glucose monitoring, closed-loop systems, incorporation with wearable devices, and adopting a comprehensive approach to care.
https://www.healthline.com/health/diabetes/top-iphone-android-apps
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4422872/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7530691/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7325854/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6859270/
https://www.nature.com/articles/s41591-022-02144-z
https://www.frontiersin.org/articles/10.3389/fsurg.2022.862322/full
https://pubmed.ncbi.nlm.nih.gov/28585879/
https://www.frontiersin.org/articles/10.3389/fgene.2018.00515/full
https://academic.oup.com/edrv/article/44/2/254/6692818
https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6550406/
https://my.clevelandclinic.org/health/drugs/11444-glucose-continuous-glucose-monitoring
We humans often experience pain as an unwelcome barrier. But what if there was a way to break through those barriers?
What if physical activity held the key to unlocking a higher pain tolerance? A new study reinforces that engaging in physical activities reduces chronic pain experience.
This article reveals pain tolerance, the factors affecting them, and how physical activity is associated with pain tolerance effect with a study supporting this concept.
Read on to uncover further insights.
Your genes play a strong role in influencing your pain threshold.
Pain tolerance is the capacity of a person to handle or tolerate pain.
Individuals with higher pain tolerance can feel less pain than those with moderate or low pain tolerance.
A simple example is a person's ability to touch a hot surface. A person with higher tolerance can have higher exposure than others.
Some factors influence the pain tolerance of an individual.
Genetics has emerged as a significant factor in understanding the variation in pain tolerance among individuals.
Our genetic makeup plays a crucial role in determining how we perceive and respond to pain stimuli.
Studies have shown that certain genetic variations can affect the functioning of pain receptors, neurotransmitters, and inflammatory pathways, ultimately influencing our pain perception and tolerance levels.
Research strongly suggests that males and females differ in their responses to pain.
This is due to differences in the anatomy, genetic makeup, types and levels of hormones, nerve responses, etc., between males and females.
Each of us possesses a unique lifestyle and varying levels of exposure to different experiences. For instance, people who smoke may be more sensitive to pain.
On the other hand, athletes have a higher pain tolerance.
It’s no secret that your mind and body are connected. So, anything that affects your mental health, including conditions like depression and anxiety, may increase pain sensitivity.
Engaging in physical activities/exercises is associated with higher pain tolerance.
During exercise, the body releases chemical compounds known as endorphins.
Endorphins are the body’s natural pain-relieving chemicals.
They engage with specific parts of the brain, subsequently diminishing one's perception of pain.
This decrease in pain sensation through exercise is termed exercise-induced hypoplasia.
Furthermore, repeated exposure to discomfort during exercise might lead to adaptations in the central nervous system, resulting in enhanced pain tolerance.
However, the exact mechanisms behind this connection are not yet fully understood.
Many aspects of our fitness, like injury risk, endurance potential, lung capacity, tendon strength, and pain tolerance, are influenced by our genes. Learning about how your genes impact fitness can be very helpful in achieving your fitness goals.
According to a recently published study in PLOS ONE, higher levels of physical activity have been found to decrease or prevent chronic pain sensation.
This study was conducted by nine researchers affiliated with the Department of Pain, University Hospital of North Norway, Tromsø, Norway, and some centers in Norway.
The study included 10,732 Norwegian adults, 51% of whom were females.
The participants’ mean age was 55.8 years.
The study measured two parameters: physical activity and pain tolerance.
The former was self-reported by the participants as “leisure-time physical activity,” which includes all physical activities done during the day, including exercise.
Pain tolerance was measured using a cold-pressor test (CPT) where the participants had to submerge their hands (till their wrists) in water (3°C) for as long as possible.
Certain workouts have shown promising results when it comes to improving pain tolerance through exercise. Here are some of the best exercises to consider:
Remember, it's important to listen to your body and start at an appropriate level of intensity that is best for your needs.
Consult a healthcare professional or fitness expert for any underlying health conditions or concerns.
Pain tolerance refers to a person's ability to endure or withstand pain.
Factors like age, gender, genetics, environment, and lifestyle factors might influence a person to experience pain tolerance.
A new study suggests that engaging in physical activity is associated with higher pain tolerance - the more intensity, the higher the pain tolerance.
Certain types of physical activities, like HIIT, resistance training, yoga, and tai-chi, in particular, are known to improve pain tolerance.
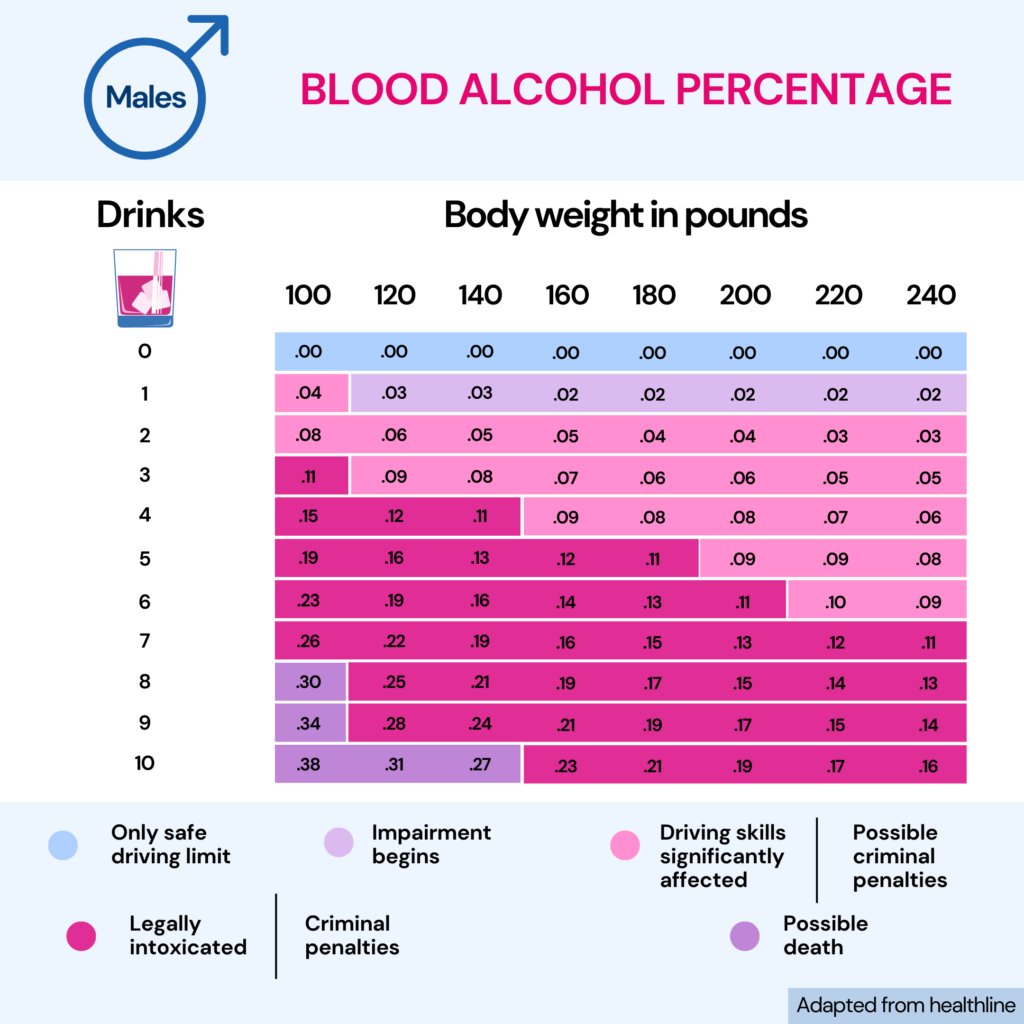
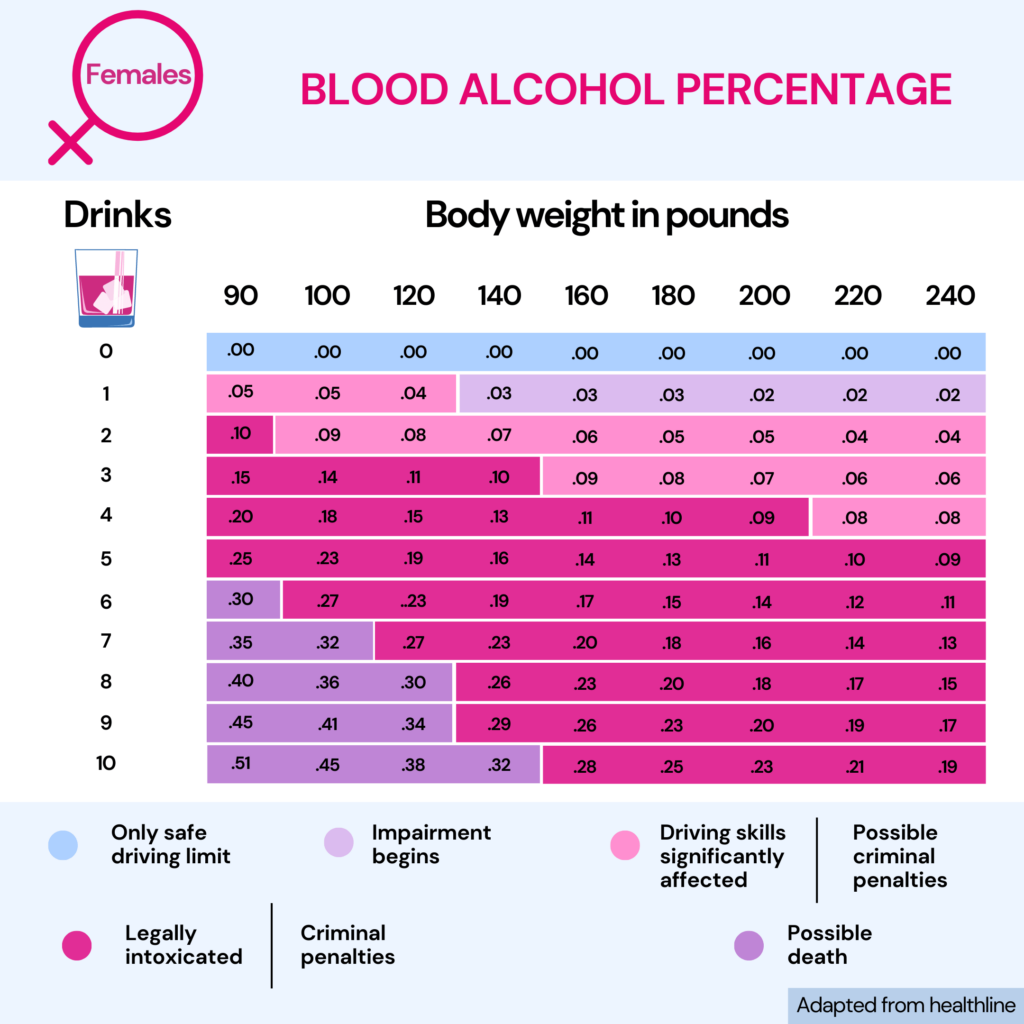
Having a drink once in a while is acceptable. However, if you drink frequently and for an extended period, you develop alcohol tolerance.
While most people may boast about their tolerance to alcohol, when unchecked, it can lead to harmful health consequences, including addiction and liver disease.
Several reasons affect your tolerance to alcohol, and no two people will have the same alcohol tolerance.
Let’s explore the various factors of alcohol tolerance and how your genes have a role to play in it!
Tolerance is your body’s ability to suppress normal responses to substances and toxins.
Alcohol tolerance refers to a situation where continuous drinking results in the same amount of alcohol having a lesser effect on the body.
An increased amount of alcohol may be required to produce the same effects.
Your alcohol tolerance depends upon how your body responds to it in different situations, how much remains in the system, and the efficiency in eliminating it.
Someone with a greater tolerance usually enjoys many drinks without feeling “drunk.”
Alcohol tolerance is one of the many prominent symptoms of alcohol dependence.
This is, in fact, a stage of alcohol addiction when you need a drink to prevent alcohol withdrawal symptoms.

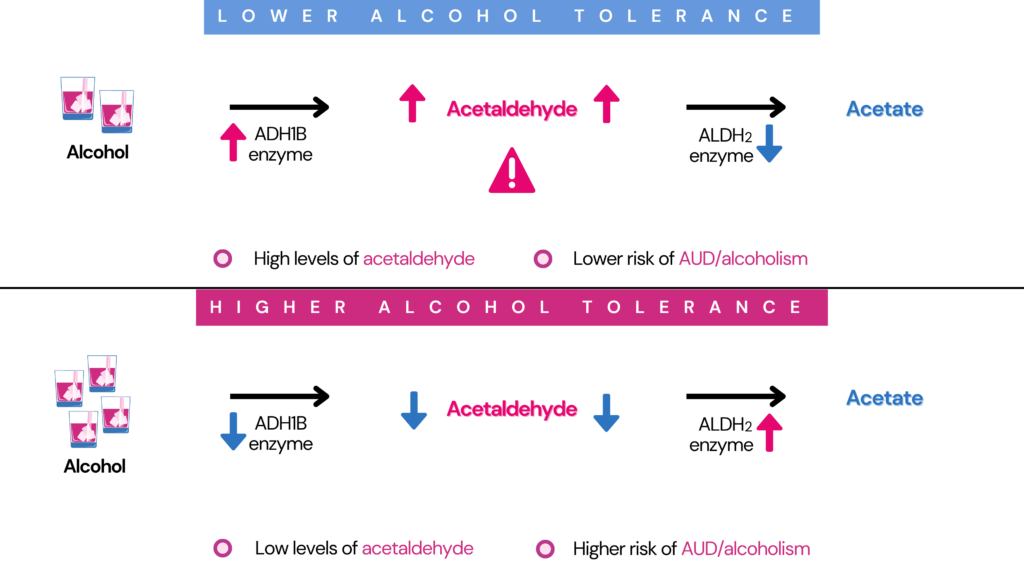
Genetics plays a significant role in alcohol tolerance.
Changes in the genes, including ADH1B and ALDH2, that participate in alcohol metabolism can influence alcohol tolerance in individuals.
How fast or slow your body breaks down or metabolizes alcohol is influenced by your genes.
Studies report that genetics influences 40% to 60% risk of alcohol-related disorders.
Alcohol is broken down or metabolized by 3 main enzymes.
Any differences in these enzymes make people metabolize alcohol differently.
In fact, genetic differences in these enzymes are responsible for why different ethnic groups have higher or lower alcohol-related problems.
Higher levels of ADH enzymes and lower levels of ALDH2 enzymes can result in the build-up of acetaldehyde.
This leads to poor alcohol tolerance.
A type of the ADH gene called the ADH1B*2 (primarily found in Asian and Polynesian populations) produces the ADH1B enzyme with 100-fold activity.
This protects people with this gene variant from alcohol dependence.
The ALDH2 gene produces the ALDH2 enzyme.
A genetic mutation in the ALDH2 gene makes the gene less active or inactive.
A type of this gene called the ALDH2*2 gene has been observed in the Asian population.
This type produces the ALDH2 enzyme with 85% lower activity in the liver and inhibits voluntary consumption of alcohol by 50%.
Here's how you can still get your alcohol dependence report
Alcohol intolerance is a genetic condition in which the body prevents the effective breakdown of alcohol.
While many people do not develop any adverse reaction to consuming alcohol, some people who are alcohol intolerant may show some signs and symptoms.
When these alcohol-intolerant people consume alcohol, they experience an unpleasant phenomenon called a flush reaction.
A few common symptoms of alcohol flush reaction are:
While many people may think their alcohol tolerance is good, it is not!
One of the dangers of high alcohol tolerance is binge drinking and alcoholism.
Since people with high alcohol tolerance can consume and tolerate large amounts of alcohol, they are more likely to drink more.
With increased consumption, alcohol influences changes in the brain.
For example, you are more likely to feel happy or exhilarated when you drink.
This acts as an incentive, prompting you to drink more, eventually leading to alcoholism.
Along with alcohol tolerance, other factors that may contribute to alcoholism are:
While several factors influence alcoholism, family history is one of them.
One does not inherit it in a straightforward manner.
However, you can inherit the gene changes that increase your risk of developing alcoholism can be inherited.
So, while you may not inherit the addiction itself, you may receive the genes that increase your risk of developing alcoholism.
It has also been observed that since multiple genes play a role in alcohol use disorder, it may skip a generation.
Factors that may influence alcohol tolerance are:
While there are no tests for alcohol tolerance, genetic testing at home and a medical facility are available for alcohol intolerance.
A genetic test for alcohol intolerance involves taking a blood, saliva, or tissue sample to observe changes in the ADH and ALDH genes.
Certain gene changes that lower ADH enzyme levels and increase ALDH enzyme levels can increase your alcohol tolerance.
On the other hand, gene changes resulting in high ADH and low ALDH enzyme levels can decrease your alcohol tolerance, lowering your risk for alcohol use disorders.
A genetic test can help reveal what changes you carry in these genes and help you understand your risk for alcohol use disorders.
When it comes to preparing for an allergy test, the list of do's and don'ts can leave you feeling perplexed.
The one question that frequently arises, especially for those who rely on their daily caffeine fix, is, “Can you enjoy a steaming cup of coffee before undergoing an allergy test?”
This article delves into the surprising relationship between coffee consumption and allergy testing, shedding light on whether that cherished cup of joe could potentially impact the results.
Your genes can affect how your body processes caffeine.
There are different versions of the caffeine genes, and depending on which one you have, you may react differently to caffeine.
This is why some people can sleep by 10 PM after drinking coffee at 7 PM, and others lay awake at 2 AM despite stopping caffeine intake by 4 PM.
Learn more about your caffeine gene:
Surprisingly, the answer is no.
Before the allergy test, it is recommended to avoid coffee and other caffeinated beverages for at least 24 to 48 hours.
Caffeine can affect test results by masking symptoms, reducing immune system responses, or causing anxiety.
However, certain guidelines may vary depending on the healthcare provider or testing facility.
For reliable and precise results, following the directions provided by the healthcare professional conducting an allergy test is essential.
There are several reasons why caffeine is discouraged before an allergy test.
Let's discuss a few among them:
Also Read: How It Works: Caffeine Genetics
While caffeine takes the spotlight, It's important to remember that avoiding caffeine alone before an allergy test is not enough. Several foods and drinks are to be avoided as well.
This list includes:
It's essential to remember that avoiding coffee before an allergy test is mainly done to ensure accurate and trustworthy results.
Now that your allergy test is over, you might wonder if you can have a cup of coffee.
Relax, there's good news! In most cases, having coffee while taking a first-generation antihistamine like Benadryl is often acceptable.
However, it's best to avoid caffeine if you're taking a second-generation antihistamine like Zyrtec or Allegra.
Still, combining caffeine with antihistamines can increase the chances of side effects like feeling jittery or having trouble sleeping.
You may continue your regular activities and eating routines, including drinking coffee. But following your healthcare expert's directions is always a good idea.
Apart from caffeine and particular food and drink restrictions, there are a few general dos and don'ts to consider when preparing for an allergy test.
These tips can help improve the test's accuracy and effectiveness:
Dos:
Don'ts:
It is usually suggested to avoid consuming caffeine or other caffeinated beverages before an allergy test. Caffeine can mask symptoms, interfere with immune system reactions, and increase anxiety, affecting the accuracy of test results.
In addition to caffeine, it is essential to avoid certain foods, vegetables, herbal supplements, antihistamines, seafood, and alcohol before an allergy test.
However, once the test ends, you can usually resume your normal activities, including drinking coffee as prescribed.
Following the guidelines provided by your healthcare expert, continuing to dietary restrictions, and addressing any concerns or questions may help ensure a successful allergy test and accurate results.